Abstract
Purpose
This study was conducted to examine the effects of simulation-based education on communication skill and clinical competence in maternity nursing practicum.
Methods
This study used a non-equivalent control pretest-posttest design. The simulation-based education in maternity nursing practicum consisted of two clinical situation scenarios pertaining to patients with normal and high-risk deliveries. The control group consisted of 35 students in 2010 and the experimental group consisted of 35 students in 2009. The experimental group was given the simulation-based education using a high-fidelity patient simulator over 3 sessions, whereas the control group was given a conventional pre-clinical practice orientation before maternity nursing clinical practicum. Data were collected using a questionnaire, which included questions to assess communication skill and clinical competence. Data were analyzed using SPSS/WIN 18.0.
Results
Members of the experimental group, who received the simulation-based education, showed significantly higher communication skill and clinical competence scores than the control group (t=-2.39, p = .020; t=-2.71, p = .009).
Conclusion
The simulation-based education in maternity nursing practicum is effective in promoting communication skill and clinical competence. With application of diverse clinical situation scenarios, it is recommended to develop and apply simulation-based education using a high-fidelity simulator in the area of maternity nursing.
The aim of nursing education is to produce professional nurses, who, after completing nursing school, are capable of professionally solving the health problems of patients. Nursing students acquire a wide range of theoretical knowledge in the nursing curriculum. In addition to theory, practical education is essential to develop the ability to solve the health problems of patients in practice (Shin, Hur, Park, Song, & Kim, 2007). Practical education teaches students to apply in practice the theoretical knowledge acquired in school. It can be divided into education obtained in the lab and education obtained through clinical practice. Traditionally, clinical practice education has been structured as practical experience occurring in a real-world environment (Lee & Kim, 2011).
Therefore, nursing educators should provide opportunities for clinical practice education designed for nursing students that would enable them to perform effective nursing and to assess patients appropriately in dynamic clinical situations (Larew, Lessans, Spunt, Foster, & Covington, 2006). However, clinical practice education taking place onsite in an actual practice generally do not work as planned in accordance with the learning goals set by the professor. This is due to factors such as unpredictable working environments, the need to consider patients' comfort and safety, increased attention to patients' rights and self-determination, and the shortage of field training personnel compared to the number of students. Therefore, observation-oriented practical education needs to be conducted. As a result, the satisfaction of nursing students with their clinical practice education is low and the opportunity of obtaining sufficient clinical competency through practical education is limited (Kim et al., 2011).
In the area of obstetric nursing practice, in particular, there is more difficulty than in other fields in obtaining clinical practice onsite. Due to unpredictable progress of labor, unexpected occurrences interfering with learning opportunities are common and emergency situations frequently occurred during delivery. Thus, nursing students often don't have the opportunity to provide direct nursing care to the patients who are in labor (Chung, Kim, & Park, 2011). In addition, because of concerns for the safety of the mother and fetus and for the mother's privacy, it is difficult for students to observe and perform the practice of nursing. Moreover, due to the low fertility rate in Korea, the opportunity to participate in core practical experiences of maternity nursing, such as observation of deliveries, is limited and it is difficult to find appropriate hospitals (Kim & Park, 2006). To remedy these problems and to achieve the learning objectives of the maternity nursing practicum, new teaching and learning methods are required.
Simulation-based education consists of various forms of education including multimedia technology, anatomical models, and simulators of the human body. It is a new education strategy that improves the safety of patients. This education is designed to mimic real-life situations and provide opportunities for health professionals and students to find solutions for clinical problems. It provides the opportunity to perform clinical decision-making without generating any risk to patients (Bond & Spillane, 2002). In addition, because a standardized curriculum can be provided and all students have the same experience (Ellis et al., 2008), it is considered to be an educational alternative that can overcome the limitations of the maternity nursing practicum.
Problems in maternity nursing are complex because they involve the entire process leading to pregnancy, delivery, and the period after delivery. Problems can spontaneously arise at any point throughout this entire time course and can include a variety of problems involving the whole family (Kim, Park, Chung, & Kim, 2006). Normally, there are pregnant women in labor, along with each woman's husband and her family, in the delivery room. Thus, labor and delivery nurses have to be concerned not only with clinical competence based on a contextual understanding of the labor process, but also with the family members. Effective communication skills are therefore needed as well as clinical skills (Chung et al., 2011). There had been only two previous studies on simulation education in the field of maternity nursing and the results showed the educational effects leading to increased confidence among the nursing students in their nursing performance (Chung et al., 2011; Lee & Kim, 2011). This study was differentiated from existing studies of delivery simulation in nursing by focusing on the nursing process. Therefore, the purpose of the current study was to investigate the effect of simulation-based education in maternity nursing practicum.
