Abstract
Purpose
The purpose of this study was to investigate the effect of dehydration from preoperative fasting on postoperative nausea and vomiting in patients who underwent gynecologic surgeries.
Methods
Study design was a prospective descriptive study. A total of 75 patients in a university hospital were selected. Data were collected from March 17 to May 16, 2014 using self-report questionnaires and clinical electronic chart.
Results
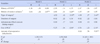
Factors influencing the development of postoperative nausea and vomiting were type of surgery (t=3.44, p=.001), use of PCA (t=-2.16, p=.034), and preoperative dehydration level (t=5.93, p<.001), and these variables accounted for 51.7% of postoperative nausea and vomiting. Among these variables, preoperative dehydration amount (β=.56) showed the largest influence in the difference in postoperative nausea and vomiting.
Conclusion
Reducing dehydration during preoperative fasting can prevent occurrence of postoperative nausea and vomiting. Development of a clinical guideline is necessary to give directions for the prevention of dehydration during preoperative fasting and to ensure the proper duration of fasting according to patient characteristics, type of surgery and time of surgery.
Figures and Tables
Table 1
Level of Dehydration during Preoperative Fasting and INVR score during Postoperative 24 hour Period (N=75)
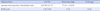
| Characteristics | M±SD | Measuring range | Tool range |
|---|---|---|---|
| Amount of preoperative dehydration (mL) | 610.58±217.97 | 97.00~1,118.00 | - |
| INVR score | 7.35±5.65 | 0~25 | 0~32 |
Table 2
Difference in Postoperative Nausea and Vomiting according to General Characteristics (N=75)
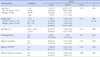
Table 3
Difference in Postoperative Nausea and Vomiting according to Anesthetic and Surgical related Characteristics (N=75)
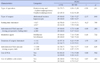
Table 4
Factors associated Postoperative Nausea and Vomiting in Gynecologic Surgery (N=75)
Summary Statement
▪ What is already known about this topic?
Preoperative fasting is prerequisite for all patients who are undergoing surgeries, but it is related to postoperative nausea and vomiting. Dehydration may affect postoperative nausea and vomiting.
▪ What this paper adds?
Our research identified that the amountof dehydration from preoperative fasting is the most significant factor that affects the extent of postoperative nausea and vomiting.
▪ Implications for practice, education and/or policy
This study shows preoperative fasting causes postoperative nausea and vomiting. Time of midnight should be reorganized into new timing system for patients who undergo a surgery in different time period.
References
1. Sendelbach S. Preoperative fasting doesn't mean nothing after midnight. Am J Nurs. 2010; 110(9):64–65.

2. Lee JH, Oh AY, Kim SD. Effect of preoperative NPO and oral fluid on gastric fluid volume and pH. Korean J Anesthesiol. 1999; 36(3):377–386.
3. Somwanshi M, Tripathi A, Singh B, Bajaj P. Effect of preoperative oral fluids on gastric volume and pH in postpartum patients. Middle East J Anaesthesiol. 1995; 13(2):197–203.
4. American Society of Anesthesiologist. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: A report by the American Society of Anesthesiologist task force on preoperative fasting. Anesthesiology. 1999; 90(3):896–905.
5. Tudor G. Fasting: how long is too long. Aust Nurs J. 2006; 13(7):29–31.
6. Adanir T, Aksun M, Ozqurbuz U, Altin F, Sencan A. Does preoperative hydration affect postoperative nausea and vomiting? A randomised controlled trial. J Laparoendosc Adv Surg Tech A. 2008; 18(1):1–4.
7. Lambert KG, Wakim JH, Lambert NE. Preoperative fluid bolus and reduction of postoperative nausea and vomiting in patients undergoing laparoscopic gynecologic surgery. AANA J. 2009; 77(2):110–114.
8. Läer S, Scholz J, Ritterbach C, Laer C, Rahme E, Schulte AM, Esch J. Association between increased 5-HIAA plasma concentrations and postoperative nausea and vomiting in patients undergoing general anaesthesia for surgery. Eur J Anaesthesiol. 2001; 18(12):833–835.

9. McCracken G, Houston P, Lefebvre G. Society of obstetricians and gynaecologists of canada clinical practice guideline: Guideline for the management of postoperative nausea and vomiting. J Obstet Gynaecol Can. 2008; 30(7):600–607.
10. Ho KY, Chiu JW. Multimodal antiemetic therapy and emetic risk profiling. Ann Acad Med Singap. 2005; 34(2):196–205.
11. Stadler M, Bardiau F, Seidel L, Albert A, Boogaerts JG. Difference in risk factors for postoperative nausea and vomiting. Anesthesiology. 2003; 98(1):46–52.

