Abstract
Purpose
This study aimed to evaluate the impact of a lifestyle modification program on menstrual irregularity among overweight and obese women with polycystic ovarian syndrome.
Methods
A quasi experimental research design was used to conduct this study on 82 women with polycystic ovarian syndrome at the Gynecology and Obesity clinics of Mansoura University Hospital, Egypt. Two groups were included; the study group received a lifestyle modification program for 48 weeks, while the control group was not subjected to this program. Data collection was done for the following variables, a structured interview questionnaire was used to assess the women's general characteristics, menstrual patterns, and 24-hour dietary recall and the researcher took anthropometric measurements and assessed hirsutism by the Ferriman-Gallwey scale.
Results
After one year of lifestyle modification, the number of menstrual cycles significantly increased from 2.7±1.6 to 6.9±1.5 (t=12.26, p<.001) in the study group compared to insignificant minor changes among the control group (t=0.69, p=.488). Additionally, 58.5% were menstruating regularly compared to none in the control group (χ2=33.93, p<.001).
Polycystic ovarian syndrome (PCOS) is one of the most common endocrine disorders; it affects 5~10% of women at reproductive age worldwide[1]. In Egypt, PCOS shows as up to 26% of familial PCOS and 5.4% of women do not have a familial history[2]. Its hallmarks are biochemical and/or clinical hyperandrogenism in addition to chronic anovulation with subsequent menstrual disturbances such as oligo/amenorrhea[3].
Obesity, especially the truncal type, affects 17.2% of Egyptian PCOS women[2]. It adversely influences the degree of associated insulin resistance, which in turn affects the androgen level; therefore, resulting in menstrual irregularity and hirsutism[4]. A previous study concluded that severe caloric restriction for weight reduction is associated with restoration of menstrual cycles[5]. However, long-term severe caloric restriction resulting in rapid weight loss, can lead to poor patient compliance; accordingly, the body gains its baseline weight within one year[6].
The increasing rates of obesity, among Egyptian population, are largely attributed to their lifestyles; including unhealthy dietary habits, like consuming the widely distributed junk, fast food coupled with increasing sedentary lifestyles, seen in such reports that 63% of the Egyptian population at the age of twenty or more have sedentary lifestyles[7].
Recently, large studies investigated the impact of the lifestyle modification in PCOS women and suggested that modest weight loss, even as little as 5% from baseline body weight can positively affect hyperinsulinemia. As a result, it causes a decrease of androgens and normalization of menstrual cycles. Evidence supports the role of the healthcare providers in encouraging women with menstrual irregularities to change their lifestyle[89]. PCOS has always been considered as a systemic problem that carries many risks at the time of presentation and later in a woman's life. For example, infrequent menstrual flow carries 3-fold increased risks of endometrial hyperplasia and endometrial carcinoma[10]. This stimulates the current study to evaluate the impact of a lifestyle modification program on menstrual irregularity among overweight or obese women with PCOS, where Egyptian studies which investigated this topic are so limited.
This was designed as a quasi-experimental study. It was conducted at the obesity outpatient clinic of Rheumatology department in collaboration with the gynecology outpatient clinic of Obstetrics and Gynecology department at Mansoura University Hospitals, Egypt.
A convenience sample of single women who had attended the study settings from January to August 2012, were eligible to participate in this study when they fulfilled the following criteria: 1) diagnosed with PCOS based on the presence of menstrual cycle disturbances after ≥2 years of menarche; either in the form of oligomenorrhea (i.e. fewer than six menstrual cycles during the previous year), or amenorrhea (i.e. no menstruation for ≥6 months), and features of androgen excess such as hirsutism and acne (hirsutism based on the Ferriman-Gallwey score ≥8 after two weeks of omitting management of excessive hair)[11], 2) overweight or obese women (i.e. with a BMI of 25.0~29.9 or≥30.0 respectively)[12], and 3) free from any serious medical disease requiring medical supervision and not on medical treatment known to cause menstrual disturbances.
This study was comprised of a total sample of 82 clients based on visiting the study setting during the assigned study period. Each eligible client was given equal opportunity to join either study or control group. Accordingly, the study group comprised a total number of 41 clients and similarly the control group. During the study period, five women dropped from the study group because they did not comply with the minimum number of follow-up interviews (n=10), and three were lost from the control group; two of them did not comply with the minimum number of follow-up interviews, while one was lost due to marriage, and all were replaced with the next potential candidates. The flowchart of the studied sample is presented in Figure 1.
A structured questionnaire was developed by the researchers to assess the general characteristics of the participants. The 1st section consisted of eight items on age, residence, education, and lifestyle habits (e.g., number of meals per day, components of meals, duration and form of exercise, duration of watching television per day). Menstrual Patterns
This section included the menstrual history such as age of menarche, cycle length, duration of menstrual blood flow, and number and rhythm of menstrual cycles through the previous year. All the items of this section were self-reported by the clients.