The purpose of this study was to determine the effect of simulation-based education on the communication skill and clinical competence of nursing students in maternity nursing practicum.
Hypothesis 1: There will be a difference in communication skill between experimental group who participated in the simulation-based education in maternity nursing practicum and control group who did not.
Hypothesis 2: There will be a difference in clinical competence between experimental group who participated in the simulation-based education in maternity nursing practicum and control group who did not.
This study was designed as a quasi-experimental study, using a nonequivalent control group and a pretest-posttest design to examine the effects of simulation-based education on the communication skill and clinical competence of nursing students in maternity nursing practicum.
The participants enrolled in this study were junior nursing students. They had taken a theoretical course in maternity nursing covering prenatal care and delivery as second semester sophomores. Nursing students who were willing to participate in simulation-based education were enrolled in this study. They participated in simulation-based education for three weeks and were then placed in the labor and delivery room of a university hospital or women's hospital for two weeks. The students did not have any previous simulation-based learning experiences prior to participating in this study. The experimental group was composed of students who participated in 2009. The following year, the control group was composed of participants who were junior nursing students in 2010. The number of subjects needed was calculated according to Cohen's sampling formula by using a sample size calculation program G*power 3.1.3. Based on the calculation results with two-tailed significance level α=.05, large effect size d=.80, and power=.90, the minimum sample size required for each group was 34 (Faul, Erdfelder, Buchner, & Lang, 2009). At the beginning of the study, the experimental group size was 38 and the control group size was 35, but three members of the experimental group were eliminated. The reasons for the elimination were that two of them missed one or more classes during the simulation-based education and the remaining participant provided insufficient answers to the questionnaire. Thus, the final experimental group size was 35 and the control group size was 35, making 70 subjects in total.
Communication skill was measured using a tool developed by Yoo (2001) to evaluate nursing students' ability to communicate. E-mail approval was received from the original author for use of the tool. This tool contained a total of five questions with a 5-point scale: two questions to determine professional attitude as a nurse and three questions to determine whether sufficient explanation was provided during the nursing care. The higher the score, the higher the level of communication skill a subject possessed. Cronbach's α of this tool was .89 in Lee's study (2011) and .90 in this study.
In order to verify the homogeneity of clinical competence, a tool from Yang and Park (2004) was used. Verbal approval was received over the phone from the original author (Yang) for use of the tool. This tool contained a total of 19 items with a 5-point scale: four questions about the nursing process skills of nursing students, four questions determining the ability to perform direct nursing interventions, three questions for psychosocial nursing ability, three questions for patient education ability, three questions assessing ability in basic nursing performance, and two questions for physical examination and patient monitoring capabilities. The higher the score, the higher the level of clinical competence. Cronbach's α of this tool was .86 in Yang and Park's study (2004) and .89 in this study.
Post-evaluation for clinical competence was done using a tool developed by Yang and Park (2004) after modifying it to fit clinical competence related to delivery nursing. The validity of the content was examined by two professors of maternity nursing, two clinical practice instructors, and one professor of fundamental nursing. The validity index of all of the questions was more than .80. This tool contained a total of 19 items with a 5-point scale: four questions about the nursing process skills of nursing students, four questions determining the ability to perform direct nursing interventions, three questions for psychosocial nursing ability, three questions for patient education ability, three questions assessing ability in basic nursing performance, and two questions for physical examination and patient monitoring capabilities related to delivery. The higher the score, the higher the level of clinical competence. Cronbach's α of this tool for reliability was .90 in this study.
The process of developing the simulation-based education in maternity nursing practicum was as follows: The simulation-based education consisted of situations which a nurse might be required to handle in a normal delivery and a high-risk delivery, which were the main learning contents for the labor and delivery practice. The simulation-based practical education was conducted in the simulation lab in teams of three or four students over a period of 3 weeks before a maternity nursing clinical practicum, and consisted of 3 sessions, for a total of 9 hours. In the first session, orientation was conducted in which the simulation-based education courses and the normal delivery and high-risk delivery scenarios were presented. In one of the scenarios, a 38-year-old primipara visited the hospital due to rupture of membranes and suffered hypertonic uterine dysfunction during delivery. After team discussion, a summary of the nursing process and the concept maps of the clinical cases were written. According to the nursing process and concept maps, nursing students practiced taking vital signs, performing intravenous injections, and providing oxygen therapy. In the second and third