Abstract
Purpose
The purpose of this study was to determine the stress, depression, and fetal attachment of pregnant women who underwent infertility treatment, and to identify factors associated with fetal attachment.
Methods
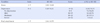
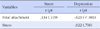
As a correlation survey design, data were collected from 136 pregnant women who underwent infertility treatment. Data were analyzed using χ2-test, t-test, ANOVA, Pearson correlation coefficients, and stepwise multiple regression.
Results
Stress, depression, and fetal attachment averaged 3.01±0.60 (range of scale 1~5), 10.02±6.51 (out of a possible 63), and 3.64±0.55 (range of scale 1~5), respectively. Level of fetal attachment was higher when mother's age was less than 35, having other children, and having prenatal education experience. Lower score of depression and client's age less than 35 were significant factors affecting fetal attachment.
Conclusion
Infertility is a life-affecting trauma for the individual, and personal and social changes due to infertility cause physical and psychological difficulties even after a successful pregnancy with infertility treatment. Therefore, prenatal management programs need to be developed giving consideration to the emotional and physical changes in order to promote physical and psychological stability in the women pregnant following infertility treatment.
Figures and Tables
Summary Statement
▪ What is already known about this topic?
Prior studies showed that pregnancy causes various physical and emotional changes to pregnant women, and negative emotions such as stress and depression negatively influence maternal-fetal attachment.
▪ What this paper adds?
Negative correlation was observed between depression and fetal attachment. Fetal attachment showed statistically significant differences according to the woman's age, having had a child or not, and herand her spouse's pre-natal education experience. The woman'slower level of depression and age less than 35 were significant factors affecting fetal attachment.
▪ Implications for practice, education and/or policy
Infertility-related healthcare professionals need to understand infertility-treated pregnant women's emotional changes and help them overcome their psychological and emotional difficulties and reach appropriate solutions. In addition, adequate nursing intervention programs should be developed to help these women adapt and deal with the various challenges they face during pregnancy.
References
1. Hwang N. Factors related to the depression of infertile women. Health Soc Welf Rev. 2013; 33(3):161–187.
2. Kim YJ, Jee BC, Suh CS, Kim SH. Effects of conversion of infertility treatment on semen quality. Korean J Reprod Med. 2007; 34(3):159–166.
3. Wang YA, Macaldowie A, Hayward I, Chambers GM, Sullivan EA. Assisted reproductive technology in Australia and New Zealand 2009 [Internet]. Canberra: Australian Institute of Health and Welfare (AIHW);2009. cited 2013 May 13. Available from: http://www.aihw.gov.au/publication-detail/?id=10737420465.
4. McMahon CA, Tennant C, Ungerer J, Saunders D. 'Don't count your chickens': A comparative study of the experience of pregnancy after IVF conception. J Reprod Infant Psychol. 1999; 17(4):345–356.

5. Chang EY. Women's experiences of pregnancy after infertility[master's thesis]. Seoul: Ewha Womans University;1998.
6. Hjelmstedt A, Widström A, Wramsby HM, Collins A. Patterns of emotional responses to pregnancy, experience of pregnancy and attitudes to parenthood among IVF couples: A longitudinal study. J Psychosom Obstet Gynaecol. 2003; 24(3):153–162.

7. Bennett SM, Litz BT, Lee BS, Maguen S. The scope and impact of perinatal loss: Current status and future directions. Prof Psychol Res Pr. 2005; 36(2):180–187.

8. Choi SK, Ahn SY, Shin JC, Jang DG. A clinical study of depressive symptoms during pregnancy. Korean J Obstet Gynecol. 2009; 52(11):1102–1108.
9. Dayan J, Creveuil C, Marks MN, Conroy S, Herlicoviez M, Dreyfus M, et al. Prenatal depression, prenatal anxiety, and spontaneous preterm birth: A prospective cohort study among women with early and regular care. Psychosom Med. 2006; 68(6):938–946.