Body weight, waist circumference, and BMI were measured by the nurse researcher. Body weight was obtained using the same weighting scale and recorded to the nearest 0.1 kg, height was measured with a fixed stadiometer and recorded to the nearest 0.5 cm; while participants in bare feet, and waist circumference was measured during expiration according to the National Health and Nutrition Examination Survey anthropometric manual[13] and recorded in centimeters to the nearest 0.1 cm.
The Ferriman-Gallwey scale[11] is a valid universal scoring system that was used to evaluate the degree of hair growth in nine key anatomic areas (i.e. lips, chin, hands and legs, breasts, abdomen, pubic area, lower and upper back). The degree of hirsutism of each area was scored using a 4-grade scale ranged from 0 to 4, where 0 represents no hair growth and 4 means a maximum hair growth. For each respondent the scores of the nine areas were summed up to obtain the Ferriman-Gallwey Hirsutism total score. From a maximum possible score of 36, a score of≥8 indicates androgen excess[11] and this was an inclusion criteria, as well as outcome variable. To maintain reliability of the collected data, hirsutism score was assessed only by the nurse investigator. This assessment was performed in a separate room and the client's privacy was strictly maintained.
A 24-hour dietary recall was used to describe the food and drink intake. It is a standardized design consisting of 3 items on a single sheet (i.e., time, quantity, and type of intake)[14]. It is a valid clinical tool filled in by every participant daily for the week preceding the clinic visit to be checked by the investigators on the interview day. Examples of type of food and drink include: At 7 am, 1/4 slice of brown bread, 5 spoons of light cheese, and a cup of tea with one spoon of sugar were consumed. At 2 pm, a chicken chest, 5 spoons green salad, two spoons of rice, and a glass of orange juice. At 7 pm, one cup of yoghurt and two apples.
The lifestyle modification program was designed as a comprehensive approach based on counseling the subjects about energy-restricted diet, eating behaviors, and physical activity. Energy-restricted diet depends on reducing the total caloric needs/day by 500 calories. The total caloric needs per day were calculated for every participant by means of the Harris-Benedict equation based on her activity level[15]. For the study group subjects, the daily caloric needs ranged from 1200~1800 calories that was divided on small frequent meals with 10~15% from proteins, 30~35% from fat and 55% from carbohydrates of low glycemic index[16].
Along with the energy-restricted diet, healthy balanced diet was recommended by asking the participants to consume 4~5 servings of fresh vegetables and fruits, whole grains, food rich with fibers content, daily drink a minimum of 1.5 liter of water and take a daily multivitamin supplement as ordered by the dietitian. Conversely, they were instructed to decrease food rich with saturated fats (e.g., meats, fried food), and fast food and caffeine were discouraged as a part of the healthy diet plan.
Additionally, participants were instructed on modifying their eating behaviors (e.g. avoid eating during the times of watching television, or immediately before bedtime, avoid drinking through/immediately after meals; rather drink before meals time). Moreover, at least 150 minutes of moderate-intensity activity or 75 minutes of vigorous-intensity activity per week were recommended[1718]. The lifestyle modification program contents were prepared by the research team and revised by an interdisciplinary team of dietitian, exercise physiologist and a specialist of maternity and gynecology nursing before providing it to the participants.
The process of this research was carried out via three phases; initial assessment, implementation of the program, follows up visits, and outcomes evaluation.
At the baseline and before the group assignment, gynecologic history was obtained to ensure women eligibility for participation; thereafter the aim and approach of this research were explained to the clients in order to get their informed consent. Full general and clinical assessment for anthropometrics was performed by the nurse investigator, the hirsutism score was assessed; menstrual history which describes the menstrual cycle characteristics during the year preceding enrollment was obtained and recorded as baseline data.
A lifestyle modifications program was provided to the study group through two educational sessions in small groups (n=3~5) on two consecutive days at the Obesity Clinic with duration of approximately 45~60 minutes for each session. PCOS definition, symptoms, and complications, in addition to the importance of weight reduction were discussed during the 1st session, while the 2nd session concerned with the permitted, forbidden food, eating behaviors, and different forms of physical activity. Both sessions were presented in a power point presentation by the nurse researcher. The study group was provided with an instructional brochure to be used as a guide for the permitted and forbidden foods and behaviors. They were asked to accurately record their dietary intake daily for the week preceding the assigned clinic visit; using a 24-hour dietary recall.
Initially for the 1st two months of enrollment, participants were followed through biweekly face-to-face interview that the nurse investigator went along with a registered dietitian at the obesity clinic to monitor the participant's compliance with the lifestyle modification program. Then, they moved on monthly face-to-face interviews, giving a total number of fifteen face-to-face individual interviews by end of the study, including the initial interview. A telephone conversation with a pre assigned researcher was made to the client who found a difficulty in attending one or two biweekly/monthly interview. Attending the two educational sessions and a minimum number of ten follows up face-to-face/telephone interviews was considered as sufficient participation to stay in the study.