sessions, simulations of normal and high-risk deliveries were conducted, respectively. After the second and the third sessions, all the students were gathered and a debriefing was conducted in which the students talked about their experiences, strengths and weaknesses, and analyzed the simulation situations (Figure 1). After the completion of the simulation-based education, on the Friday of the week before the beginning of maternity nursing clinical practicum, pre-clinical practice orientation for the maternity nursing clinical practicum was conducted for the experimental group. The orientation contents included goals of the maternity nursing clinical practicum and cautions. Conventional pre-clinical practice orientation, for the control group, was conducted through a lecture. The contents were the same as those for the experimental group, with the addition of watching movies on delivery nursing and childbirth. The pre-survey was done before the simulation-based education and the post-survey was conducted at the end of the two weeks of maternity nursing clinical practicum (Figure 2). The 3-week simulation-based education was conducted for the control group after the completion of nursing clinical practicum as well.
The purpose and procedure of this study, voluntary participation, guaranteed anonymity, and the possibility to abandon the trial were explained to the subjects and written consent was obtained. After collecting the survey data, simulation-based education in maternity nursing was also conducted for the control group.
The statistical package for social sciences software (SPSS/WIN 18.0) was used for data analysis (SPSS Inc., Chicago, IL, USA). The general characteristics of the experimental group and the control group (age, presemester grades) and pre-homogeneity of the dependent variable were analyzed with an independent t-test. To test the effects of simulation-based education in maternity nursing practicum, an independent t-test was applied to test for any difference between pretest and posttest data for the control and experimental groups.
The subjects of this study were junior nursing students with an experimental group size of 35 and a control group size of 35, for a total of 70 students. The ages and the pre-semester grades of the two groups were not significantly different.
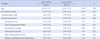
In the pre-survey before the experiment, the results of the homogeneity test for the dependent variable showed the average score for communication skill to be 3.69±0.61 for the experimental group and 3.91±0.63 for the control group. The average score for clinical competence was 3.53±0.54 for the experimental group and 3.69±0.49 for the control group. Homogeneity between the two groups was not significantly different (t=-1.54, p=.128; t=-1.33, p=.188)(Table 1).
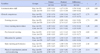
"There will be a difference in communication skill between experimental group who participated in the simulation-based education in maternity nursing practicum and control group who did not." The communication skill score of the experimental group that participated in simulation-based education increased 0.58 points from 3.69±0.61 to 4.27±0.50 and the score for the control group increased 0.09 points from 3.91±0.63 to 4.01±0.58, indicating a significant difference between the two groups (t=-2.39, p=.020).
Thus, hypothesis 1 was supported (Table 2).
"There will be a difference in clinical competence between experimental group who participated in the simulation-based education in maternity nursing practicum and control group who did not." The clinical competence score of the experimental group that participated in simulation-based education increased 0.63 points from 3.53±0.54 to 4.16±0.44 and the score for the control group increased 0.15 points from 3.69±0.49 to 3.84±0.46, indicating a significant difference between the two groups (t=-2.71, p=.009). Thus, hypothesis 2 was supported (Table 2).
The purpose of this study was to determine the effect of simulation-based education on the communication skill and clinical competence of nursing students and to contribute to the improvement of nursing clinical skills. The final scenario, including normal and high-risk deliveries was developed by reviewing maternity nursing practicum learning objectives.
Maternity nursing clinical practice could be performed after the simulation-based education by applying the learned nursing process. The communication skill of the experimental group that participated in simulation-based education increased. This result supported the finding by Birch et al.,(2007) that simulation improved communication skill and the finding by Medley and Horne (2005) that communication could be promoted through simulation. In addition, Lee and Kim (2011) showed that the students were able to communicate and they had confidence about performing clinical skills after completing simulation-based education in obstetric nursing. On the other hand, any research finding showed simulation-based education did not improve communication skill (Lee, Cho, Yang, Roh, & Lee, 2009). This result was differentiated from current study. The subjects were freshman in Lee et al.,(2009)s study and junior in this study. Also, in the 1st session of this study, subjects wrote nursing process and concept map about clinical scenarios. One of the nursing diagnoses that subjects derived was anxiety. The nursing activities to reduce anxiety of patient and her family members could be helped improvement of communication skill of the experimental group. Thus, it is necessary to evaluate communication skill considered subjects' characteristics, to identify communication skill improvement for prolonged periods and to analyze subjects' communication contents and quality in future research.