12. Choi DH, Ko JS, Ahn HJ, Kim JA. A korea predictive model for postoperative nausea and vomiting. J Korean Med Sci. 2005; 20(5):811–815.
13. Magner JJ, McCaul C, Carton E, Gardiner J, Buggy D. Effect of intraoperative intravenous crystalloid infusion on postoperative nausea and vomiting after gynaecological laparoscopy: Comparison of 30 and 10 mL. kg-1. Br J Anaesth. 2004; 93(3):381–385.
14. Antor MA, Uribe AA, Erminy-Falcon N, Werner JG, Candiotti KA, Pergolizzi JV, et al. The effect of transdermal scopolamine for the prevention of postoperative nausea and vomiting. Front Pharmacol. 2014; 5(55):1–8.

15. Chun HR, Jeon IS, Park SY, Lee SJ, Kang SH, Kim SI. Efficacy of palonosetron for the prevention of postoperative nausea and vomiting: A randomized, double-blinded, placebo-controlled trial. Br J Anaesth. 2014; 112(3):485–490.

16. Anderson LA, Gross JB. Aromatherapy with peppermint, isopropyl alcohol, or placebo is equally effective in relieving postoperative nausea. J Perianesth Nurs. 2004; 19(1):29–35.

17. Ferruggiari L, Ragione B, Rich ER, Lock K. The effect of aromatherapy on postoperative nausea in women undergoing surgical procedures. J Perianesth Nurs. 2012; 27(4):246–251.

18. Xu M, Zhou SJ, Jiang CC, Wu Y, Shi WL, Gu HH, et al. The effects of P6 electrical acustimulation on postoperative nausea and vomiting in patients after infratentorial craniotomy. J Neurosurg Anesthesiol. 2012; 24(4):312–316.

19. Ali SZ, Taguchi A, Holtmann B, Kurz A. Effect of supplemental pre-operative fluid on postoperative nausea and vomiting. Anaesthesia. 2003; 58(8):780–784.

20. Park SI, Ko YK, Yoon HS, Yoon SH, Lee WH, Lee JU. Analysis of factors related to postoperative nausea and vomiting after laparoscopic hysterectomy. Korean J Anesthesiol. 2005; 49(2):210–215.

21. Moon HY. Palonosetron and aprepitant for prevention of postoperative nausea and vomiting in patient undergoing laparoscopic gynecology surgery [master's thesis]. Seoul: Chung-Ang University;2014.
22. Jung HJ, Park SY. Combination effects of capsicum plaster at the korean hand acupuncture points K-d2 with prophylactic antiemetic on postoperative nausea and vomiting after gynecologic laparoscopy. J Korean Acad Nurs. 2013; 43(2):215–224.

23. Choi YK, Kim HJ, Park SW, Kim KS. The optimal anti-emetic dose of Ramosetron for prevention of postoperative nausea and vomiting following gynecologic surgery. Korean J Anesthesiol. 2008; 54(5):538–543.
24. Aitkenhead AR, Moppett IK, Thompson JP, editors. Smith & Aitkenhead's Textbook of Anaesthesia. 6th ed. London, UK: Churchill Livingstone;2014.
25. Rhodes VA, McDaniel RW. The index of nausea, vomiting, and retching: A new format of the index of nausea and vomiting. Oncol Nurs Forum. 1999; 26(5):889–894.
26. Kim YJ, Kim JY, Choi IR, Kim MW, Rhodes V. The index of nausea, vomiting, and retching Korean translation. J Korean Acad Adult Nurs. 2000; 12(2):278–285.
27. Lee YY. Prediction model on causing factors for the postoperative nausea and vomiting in patients using patient controlled analgesia [dissertation]. Seoul: Chung-Ang University;2006.
28. Song JW, Shim JK, Song Y, Yang SY, Park SJ, Kwak YL. Effect of ketamine as an adjunct to intravenous patient-controlled analgesia, in patients at high risk of postoperative nausea and vomiting undergoing lumbar spinal surgery. Br J Anaesth. 2013; 111(4):630–635.

29. Wang PK, Tsay PJ, Huang CC, Lai HY, Lin PC, Huang SJ, et al. Comparison of dexamethasone with ondansetron or haloperidol for prevention of patient-controlled analgesia-related postoperative nausea and vomiting: A randomized clinical trial. World J Surg. 2012; 36(4):775–781.

30. Yun JS. Effects of amounts of intraoperative intravenous fluid administration on postoperative nausea and vomiting [master's thesis]. Daejeon: Chungnam National University;2007.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download