Each interview took about 10~15 minutes. During this interview the investigators had to monitor the participant's compliance with the program by way of reviewing the 24-hours dietary recalls for the one week preceding the assigned interview. As well as, inquiring the clients verbally about the type and duration of performed exercise and their eating behavior during the same period. All the outcome measures including, anthropometric measures, menstrual history, and the hirsutism score were recorded at the initial assessment and were recorded again after one year of enrollment.
This study was approved by the Ethics Committee in Faculty of Nursing and Faculty of Medicine, Mansoura University, Egypt. Informed consent was obtained from each participant after clarifying the study aim and approach. Participants were assured about the confidentiality of their data as well they were informed that they have the right to withdraw at any time. Additionally, at the end of the study, clients who had been allocated to the control group were invited to be involved in the same lifestyle modification program, but separate from the intervention group, so that they were not disadvantaged.
All statistical analyses were performed using SPSS for windows version 17.0 (SPSS, Chicago, IL). Continuous data were obtained at baseline and after 12 months follow-up period were expressed as M±SD and compared pre- and post-test scores in each group using paired t test. Categorical data were expressed in numbers and percent and compared using the χ2 test. The 95% confidence intervals (CI) for the difference in means were calculated. Statistical significance was set at p<.05.
Table 1 reveals that the general characteristics of the two groups were similar at the baseline (p>0.05). BMI for the study and control groups were almost identical (33.1±1.6 and 33.4±1.9 respectively; t=0.77, p=.442). Most of the study and control groups (90.2% and 92.7% respectively) were obese, while the minorities (9.8% and 7.3% respectively) were overweight. Mean number of menstrual cycles was almost similar for the study and control groups (2.7±1.6 and 2.5±1.3 respectively; χ2=0.62, p=.536). Around two thirds of the study and control groups (68.3% and 65.9% respectively) were oligomenorrhea. Differences observed between the two groups for waist circumference and hirsutism score were not statistically significant (t=0.27, p=.785; and t=1.03, p=.305 respectively).
Table 2 shows that after one year of lifestyle modification, mean weight for the study group significantly decreased by 7.4 kg reflecting a reduction of 8.7% from the baseline value (t=5.27 & p<.001), compared to insignificant reduction in the control group by 2.5 kg reflecting a weight loss of 2.9% at end of the study (t=1.55, p=.125). Similarly, among the study group BMI decreased by 2.89 (t=7.45, p<.001), and waist circumference decreased by 8.3 cm at the end of the study (t=3.48, p=.001). On contrary, the changes reported in the control group were insignificant. Moreover, while the hirsutism score was similar in the two groups at baseline, after one year of lifestyle modification the hirsutism score was significantly reduced in the study group by 4.2 (t=3.65, p<.001) compared to insignificant decrease by 0.6 in the control group (t=0.51, p=.609).
Figure 2 illustrates that the number of the menstrual cycles among the two groups did not differ significantly at baseline. It was significantly increased by 4.2 points from 2.7±1.6 at baseline to 6.9±1.5 after one year of lifestyle modification program in the study group (t=12.26, p<.001), compared to insignificant change in the control group (t=0.69, p=.488).
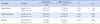
Table 3 shows that no subjects in both groups had regular menses at baseline. After one year of lifestyle modification, 24 women (58.5%) in the study group were menstruating regularly compared to none in the control group. Among the study group, women who were amenorrhea and oligomenorrhea (31.7% and 68.3% respectively) was approximately halved at one year (12.2% and 29.3% respectively) with statistically significant differences (χ2=4.56, p=.033 for amenorrhea; χ2=12.49, p<.001 for oligomenorrhea), in contrast to the control group, which showed insignificant minor changes.
The present study aimed to evaluate the impact of a lifestyle modification program on menstrual irregularity among overweight or obese women with PCOS. This aim was achieved through the present study finding which revealed a significant decrease in menstrual cycle irregularities among the study group after one year of lifestyle modification. Accordingly, the study hypothesis was confirmed, "overweight or obese women with PCOS who participate in a lifestyle modification program experience less menstrual irregularity than those who do not participate."
This study finding is consistent with previous studies that investigated the impact of lifestyle modification on managing PCOS symptoms among adult women. Such studies concluded that lifestyle modification results in weight loss with subsequent improvement of menstrual cycle irregularities and androgen excess[19202122].
The present study showed that among the study group with 8.7% weight reduction from the baseline value, frequency of amenorrhea and oligomenorrhea was significantly decreased and led more than half of the participants to have regular menstruation after one year of lifestyle modification compared to none at baseline. Similar to the present study, a previous study had analyzed the impact of a comprehensive lifestyle modification program on menstrual irregularities among 59 obese German girls with PCOS. After one year of lifestyle modification the authors dichotomized the studied group into successful weight loss group (n=26) and unsuccessful weight loss group (n=33) and reported a significant decrease in the prevalence of amenorrhea and oligomenorrhea from baseline (by 42% and 19%, respectively) among the successful weight loss group compared to insignificant decrease (by 6% and 3% respectively) among the unsuccessful weight loss group [23].
