Abstract
Purpose
The purpose of this study was to investigate factors which effect clinical nurses' exhaustion.
Methods
This research was conducted targeting 140 clinical nurses. Data were collected from 18 September to 30 September 2015. Data were analyzed using the program SPSS/WIN 18.0. Descriptive statistics, t-test, ANOVA, Pearson correlation coefficient, and Stepwise multiple regression analysis were used.
Results
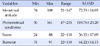
Burnout was significantly different by age (F=7.99, p=.001), marital status (t=8.69, p=.004), department area (F=7.65, p<.001), frequency of night work in a month (F=7.65, p=<.001), and clinical career (F=3.68, p=.028). There was positive correlations between menstrual attitudes of participants and premenstrual syndrome (r=34, p<.001), menstrual attitudes and stress (r=.40, p<.001), and menstrual attitudes and burnout (r=.16, p=.031). There were positive correlations between premenstrual syndrome and stress (r=.46, p<.001), between premenstrual syndrome and burnout (r=.35, p<.001), and between stress and burnout (r=.36, p<.001). Factors influencing burnout were premenstrual syndrome (β=.335) and age (β=.216), with an explanatory power of 18.0%.
Figures and Tables
Table 1
Differences in Burnout by General Characteristics of Subjects (N=131)

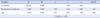
Table 2
Levels of Menstrual Attitude, Premenstrual Syndrome, Stress and Burnout (N=131)
| Variables | Min | Max | Range | M±SD |
|---|---|---|---|---|
| Menstrual attitude | 34 | 108 | 21~147 | 72.53±14.03 |
| Premenstrual syndrome | 50 | 161 | 47~235 | 119.76±23.20 |
| Stress | 24 | 88 | 22~110 | 56.35±17.09 |
| Burnout | 31 | 91 | 22~110 | 64.22±14.13 |
Summary Statement
▪ What is already known about this topic?
Burnout is significant problem for clinical nurses. Menstrual attitude and pre-menstrual syndromes can influence burnout for nurses. But there is paucity of studies on the effects of menstruation that impact clinical nurses ability to perform at the optimum.
▪ What this paper adds?
Menstrual attitude and pre-menstrual syndrome were related with stress and burnout for clinical nurses.
▪ Implications for practice, education and/or policy
Menstrual attitude and premenstrual syndrome should be thoroughly assessed with program development for reducing clinical nurses' premenstrual syndrome.
References
1. Part JM, Suh SR, Kim KY, Kim HJ. Female workers' attitudes toward menstruation, premenstrual discomfort and coping method. J Korean Soc Matern Child Health. 2012; 16(1):100–112.
2. Shin MA, Jeong MH. The relationship between premenstrual syndrome and menstrual attitudes of college students. J Korean Acad Soc Nurs Educ. 2006; 12(1):43–51.
3. Freeman EW. Premenstrual syndrome and premenstrual dysphoric disorder: Definitions and diagnosis. Psychoneuroendocrinology. 2003; 28(3):25–37.
4. Song JE, Chae HJ, Jang WH, Park YH, Lee KE, Lee SH, et al. The relationship between life style, menstrual attitude and premenstrual syndrome in nursing students. Korean J Women Health Nurs. 2013; 19(2):119–128.

5. Jeong BS, Lee C, Lee JH, Seo MK, Han OS, Kim CY. Prevalence of premenstrual syndrome and premenstrual dysphoric disorder among Korean college women. J Korean Neuropsychiatr Assoc. 2001; 40(4):551–558.
6. Jo Y, Jang K, Park S, Yun H, Noh K, Kim S, et al. Relationship between menstruation distress and coping method among 3-shift hospital nurses. Korean J Women Health Nurs. 2012; 18(3):170–179.

7. Jung GS, Oh HM, Choi IR. The influential factors on premenstrual syndrome college female students. J Korea Acad Ind Coop Soc. 2014; 15(5):3025–3036.

8. Lee WH, Kim CJ. The relationship between depression, perceived stress, fatigue and anger in clinical nurses. J Korean Acad Nurs. 2006; 36(6):925–932.

9. June KJ, Byun SW. Nurse’s burnout research throughout the past 10 years in Korea. J Korean Acad Nurs Adm. 2009; 15(3):305–313.
10. Kim JW, Lee JH, Kim DM, Lee MH. Relationship among cognitive style, perceived stress and premenstrual symptoms. J Korean Neuropsychiatr Assoc. 2002; 41(6):1099–1108.
11. Han KS, Park YH, Kim SR. The influence of stress-related personality traits, hardiness, and burnout on job satisfaction in nurse. Korean J Stress Res. 2011; 19(1):79–87.
12. Park YH, Jeong BS, Kim CY, Lee C. Prevalence of premenstrual dysphoric disorder and occupational function in a nurse group. J Korean Neuropsychiatr Assoc. 2001; 40(5):832–841.
13. Lee JW. Influences of job stress, coping, self-efficacy on burnout of clinical nurses. J Fish Mar Sci Educ. 2014; 26(5):1003–1012.

14. Yang YK. A study on burnout, emotional labor, and self-efficacy in nurses. J Korean Acad Nurs Adm. 2011; 17(4):423–431.

15. Lee Y, Choi ES. Effects of psychosocial work environment on stress, depression, sleep disorder, and burnout of general hospital nurses. Korean J Occup Health Nurs. 2015; 24(2):114–121.

16. Yang DO, Youn GH. Attitudes toward menstruation according to the increased years after menarche. Korean J Woman Psychol. 2001; 6(3):37–48.
17. Moos RH. The development of a menstrual distress questionnaire. Psychosom Med. 1968; 30(6):853–867.

18. Koh KB, Park JK, Kim CH. Development of the stress response inventory. J Korean Neuropsychiatr Assoc. 2000; 39(4):707–719.
19. Choi SM, Kang TY, Woo JM. Development and validation of a modified form of the stress response inventory for workers. J Korean Neuropsychiatr Assoc. 2006; 45(6):541–553.
21. Jang ES. A Study on the psychiatric social worker's burnout and their work environment in Korea [master's thesis]. Seoul: Soongsil University;1995. 1–61.
22. Kim JS, Lee YS. Study on fatigue, stress and burnout of pregnant nurses. Korean J Occup Health Nurs. 2013; 22(3):208–217.

23. Yang DO, Youn GH. The relationship between increased years after menarche and attitudes toward menstruation. Korean J Psychol. 2001; 6(3):37–48.
24. Oh HS, Koh CK. The mediating effect of mindfulness in the relationship between emotional intelligence and stress among clinical nurses. Korean J Stress Res. 2014; 22(3):139–147.

25. Park CS. Factors influencing on burnout experience in working nurses at hospital. Korean J Women Health Nurs. 2002; 8(4):550–558.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download