The clinical competence of the experimental group that participated in simulation-based education in maternity nursing practicum also improved, which was consistent with the results of prior studies. Among the sub-area scores of clinical competence, basic nursing performance score were the highest, followed by patient education, and psychosocial nursing. This result matched the findings of Alinier, Hunt and Gordon (2004) that simulation-based education helped to improve skills, and also matched the findings of Hur, Choi, Jung, Kang, & Kim (2012) that simulation-based practice improved the performance skills of nursing students. The students' basic nursing performance improved because the simulation-based education included practice with taking vital signs, performing intravenous injections, and providing oxygen therapy in its first session, which preceded the actual simulation in the second session. In addition, since the subjects of this study didn't have simulation-related learning experience, the opportunities to perform repetitive procedures during the simulation-based education had positive results.
The second highest score among the sub-areas of clinical competence was in the patient education area. Since there had been no previous study on patient education abilities, it was difficult to make a comparison, but the patient education score was lowest among the clinical competence areas in Yang's study (2012). This was due to differences in the experience of the study subjects in the situations and scenarios provided. Unlike other areas of maternity nursing, patient education and psychosocial nursing care were essential because nurses had to take care of both patients and their families during labor, and that required cooperation. Also, patient education abilities were one of the core components that nurses needed to learn. Therefore, in an effective study, it was necessary to develop education abilities in a variety of scenarios through simulation-based education.
The most increased score among the sub-areas of clinical competence was physical examination and patient monitoring. This result was consistent with the fact that delivery nursing practice education utilizing simulation had been shown to improve the interpretation of results of electronic fetal monitoring, the assessment of uterine contraction patterns, and confidence regarding recording in clinical competence (Chung et al., 2011). Simulation-based education also helped to improve the skills in usage and reading of various medical devices (Lee, Kim, Yeo, Cho, & Kim, 2009). In addition, in studies on assessment related items, such as an assessment of subjective-objective data and interpreting vital signs, results were improved over those of other items (Lee & Choi, 2011). The study conducted by Yang (2012) had similar results. Furthermore, the results supported the finding that 61% of learners who performed physical examination in simulation-based education before the first clinical practice had increased confidence in their abilities (Bremmer, Aduddell, Bennett, & VanGreest, 2006).
At the beginning of simulation-based education, the scenario was presented in the first session and the nursing process and concept maps of the clinical scenario were made through team discussion. There had been only one study performed on applying simulation-based education to the nursing process. The result showed that there was a difference between the experimental group and the control group in the number of nursing diagnoses derived (Ham, 2009). The results of current study in the clinical area showed a score for nursing process for the experimental group of 0.64 and for the control group of 0.30, showing a score increased by 0.34 points. There is not a statistically significant difference in both groups. The post-test was administered after two weeks of maternity nursing clinical practice. Thus, it did not rule out the influence of conventional clinical practice and education, while trying to study a case to apply the nursing process to patients. Moreover, the results of this study were obtained through self-reported surveys of study subjects. Therefore, teachers should evaluate the quality of applied nursing process in future research.
It was believed that the simulation-based education in maternity nursing practicum was a way to overcome the limited opportunities for maternity nursing clinical practice caused by the decreased birth rate and by patient issues such as privacy protection. It would be an effective teaching and learning method to assist nursing students in understanding patients' experience with labor and their family situations and to improve communication skill and clinical competence in dynamic situations.
The purpose of this study was to determine the effect of simulation-based education on the communication skill and clinical competence of nursing students in maternity nursing practicum. The results were as follows:
The communication skill score and clinical competence score of the experimental group that participated in simulation-based education increased compared to the control group. Thus, hypotheses 1 and 2 were supported.
Based on the above results, the following suggestions could be made:
First, it was suggested to apply a wide variety of scenarios developed for use in simulation-based education in the area of maternity nursing.
Second, it was suggested to research and develop standardized tools that can measure the effectiveness of simulation-based education in maternity nursing.
Figures and Tables
Summary Statement
▪ What is already known about this topic?
Simulation-based learning is considered a complementary training method to compensate for circumstances that limit real-world clinical practicum, such as the reduction in clinical practice opportunities and the use of observation-oriented practice.
▪ What does this paper add?
A three-session simulation-based education concerning normal deliveries and high-risk deliveries took place three weeks before the beginning of a maternity nursing clinical practicum.
▪ Implications for practice, education and/or policy
The simulation-based education in maternity nursing practicum was effective in improving communication skill and clinical competence, and is regarded as a method that can overcome limitations in clinical practice.
References
1. Alinier G, Hunt W, Gordon R. Determining the value of simulation in nurse education: Study design and initial results. Nurse Educ Pract. 2004. 4:200–207. http://dx.doi.org/10.1016/S1471-5953(03)00060-0.