Also, Hoeger et al.[24] conducted a clinical trial in New York; over one year, to study the effect of intensive lifestyle intervention and/or metformin on menstrual events among 38 overweight or obese women with PCOS. They found a significant restoration of ovulation and menstrual events only when the lifestyle modifications were implemented along with the medical treatment.
Such agreement between the present study findings and the findings of the previously described two studies may be explained by the fact that insulin resistance is more likely to be associated with hyperinsulinemia, and it is evidenced that hyperinsulinemia acts as a leading cause of elevated androgen levels among PCOS women [25]. Based on that notion the researchers of the present study attributed the improvement of menstrual irregularities to the decrease in insulin resistance in the study group; that was evidenced by a significant reduction in the waist circumference at end of the study[26], causing a reduction in hyperinsulinemia, accordingly improving menstrual irregularity.
Also, the present study investigated the changes in the number of menstrual cycles over the study period and revealed a significant increase in the study group compared to insignificant changes in the control group. Interestingly the present study results agreed with the findings of Ornstein et al.[27]. They had conducted a pilot study in New York on 24 young adult/adolescent women with PCOS, aiming to investigate the effect of weight loss on menstrual function by assigning the participants randomly into low fat or low caloric diet. The authors had found a significant increase in the average menstrual cycles over the study period from 0.6±0.6 pre-treatment to 1.6±1.3 post-treatment (p=.003), with a weight loss of 6.5% (p<.001) in both dietary regimens groups. Moreover, by dichotomizing the participants into successful weight loss or unsuccessful weight loss groups, the authors[27] observed that women who successfully lost their weight were 3.4 times more likely to have improvement in their menstrual function compared to those who did not loss their weight (p=.001). Our study recommended 'energyrestricted diet' for the study group and there were no specific recommendations for the control, which makes direct comparison with Ornstein's study difficult, but we also found that menstrual patterns improved with weight loss. The reported significant increase in the number of the menstrual cycles may be related to the decrease in the stimulation of ovarian androgen production as a result of the associated reduction in hyperinsulinemia[19].
Using the Ferriman-Gallwey score, hirsutism showed a significant decrease in the study group compared to insignificant changes among the control group. Such finding is congruent with the finding of a prospective intervention study[28] conducted in Ain Shams maternity hospital., Egypt. It investigated the effectiveness of lifestyle modification; specifically, dietary counseling and exercise on PCOS symptoms in 64 women in their reproductive age. The investigators had concluded that women with PCOS who attained weight reduction as a result of lifestyle modification had showed a significant improvement in total hirsutism score. Such agreement between our finding and the Egyptian study finding [28] may be related to the improvement of the androgen excess level as a result of lifestyle modification that results in a decrease in hirsutism score.
Conversely, the present study disagrees with Hoeger et al.[24], mentioned above, which did not find significant changes of hirsutism scores by lifestyle intervention and/or metformin use. Such disagreement may be explained by two rationales; firstly, it may be related to how Hoeger and his colleagues had evaluated the hirsutism score. As in the current study the researchers considered that most women with PCOS are using cosmetic methods to manage their hirsutism, thus the women enrolled in this study were instructed to omit the hair management for the two weeks preceding hirsutism evaluation, while in the Hoeger's study[24] the interval between the excessive hair management and assessing hirsutism score is not clear, whether it was the same, shorter, or longer time interval and whether clients continued to manage the hirsutism or not. Secondly, it may be due to the younger age group of enrolled clients in the current study. All the participants were young (in mid-twenties, compared to the Hoeger's sample [24] who had a mean age of 29.4±5.7 years), post-pubertal, single, and had variable degrees of hirsutism, reflecting the exposure to the excess androgen in a relative shorter period of life.
Two limitations were raised in this study. First, the investigators relied only on the waist circumference as an indicator of insulin resistance, rather relying on more specific measures such as fasting glucose, HDL cholesterol, triglycerides and blood pressure would have been advantageous to confirm the study findings. Second, the dietary intake was evaluated according to the 24-hours dietary recalls for the last week preceding the assigned interview; indicating lack of data about the other days of the preceding month; however it was not applicable to ask the woman to daily record her intake.
Considering PCOS as heterogeneous in nature with a wide range of symptoms; health care providers working in gynecology clinics need an in-depth understanding of its pathophysiology, diagnostic measures, and symptom management. This study and others stress nurses' and gynecologists' role to ensure patients receive adequate oral and written information on lifestyle modification to be of guidance for them.
Figures and Tables
Figure 2
Number of menstrual cycles among the study and control groups at baseline and after one year of enrollment.

