Abstract
Purpose
The purpose of this study was to identify nutritional status, and relationships among malnutrition, depression and quality of life in patients with gynecologic cancer who were receiving chemotherapy.
Methods
For this study a descriptive cross-sectional design was used. Participants were 111 women who were enrolled and agreed to undergo a face-to-face interviews including administration of the structured questionnaires: Patient-Generated Subjective Global Assessment (PG-SGA), Beck Depression Inventory (BDI), Simplified Nutritional Appetite Questionnaire (SNAQ), and Functional Assessment of Cancer Therapy-General (FACT-G).
Results
Mean body mass index was 23.3 and mean body weight was 56.5 kg. Sixty-three (57%) of the 111 patients were malnourished according to the PG-SGA. The malnourished patients showed higher levels of depression and lower quality of life compared to the non-malnourished patients. In addition, malnutrition was associated with BMI level, depression, appetite and quality of life.
Conclusion
The findings indicate that the prevalence of malnutrition is high and malnutrition in patients with gynecologic cancer influences depression and adversely affects the quality of life of these women. To improve the patient's quality of life, nutritional assessment and appropriate management is important to decrease malnutrition in patients with gynecologic cancer.
Figures and Tables
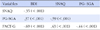
Table 2
Nutritional Status, Depression, and Quality of Life of Patients with Chemotherapy (N=111)

PG-SGA=patient-generated subjective global assessment; BMI=body mass index; SNAQ=simplified nutritional appetite questionnaire; BDI=Beck depression inventory; FACT-G=functional assessment of cancer therapy-general; PWB=physical well-being; SWB=social/family well-being; EWB=emotional well-being; FWB=functional well-being.
Table 3
Malnutrition, Depression and Quality of Life by General Characteristics of Participants (N=111)

Summary Statement
▪ What is already known about this topic?
Malnutrition is a major problem for cancer patients in general, and the same is true for patients with gynecologic cancer who are on chemotherapy.
▪ What this paper adds?
Malnutrition in patients with gynecologic cancer was found to influence depression and adversely affect quality of life in these patients.
▪ Implications for practice, education and/or policy
As the prevalence of malnutrition is high, nutritional assessment using a validated tool such as PG-SGA is essential for patients with gynecologic cancer who are receiving chemotherapy.
References
1. Middleton MH, Nazarenko G, Nivison-Smith I, Smerdely P. Prevalence of malnutrition and 12-month incidence of mortality in two Sydney teaching hospitals. Intern Med J. 2001; 31(8):455–461.

2. Barrera R. Nutritional support in cancer patients. JPEN J Parenter Enteral Nutr. 2002; 26:5 Suppl. S63–S71.

3. Sheard JM, Ash S, Silburn PA, Kerr GK. Prevalence of malnutrition in Parkinson's disease: A systematic review. Nutr Rev. 2011; 69(9):520–532.

4. Van Cutsem E, Arends J. The causes and consequences of cancer-associated malnutrition. Eur J Oncol Nurs. 2005; 9:Suppl 2. S51–S63.

5. Brugler L, Stankovic AK, Schlefer M, Bernstein L. A simplified nutrition screen for hospitalized patients using readily available laboratory and patient information. Nutrition. 2005; 21(6):650–658.

6. Langer CJ, Hoffman JP, Ottery FD. Clinical significance of weight loss in cancer patients: Rationale for the use of anabolic agents in the treatment of cancer-related cachexia. Nutrition. 2001; 17:1 Suppl. S1–S20.

7. Laky B, Janda M, Kondalsamy-Chennakesavan S, Cleghorn G, Obermair A. Pretreatment malnutrition and quality of life - association with prolonged length of hospital stay among patients with gynecological cancer: A cohort study. BMC Cancer. 2010; 10:232.

8. Lis CG, Gupta D, Lammersfeld CA, Markman M, Vashi PG. Role of nutritional status in predicting quality of life outcomes in cancer-a systematic review of the epidemiological literature. Nutr J. 2012; 11:27.

