Abstract
Purpose
The objective of this study was to identify the relationships among symptom bother, physical and mental stress and health-related quality of life (HRQoL) in women with overactive bladder (OAB) syndrome.
Methods
The participants were 106 women who were diagnosed with OAB (urgency, urge urinary incontinence, frequency, and/or nocturia) at P university hospital. Data were collected from Dec 23, 2011 to Aug 31, 2012.
Results
The mean score for symptom bother was 43.1 points, for physical stress, 12.8 which was slightly higher than mental stress (11.8), and for HRQoL, 63.9. For symptom type, there were statistically significant differences in the symptom bother (F=8.67, p<.001) and HRQL (F=3.32, p= .023). The Symptom bother of OAB was positively correlated with physical stress (r=.23, p= .014) and mental stress (r=.33, p<.001) and negatively correlated with the subscales of HRQoL; coping (r=-.66, p<.001), concern (r=-.71, p<.001), sleep (r=-.59, p<.001), and social interaction (r=-.58, p<.001).
Figures and Tables
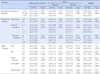
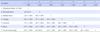
Table 4
Comparison of OAB Symptom bother, Stress and HRQoL by Disease related Characteristics (N=106)
References
1. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: Report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002; 21:167–178.

2. An HE. Symptom severity and quality of life of elderly women with overactive bladder symptoms in rural area. Incheon: The Inha University;2010. Unpublished master's thesis.
3. Bartoli S, Aguzzi G, Tarricone R. Impact on quality of life of urinary incontinence and overactive bladder: A systematic literature review. Urology. 2010; 75:491–500. http://dx.doi.org/10.1016/j.urology.2009.07.1325.

4. Brubaker L, Chapple C, Coyne KS, Kopp Z. Patientreported outcomes in overactive bladder: Importance for determining clinical effectiveness of treatment. Urology. 2006; 68:3–8.

5. Chen GD, Lin TL, Hu SW, Chen YC, Lin LY. Prevalence and correction of urinary incontinence and overactive bladder in Taiwanese women. Neurourol Urodyn. 2003; 22:109–117. http://dx.doi.org/10.1002/nau.10010.
6. Chung HS, Kim JS, Kim SO, Kim HS, Kwon D, Park K, et al. Age related changes of voiding patterns in women with overactive bladder. J Korean Continence Soc. 2009; 13:37–44.

7. Cohen J. Statistical power for the behavioral sciences. 2nd ed. Hillsdale, NJ: Erlbaum;1988.
8. Coyne KS, Payne C, Bhattacharyya SK, Revicki DA, Thompson C, Corey R, et al. The impact of urinary urgency and frequency on health-related quality of life in overactive bladder: Results from a national community survey. Value Health. 2004; 7:455–463.
9. Coyne KS, Wein AJ, Tubaro A, Sexton CC, Thompson CL, Kopp ZS. The burden of lower urinary tract symptoms: Evaluating the effect of LUTS on health-related quality of life, anxiety and depression; EpiLUTS. BJU Int. 2009; 103 Suppl 3:4–11. http://dx.doi.org/10.1111/j.1464-410X.2009.08371.x.

10. Coyne K, Revicki D, Hunt T, Corey R, Stewart W, Bentkover J, et al. Psychometric validation of an overactive bladder symptom and health-related quality of life questionnaire: The OAB-q. Qual Life Res. 2002; 11:563–574.
11. Faul F, Erdfelder E, Lang AG, Buchner A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007; 39:175–191.
12. Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, et al. Population-based survey of urinary incontinence, overactive bladder, and the other lower urinary tract symptoms in five countries: Results of the EPIC study. Eur Urol. 2006; 50:1306–1314.
13. Jang IS, Lee JY, Oh DN, Kim J, Jung HJ, Park S. Factors affecting on lower urinary tract symptoms in middle-aged women. J Korean Biol Nurs Sci. 2009; 11:176–182.
14. Jun EM, Cho DS. The relationship of symptoms of stress, cancer prevention behavior and the quality of life in women. Korean J Women Health Nurs. 2005; 11:156–162.

15. Kim SA. The relating factors and quality of life of overactive bladder patients in adults. Seoul: The Konkuk University;2010. Unpublished master's thesis.
16. Kim UH, Kim YH, Kim ME. The prevalence and quality of life of overactive bladder and urinary incontinence in young women. Korean J Urol. 2004; 45:543–550.
17. Milsom I, Abrams P, Cardozo L, Roberts RG, Thuroff J, Wein AJ. How widespread are the symptoms of anoveractive bladder and how are they managed? A population- based prevalence study. BJU Int. 2001; 87:760–766.
18. Milsom I, Kaplan SA, Coyne KS, Sexton CC, Kopp ZS. Effect of bothersome overactive bladder symptoms in health-related quality of life, anxiety, depression, and treatment seeking in the United State: Results form EpiLUTs. Urology. 2012; 80:90–96. http://dx.doi.org/10.1016/j.urology.2012.04.004.
19. Park SY. Stress and my health. Gwangju-city Sea-gu Health News. 1999; 11(84):7–9.
20. Sand PK, Appell R. Disruptive effects of overactive bladder and urge urinary incontinence in younger women. Am J Med. 2006; 119:16–23.

21. Sexton CC, Coyne KS, Thompson C, Bavendam T, Chen CI, Markland A. Prevalence and effect on health-related quality of life of overactive bladder in older Americans: Results from the epidemiology of lower urinary tract symptoms study. J Am Geriatr Soc. 2011; 59:1465–1470. http://dx.doi.org/10.1111/j.1532-5415.2011.03492.x.

22. Stewart WF, Van Rooyen JB, Cundiff GW, Abrams P, Herzog AR, Corey R, et al. Prevalence and burden of overactive bladder in the United States. World J Urol. 2003; 20:327–336.

23. Van der Vaart CH, De Leeuw JR, Roovers JP, Heintz AP. The effect of urinary incontinence and overactive bladder symptoms on quality of life in young women. BJU Int. 2002; 90:544–549.

24. Wennberg AL, Molander U, Fall M, Edlund C, Peeker R, Milsom I. A longitudinal population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in women. Eur Urol. 2009; 55:783–791. http://dx.doi.org/10.1016/j.eururo.2009.01.007.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download