Abstract
Purpose
The purpose of this study was to identify relationships of periodontal disease and health related quality of life (HRQoL) in pregnant women.
Methods
The participants in this study were 129 pregnant women. Data were collected using questionnaires of characteristics of the participants and subjective perception of periodontal disease and a dentist's assessment of periodontal disease. Data were analyzed using descriptive statistics, correlation, and hierarchical multiple regression.
Results
The physical QoL showed significant negative correlation with subjective perception of periodontal disease (r=-.21, p=.013). Mental QoL had significant negative correlations with subjective perception of periodontal disease (r=-.32, p<.001) and objective periodontal disease (r=-.34, p<.001). Hierarchical multiple regression analyses revealed that pregnant women who had a history of abortion and had higher subjective perception of periodontal disease tended to report lower levels of physical QoL. Pregnant women whose age are between 30-34 years and higher subjective perception and objective periodontal disease tended to report lower mental QoL.
Figures and Tables
Table 1
Differences in Health related Quality of Life according to Socio-demographic and Obstetric Characteristics and Periodontal Disease (N=129)

Table 2
Relationships among Socio-demographic, Periodontal Disease and Health related to Quality of Life (N=129)
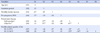
Table 3
Unique Contribution of Periodontal Disease in Explaining Physical Component of Quality of Life in Pregnant Women (N=129)
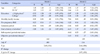
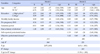
Table 4
Unique Contribution of Periodontal Disease in Explaining Mental Component of Quality of Life in Pregnant Women (N=129)
Summary Statement
▪ What is already known about this topic?
Periodontal disease is a common oral infection in pregnant women with high prevalence ranging from 50~75%.
▪ What this paper adds?
This study showed high risk of periodontal disease among pregnant women, reporting 40.3% of gingivitis and 37.2% of periodontitis, which also related to quality of life in pregnant women.
▪ Implications for practice, education and/or policy
Since oral health care is highly related to periodontal disease and quality of life in pregnant women, intensive screening for oral health problems in pregnant women should be considered as routine perinatal care and nationwide advertisement of the important of oral hygiene during pregnancy is essential.
References
1. Kushnir D, Zusman SP, Robinson PG. Validation of a Hebrew version of the oral health impact profile-14. J Public Health Dent. 2004; 64(2):71–75.
2. Saletu A, Pirker-Frühauf H, Saletu F, Linzmayer L, Anderer P, Matejka M. Controlled clinical and psychometric studies on the relation between periodontitis and depressive mood. J Clin Periodontol. 2005; 32(12):1219–1225.

3. Centers for Disease Control and Prevention. Periodontal disease [Internet]. Atlanta: Author;2014. cited 2016 May 25. Available from: http://www.cdc.gov/OralHealth/periodontal_disease/.
4. Choi ES, Lyu JY, Kim HY. Association between oral health status and health related quality of life. J Dent Hyg Sci. 2015; 15(4):480–487.
5. Ha JE, Yeo BM, Roh HY, Paik DI, Bae KH. Periodontal condition and pathogens distribution of pregnant women. J Korean Acad Oral Health. 2010; 34(4):587–594.
6. Hong NP, Nam YY. All kinds of learning of oral cavity. Seoul: Kidari;2000.
7. Vogt M, Sallum AW, Cecatti JG, Morais SS. Periodontal disease and some adverse perinatal outcomes in a cohort of low risk pregnant women. Reprod Health. 2010; 7:29.

8. Calvert MJ, Freemantle N. Use of health-related quality of life in prescribing research. part 1: Why evaluate health related quality of life? J Clin Pharm Ther. 2003; 28(6):513–521.
9. Lau Y, Yin L. Maternal, obstetric variables, perceived stress and health-related quality of life among pregnant women in Macao, China. Midwifery. 2011; 27(5):668–673.

10. Lacasse A, Bérard A. Validation of the nausea and vomiting of pregnancy specific health related quality of life questionnaire. Health Qual Life Outcomes. 2008; 6:32.