9. Gupta D, Lammersfeld CA, Vashi PG, Dahlk SL, Lis CG. Can subjective global assessment of nutritional status predict survival in ovarian cancer? J Ovarian Res. 2008; 1(1):5.

10. Laky B, Janda M, Bauer J, Vavra C, Cleghorn G, Obermair A. Malnutrition among gynaecological cancer patients. Eur J Clin Nutr. 2007; 61(5):642–646.

11. Ryan M, White K, Roydhouse JK, Fethney J. A description of the nutritional status and quality of life of Australian gynaecological cancer patients over time. Eur J Oncol Nurs. 2012; 16(5):453–459.

12. Britton B, Clover K, Bateman L, Odelli C, Wenham K, Zeman A. Baseline depression predicts malnutrition in head and neck cancer patients undergoing radiotherapy. Support Care Cancer. 2012; 20(2):335–342.

13. Massie MJ. Prevalence of depression in patients with cancer. J Natl Cancer Inst Monogr. 2004; 32:57–71.

14. Suzuki N, Ninomiya M, Maruta S, Hosonuma S, Nishigaya Y, Kobayashi Y. Psychological characteristics of Japanese gynecologic cancer patients after learning the diagnosis according to the hospital anxiety and depression scale. J Obstet Gynaecol Res. 2011; 37(7):800–808.

15. Gil KM, Gibbons HE, Jenison EL, Hopkins MP, von Gruenigen VE. Baseline characteristics influencing quality of life in women undergoing gynecologic oncology surgery. Health Qual Life Outcomes. 2007; 5:25.

16. Mendonsa RD, Appaya P. Psychiatric morbidity in outpatients of gynecological oncology clinic in a tertiary care hospital. Indian J Psychiatry. 2010; 52(4):327–332.

17. Ottery FD. Definition of standardized nutritional assessment and interventional pathways in oncology. Nutrition. 1996; 12:1 Suppl. S15–S19.

18. Bauer J, Capra S, Ferguson M. Use of the scored Patient-Generated Subjective Global Assessment (PG- SGA) as a nutrition assessment tool in patients with cancer. Eur J Clin Nutr. 2002; 56(8):779–785.
19. McCallum PD, Polisena CG. Clinical guide to oncology nutrition. 1st ed. Chicago: The American Dietetic Association;2000.
20. Park MY, Park JY. Pre-and post-transplant nutritional assessment in patients undergoing allogeneic hematopoietic stem cell transplantation. Asian Oncol Nurs. 2012; 12(1):110–116.
21. Wilson MM, Thomas DR, Rubenstein LZ, Chibnall JT, Anderson S, Baxi A. Appetite assessment: simple appetite questionnaire predicts weight loss in community-dwelling adults and nursing home residents. Am J Clin Nutr. 2005; 82(5):1074–1081.

22. Lee KR. Efficacy of nutrition management program on performance ability, physical function, nutritional status in frail elderly [master's thesis]. Seoul: Kyung Hee University;2012.
23. Beck AT. Depression: Clinical, experimental, and theoretical aspects. New York: Hoeber Medical Division, Harper & Row;1967.
24. Lee YH, Song JY. A study of the reliability and the validity of the BDI, SDS, and MMPI-D scales. Korean J Clin Psychol. 1991; 10(1):98–113.
25. Jo SA, Park MH, Jo I, Ryu SH, Han C. Usefulness of Beck Depression Inventory (BDI) in the Korean elderly population. Int J Geriatr Psychiatry. 2007; 22(3):218–223.

26. Cella D. FACIT manual: Manual of the Functional Assessment of Chronic Illness Therapy (FACIT) measurement system. Evanston, IL: Center on Outcomes, Research and Education;1997.
27. Byun MS, Kim NH. Energy intake and fatigue in patients receiving chemotherapy. J Korean Biol Nurs Sci. 2012; 14(4):258–267.

28. Kim YH, Lee JH. Relationships between side effects, depression and quality of sleep in gynecological cancer patients undergoing chemotherapy. Korean J Women Health Nurs. 2010; 16(3):276–287.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download