Abstract
Purpose
The purpose of this descriptive study was to assess levels of stress, coping style, and nursing needs for hospitalized pregnant women diagnosed with preterm labor.
Methods
Data were collected from 125 pregnant women aged between 20 and 40 years and diagnosed with preterm labor by OBGY units at 3 hospitals. Data were analyzed by frequency, percentage, t-test, and ANOVA with Scheffé test.
Results
The level of stress among women was an average of 2.13 out of 4 points, the level of coping style was an average of 2.66, and nursing needs was an average of 2.83 out of 4 points. The level of stress was significantly different by job, length of hospital stay, type of hospital, and history of admission at obstetric unit. The level of coping style was significantly different by age and monthly income. The level of nursing needs was significantly different by type of hospital. Higher level of stress and coping style were related to higher level of nursing needs. There was no significant correlation between stress and coping style.
Conclusion
The result showed the importance of nursing intervention dealing with stress, coping style and nursing needs for women with preterm labor. Nurses need to provide nursing interventions to reduce the stress, to strengthen the coping style, and to satisfy the nursing needs for pregnant women hospitalized due to preterm labor.
Figures and Tables
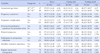
Table 1
General and Obstetric Characteristics of Participants (N=125)

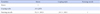
Table 2
Level of Stress, Coping Style and Nursing Needs (N=125)

Table 3
Differences in Stress, Coping Style and Nursing Needs by General Characteristics of Participants (N=125)

Table 4
Differences in Stress, Coping Style and Nursing Needs by Obstetric Characteristics of Participants (N=125)
Summary Statement
▪ What is already known about this topic?
Women's level of stress precipitates preterm labor and precedes the admission to the hospital for preterm labor. Coping style can affect the level of stress, and level of stress is associated with nursing needs. But the relationships among these variables are inconsistent in previous studies.
▪ What this paper adds?
This study found that higher levels of stress and coping style were related to higher levels of nursing needs.
▪ Implications for practice, education and/or policy
The result of the study shows the importance of nursing intervention to help hospitalized pregnant women due to preterm labor to reduce the stress and strengthen the coping style. In order to satisfy the nursing needs for pregnant women hospitalized for preterm labor, many efforts need to be made to manage their stress and strengthen their coping style.
References
1. Statistics Korea. 2013 infant mortality rate for Korea [Internet]. Seoul: Statistics Korea;2013. 2014 September 30. Available from: http://kostat.go.kr/portal/korea/kor_nw/3/index.board?bmode=read&aSeq=269012.
2. Lee NH. Ways to improve prenatal care in a low-fertility Korea. Health Welf Policy Forum. 2014; 217:64–74.
3. Cunningham FG, Gant NR, Leveno KJ, Gilstrap LC, Hauth JC, Wenstrom KD. Williams Obstetrics. 23rd ed. New York: Mc-Graw-Hill;2010.
4. McParland P, Jones G, Taylor D. Preterm labour and prematurity. Obstet Gynaecol Reprod Med. 2004; 14(5):309–319.

5. Ghorbani M, Dolatian M, Shams J, Alavi-Majd H, Tavakolian S. Factors associated with posttraumatic stress disorder and its coping styles in parents of preterm and full-term infants. Glob J Health Sci. 2014; 6(3):65–73.

6. Maloni JA. Lack of evidence for prescription of antepartum bed rest. Expert Rev Obstet Gynecol. 2011; 6(4):385–393.

7. Thornburg P. "Waiting" as experienced by women hospitalized during the antepartum period. MCN Am J Matern Child Nurs. 2002; 27(4):245–248.

8. Ryu KH, Shin HS. Phenomenological study on experience of preterm Labor. Korean J Women Health Nurs. 2009; 15(2):140–149.

9. Figueiredo B, Costa R. Mother's stress, mood and emotional involvement with the infant: 3 months before and 3 months after childbirth. Arch Womens Ment Health. 2009; 12(3):143–153.
10. Yonkers KA, Smith MV, Forray A, Epperson CN, Costello D, Lin H, et al. Pregnant women with posttraumatic stress disorder and risk of preterm birth. JAMA Psychiatry. 2014; 71(8):897–904.

11. Mackey MC, Boyle JS. An explanatory model of preterm labor. J Transcult Nurs. 2000; 11(4):254–263.

12. Silver RM, Varner MW, Reddy U, Goldenberg R, Pinar H, Conway D, et al. Work-up of stillbirth: A review of the evidence. Am J Obstet Gynecol. 2007; 196(5):433–444.

13. Schore AN. Effects of a secure attachment relationship on right brain development affect regulation, and infant mental health. Infant Ment Health J. 2001; 22(1-2):7–66.

14. Kim HK. Stress and coping style of women with preterm labor [master's thesis]. Seoul: Seoul National University;2003.
15. Lazarus RS, Folkman S. Stress, appraisal and coping. New York: Spring Publishing Company;1984.
16. Youn IS. A study on emotions, feelings of discomfort, and nursing needs of the women in the possibility of abortion: Centered on the threatened abortion and habitual abortion during hospitalization. J Korean Acad Womens Health Nurs. 1995; 1(1):119–137.
17. Lee PS, Yoo EK. A study on the physical and emotional status, and nursing needs of the pregnant women hospitalized by premature labor. J Korean Acad Womens Health Nurs. 1996; 2(1):76–91.
18. Rines AR, Montag MI. Nursing concept and nursing care. New York: A Wiley Biomedical Publication;1976.
19. Kim MK, Lee YW, Cho IS, Lim JY. Change of stress and nursing needs after hospitalization in preterm labor women. Korean J Women Health Nurs. 2009; 15(1):24–31.

20. So HS, Cho BH, Hong MS. Analysis of nursing studies of coping conducted in Korea from 1978 to 1995. J Nurs Acad Soc. 1996; 26(3):709–729.

21. Wilson-Barnett J, Carrigy A. Factors influencing patients emotional reactions to hospitalization. J Adv Nurs. 1978; 3(3):221–229.

22. Billings AG, Moos RH. The role of coping responses and social resources in attenuating the stress of life events. J Behav Med. 1981; 4(2):139–157.

23. Doyle NM, Monga M, Kerr M, Hollier LM. Maternal stressors during prolonged antepartum hospitalization following transfer for maternal-fetal indications. Am J Perinatol. 2004; 21(1):27–31.

24. Shim CS, Lee YS. Effects of a yoga-focused prenatal program on stress, anxiety, self confidence and labor pain in pregnant women with in vitro fertilization treatment. J Korean Acad Nurs. 2012; 42(3):369–376.

25. Yu WJ, Song JE. Effects of abdominal breathing on state anxiety, stress, and tocolytic dosage for pregnant women in preterm labor. J Korean Acad Nurs. 2010; 40(3):442–452.

26. Chung SH. A study of the effectiveness of policies in response to low fertility. Korea J Popul Stud. 2012; 35(1):31–52.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download