11. Amador N, Juárez JM, Guízar JM, Linares B. Quality of life in obese pregnant women: A longitudinal study. Am J Obstet Gynecol. 2008; 198(2):203.e1–203.e5.

12. Zahedi M, Deris F. The quality of life in pregnant women in Farokhshahr city, 2012. J Clin Nurs Midwifery. 2014; 3(3):63–69.
13. Safarzadeh A, Boryri T, Khojasteh F, NavvabiRigi SD. Evaluation of quality of life and pregnancy outcome in overweight pregnant women in Zahedan. J Pain Relief. 2013; 2(3):124–129.

14. Abbaszadeh F, Baghery A, Mehran N. Quality of life among pregnant women. J Hayat. 2009; 15(1):41–48.
15. Ramirez-Velez R. Pregnancy and health-related quality of life: A cross sectional study. Colomb Med. 2011; 42(4):476–481.
16. Couto ER, Couto E, Vian B, Gregorio Z, Nomura ML, Zaccaria R, et al. Quality of life, depression and anxiety among pregnant women with previous adverse pregnancy outcomes. Sao Paulo Med J. 2009; 127(4):185–189.

17. Kim YH, Lee JH. A study on the OHIP-14 of some local women impact on the EQ-5D for review. J Korean Acad Oral Health. 2015; 39(3):180–185.

18. Quandt SA, Hiott AE, Grzywacz JG, Davis SW, Arcury TA. Oral health and quality of life of migrant and seasonal farmworkers in North Carolina. J Agric Saf Health. 2007; 13(1):45–55.
19. Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates;1988.
20. Park HJ, Lee HJ, Cho SH. Influences of oral health behaviors, depression and stress on periodontal disease in pregnant women. J Korean Acad Nurs. 2016; 46(5):653–662.

21. Jin HJ, Bae KH, Kim JB, Park DY, Jeong SH, Kim BI, et al. Validity and reliability of a questionnaire for evaluating periodontal disease. J Korean Acad Oral Health. 2014; 38(3):170–175.

22. Kim BO, Kim SO, Kim OJ, Sim HS, Lee CS, Han OG, et al. Periodontology. Seoul: Dahan Narae;2005.
23. Ware J Jr, Kosinski M, Keller SD. A 12-item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med Care. 1996; 34(3):220–233.
24. Kim HY, Jung YY. Effects of antenatal depression and antenatal characteristics of pregnant women on birth outcomes: A prospective cohort study. J Korean Acad Nurs. 2012; 42(4):477–485.

25. Kim HW. Development of the pregnancy nutrition knowledge scale and its relationship with eating habits in pregnant women visiting community health center. J Korean Acad Nurs. 2009; 39(1):33–43.

26. Chang SR, Chen KH, Lin MI, Lin HH, Huang LH, Lin WA. A repeated measures study of changes in health-related quality of life during pregnancy and the relationship with obstetric factors. J Adv Nurs. 2014; 70(10):2245–2256.

27. Xiong X, Elkind-Hirsch KE, Vastardis S, Delarosa RL, Pridjian G, Buekens P. Periodontal disease is associated with gestational diabetes mellitus: A case-control study. J Periodontol. 2009; 80(11):1742–1749.

28. Geisinger ML, Robinson M, Kaur M, Gerlach RW, Griffin R, Geurs NC, et al. Individualized oral health education improves oral hygiene compliance and clinical outcomes in pregnant women with gingivitis. J Oral Hyg Health. 2013; 1(2):1–9.
29. Da Costa D, Dritsa M, Verreault N, Balaa C, Kudzman J, Khalifé S. Sleep problems and depressed mood negatively impact health-related quality of life during pregnancy. Arch Womens Ment Health. 2010; 13(3):249–257.

30. Marino R, Schofield M, Wright C, Calache H, Minichiello V. Self-reported and clinically determined oral health status predictors for quality of life in dentate older migrant adults. Community Dent Oral Epidemiol. 2008; 36(1):85–94.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download