10. O'Keane V, Marsh MS. Depression during pregnancy. BMJ. 2007; 334(7601):1003–1005.
11. Covington SN, Burns LH. Pregnancy after infertility. In : Burns LH, Covington SN, editors. Infertility counselling: A comprehensive handbook for clinicians. Pearl River, New York: The Parthenon Publishing Group;1999. p. 425–447.
12. Kang CY, Youn JY. The pregnant woman-fetus interaction and attachment development. J Child Stud. 2004; 10:131–147.
13. Schore AN. Effects of a secure attachment relationship on right brain development, affect regulation, and infant mental health. Infant Ment Health J. 2001; 22(1-2):7–66.

14. Walker LO, Cooney AT, Riggs MW. Psychosocial and demographic factors related to health behaviors in the 1st trimester. J Obstet Gynecol Neonatal Nurs. 1999; 28(6):606–614.

15. Yarcheski A, Mahon NE, Yarcheski TJ, Hanks MM, Cannella BL. A meta-analytic study of predictors of maternal-fetal attachment. Int J Nurs Stud. 2009; 46(5):708–715.

16. Davies MJ, Moore VM, Willson KJ, Van Essen P, Priest K, Scott H, et al. Reproductive technologies and the risk of birth defects. N Engl J Med. 2012; 366(19):1803–1813.

17. Hargreave M, Jensen A, Toender A, Andersen KK, Kjaer SK. Fertility treatment and childhood cancer risk: A systematic meta-analysis. Fertil Steril. 2013; 100(1):150–161.

18. Ahn HL. An experimental study of the effects of husband's supportive behavior reinforcement education on stress relief of primigravidas. J Nurs Acad Soc. 1985; 15(1):5–16.

19. Lee YH, Song JY. A study of the reliability and the validity of the BDI, SDS and MMPI-D Scales. Korean J Clin Psychol. 1991; 10(1):98–113.
20. Cranley MS. Development of a tool for the measurement of maternal attachment during pregnancy. Nurs Res. 1981; 30(5):281–284.

21. Oh J, Kim YA. A comparative study on acceptance and maintain behavior of pregnancy between natural pregnant and infertility treated women. J Korean Soc Matern Child Health. 2008; 12(2):155–165.
22. Harris DL, Daniluk JC. The experience of spontaneous pregnancy loss for infertile women who have conceived through assisted reproduction technology. Hum Reprod. 2010; 25(3):714–720.

23. Ulrich D, Gagel DE, Hemmerling A, Parstor VS, Kentenich H. Couples becoming parents: Something special after IVF? J Psychosom Obstet Gynaecol. 2004; 25(2):99–113.

24. Latendresse G. The interaction between chronic stress and pregnancy: Preterm birth from a biobehavioral perspective. J Midwifery Womens Health. 2009; 54(1):8–17.

25. Kwon MK, Bang KS. Relationship of prenatal stress and depression to maternal-fetal attachment and fetal growth. J Korean Acad Nurs. 2011; 41(2):276–283.

26. Cho HJ, Kwon JH. A test of the attachment model of prepartum depression. Korean J Clin Psychol. 2002; 21(4):727–744.
27. Pascoe JM, Kototailo PK, Broekhuizen FF. Correlates of multigravida women's binge drinking during pregnancy. A longitudinal study. Arch Pediatr Adolesc Med. 1995; 149(12):1325–1329.
29. Fisher JR, Hammarberg K, Baker GH. Antenatal mood and fetal attachment after assisted conception. Fertil Steril. 2008; 89(5):1103–1112.

30. Bar-Hava I, Orvieto R, Ferber A, Ashkenazi J, Dicker D, Ben-Rafael Z. Standard in vitro fertilization or intracytoplasimic sperm injection in advanced female age-what may be expected? Gynecol Endocrinol. 1999; 13(2):93–97.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download