2. Birch L, Jones N, Doyle PM, Green P, McLaughlin A, Champney C, et al. Obstetric skills drills: Evaluation of teaching methods. Nurse Educ Today. 2007. 27(8):915–922.

3. Bond WF, Spillane L. The use of simulation for emergency medicine resident assessment. Acad Emerg Med. 2002. 9(11):1295–1299.

4. Bremner MN, Aduddell K, Bennett DN, VanGreest JB. The use of human patients simulators: Best practice with novice nursing students. Nurse Educ. 2006. 31(4):170–174.
5. Chung CW, Kim HS, Park YS. Effects of high-fidelity simulation-based education on maternity nursing. Perspect Nurs Sci. 2011. 8(2):86–96.
6. Ellis D, Crafts JE, Hent LP, Read M, Fox R, James M. Hospital, simulation center, and teamwork training for eclampsia management: A randomized controlled trial. Obstet Gynecol. 2008. 111:723–731.
7. Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav Res Methods. 2009. 41(4):1149–1160.

8. Ham YL. Development and evaluation of a simulation educational program using a high-fidelity patient simulator for undergraduate nursing students. 2009. Seoul: Yonsei University;Unpublished doctoral dissertation.
9. Hur HK, Choi HO, Jung JS, Kang HW, Kim GY. Influence of simulation-based practice on emergency care for patients with dyspnea on learning outcomes in nursing students. J Korean Crit Care Nurse. 2012. 5(1):12–22.
10. Kim IO, Park CS. Current status of clinical practice education in maternity nursing in Korea - four-year course nursing schools centered. Korean J Women Health Nurs. 2006. 12(1):12–21.
11. Kim Y, Chun N, Lee EH, Cho IS, Ahn S, Kim J, et al. Student experience and satisfaction with clinical nursing practice in women's health nursing. Korean J Women Health Nurs. 2011. 17(3):225–242. http://dx.doi.org/10.4069/kjwhn.2011.17.3.225.

12. Kim YM, Park YS, Chung CW, Kim M. Application of problem-based learning(PBL) for students' practice in maternity nursing. Korean J Women Health Nurs. 2006. 12(4):326–337.

13. Larew C, Lessans S, Spunt D, Foster D, Covington BG. Innovations in clinical simulation: Application of Benner's theory in an interactive patient care simulation. Nurs Educ Perspect. 2006. 27(1):16–21.
14. Lee JH, Choi M. Evaluation of effects of a clinical reasoning course among undergraduate nursing students. Korean J Adult Nurs. 2011. 23(1):1–9.
15. Lee JH, Kim S, Yeo K, Cho SJ, Kim HL. Experiences among undergraduate nursing students on high-fidelity simulation education: A focus group study. J Korean Acad Soc Nurs Educ. 2009. 15(2):183–193. http://dx.doi.org/10.5977/JKASNE.2009.15.2.183.

16. Lee SE. Evaluation of the standardized patients managed instruction for a clinical maternity nursing course. J Korean Acad Soc Nurs Educ. 2011. 17(1):14–24. http://dx.doi.org/10.5977/JKASNE.2011.17.1.014.
17. Lee WS, Cho KC, Yang SH, Roh YS, Lee GY. Effects of problem-based learning combined with simulation on the basic nursing competency of nursing students. J Korean Acad Fundam Nurs. 2009. 16(1):64–72.
18. Lee WS, Kim M. Effects and adequacy of high-fidelity simulation-based training for obstetrical nursing. J Korean Acad Nurs. 2011. 41(4):433–443. http://dx.doi.org/10.4141/jkan.2011.41.4.433.

19. Medley CF, Horne C. Using simulation technology for undergraduate nursing education. J Nurs Educ. 2005. 44(1):31–34.

20. Shin Y, Hur HK, Park SM, Song H, Kim GY. Development of an integrated clinical nursing practice course for improvement of nursing competency among nursing students. J Korean Acad Soc Nurs Educ. 2007. 13(1):32–40.
21. Yang J. The effects of a simulation-based education on the knowledge and cinical competence for nursing students. J Korean Acad Soc Nurs Educ. 2012. 18(1):14–24. http://dx.doi.org/10.5977/jkasne.2012.18.1.014.
22. Yang J, Park M. The relationship of clinical competence and self-directed learning in nursing students. J Korean Acad Soc Nurs Educ. 2004. 10(2):271–277.
23. Yoo MS. Development of standardized patient managed instruction for a fundamentals of nursing course. 2001. Seoul: Yonsei University;Unpublished doctoral dissertation.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download