Table 1
General and Clinical Characteristics of the Study and Control Groups at Baseline (N=82)
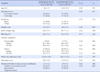
Table 2
Comparison of Body Weight, BMI, Waist Circumference, and Hirsutism Score in Study and Control Groups
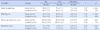
Table 3
Comparison of Rhythm of Menstrual Cycles in Study and Control Groups
Summary Statement
▪ What is already known about this topic?
Lifestyle modification for PCOS women has been found to be successful in weight loss and normalization of menstrual cycles. However, there is lack of studies that employed a control group to ensure the effect of lifestyle modification where these subjects might have lost weight without any intervention.
▪ What this paper adds?
Using a quasi-experimental design, a multidisciplinary team approach offered support/counseling in a lifestyle modification intervention overweight/obese PCOS women for 48 weeks and was effective in reducing irregularity of menstrual cycles.
▪ Implications for practice, education and/or policy
It is important for nurses to be aware that young Egyptian women with PCOS may be reluctant to seek help, and to actively promote the benefits of lifestyle modification and supportive follow up for overweight/obese PCOS women.
References
2. Abdelhafeez AT, Taha SA, Ahmad NA, Khalaf MR. Familial prevalence of PCOS and PCOS related features in Upper Egypt. Al-Azhar Assiut Med J. 2003; 1(3):1–8.
3. Teede H, Deeks A, Moran L. Polycystic ovary syndrome: A complex condition with psychological, reproductive and metabolic manifestations that impacts on health across the lifespan. BMC Med. 2010; 8:41.

4. Hoeger KM. Role of lifestyle modification in the management of polycystic ovary syndrome. Best Pract Res Clin Endocrinol Metab. 2006; 20(2):293–310.

5. Guzick DS, Wing R, Smith D, Berga SL, Winters SJ. Endocrine consequences of weight loss in obese, hyperandrogenic, anovulatory women. Fertil Steril. 1994; 61(4):598–604.
6. Moran LJ, Brinkworth GD, Norman RJ. Dietary therapy in polycystic ovary syndrome. Semin Reprod Med. 2008; 26(1):85–92.

7. Galal OM. The nutrition transition in Egypt: Obesity, undernutrition and the food consumption context. Public Health Nutr. 2002; 5(1A):141–148.

8. Moran LJ, Lombard CB, Lim S, Noakes M, Teede HJ. Polycystic ovary syndrome and weight management. Womens Health (Lond Engl). 2010; 6(2):271–283.

9. Moran LJ, Hutchison SK, Norman RJ, Teede HJ. Lifestyle changes in women with polycystic ovary syndrome. Cochrane Database Syst Rev. 2011; (2):CD007506.

10. Fearnley EJ, Marquart L, Spurdle AB, Weinstein P, Webb PM. Polycystic ovary syndrome increases the risk of endometrial cancer in women aged less than 50 years: An Australian casecontrol study. Cancer Causes Control. 2010; 21(12):2303–2308.
11. Ferriman D, Gallwey JD. Clinical assessment of body hair growth in women. J Clin Endocrinol Metab. 1961; 21:1440–1447.

12. World Health Organization. Obesity: Preventing and managing the global epidemic. Report of a WHO convention. Geneva, Switzerland: World Health Organization;2000.
13. NHANES III. National Health and Nutrition Examination Survey. Body measurements(Anthropometry) [Internet]. Rockville: National Health and Nutrition Examination Survey;1988. cite 2010 October 22. Available from: http://www.cdc.gov/nchs/data/nhanes/nhanes3/cdrom/nchs/manuals/anthro.pdf.
14. Karvetti RL, Knuts LR. Validity of the 24-hour dietary recall. J Am Diet Assoc. 1985; 85(11):1437–1442.
15. Roza AM, Shizgal HM. The Harris Benedict equation reevaluated: Resting energy requirements and the body cell mass. Am J Clin Nutr. 1984; 40(1):168–182.

16. Moran LJ, Ko H, Misso M, Marsh K, Noakes M, Talbot M, et al. Dietary composition in the treatment of polycystic ovary syndrome: A systematic review to inform evidence-based guidelines. J Acad Nutr Diet. 2013; 113(4):520–545.

17. Stener-Victorin E, Jedel E, Janson PO, Sverrisdottir YB. Low-frequency electroacupuncture and physical exercise decrease high muscle sympathetic nerve activity in polycystic ovary syndrome. Am J Physiol Regul Integr Comp Physiol. 2009; 297(2):R387–R395.

18. Jedel E, Labrie F, Odén A, Holm G, Nilsson L, Janson PO, et al. Impact of electro-acupuncture and physical exercise on hyperandrogenism and oligo/amenorrhea in women with polycystic ovary syndrome: A randomized controlled trial. Am J Physiol Endocrinol Metab. 2011; 300(1):E37–E45.

19. Yildiz BO, Knochenhauer ES, Azziz R. Impact of obesity on the risk for polycystic ovary syndrome. J Clin Endocrinol Metab. 2008; 93(1):162–168.

21. Lindenbaum C. Polycystic ovarian syndrome. Where genetics and environment collide. Adv Nurse Pract. 2010; 18(2):20–26.
22. Badawy A, Elnashar A. Treatment options for polycystic ovary syndrome. Int J Womens Health. 2011; 8(3):25–35.

23. Lass N, Kleber M, Winkel K, Wunsch R, Reinehr TH. Effect of lifestyle intervention on features of polycystic ovarian syndrome, metabolic syndrome, and intima-media thickness in obese adolescent girls. J Clin Endocrinol Metab. 2011; 96(11):3533–3540.

24. Hoeger KM, Kochman L, Wixom N, Craig K, Miller RK, Guzick DS. A randomized, 48-week, placebo-controlled trial of intensive lifestyle modification and/or metformin therapy in overweight women with polycystic ovary syndrome: A pilot study. Fertil Steril. 2004; 82(2):421–429.

25. Azziz R, Carmina E, Dewailly D, Diamanti-Kandarakis E, Escobar-Morreale HF, Futterweit W, et al. Positions statement: Criteria for defining polycystic ovary syndrome as a predominantly hyperandrogenic syndrome: an Androgen Excess Society guideline. J Clin Endocrinol Metab. 2006; 91(11):4237–4245.
26. Lee S, Bacha F, Gungor N, Arslanian SA. Waist circumference is an independent predictor of insulin resistance in black and white youths. J Pediatr. 2006; 148(2):188–194.

27. Ornstein RM, Copperman NM, Jacobson MS. Effect of weight loss on menstrual function in adolescents with polycystic ovary syndrome. J Pediatr Adolesc Gynecol. 2011; 24(3):161–165.

28. Ahmed EMS, Salem ME, Sweed MS. Effect of lifestyle modifications on polycystic ovarian syndrome symptoms. J Am Sci. 2012; 8(8):535–544.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download