Abstract
Purpose
The purpose of this study was to determine whether upright position is effective in labor through systematic review in randomized controlled trials.
Methods
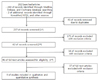
We established the PICO (Patient-Intervention-Comparator-Outcome) strategy, and reviewed 282 literatures from national and international electronic databases, and finally selected 9 references based on inclusion and exclusion criteria. We evaluated the quality of references and carried out a meta-analysis.
Results
The maternal outcomes showed that the duration of their second-stage labor was 2.29 minutes shorter than that of the women in the recumbent position, and were less likely to have episiotomy. The other outcomes, including the mode of delivery, blood loss, hemoglobin level, use of oxytocin, use of analgesics, and perineal laceration, did not differ between the groups. The fetal heart rate abnormality occurred less than in the control group. The Apgar scores of the groups did not differ.
Figures and Tables
Table 1
Characteristics selected in 9 Studies (N=9)
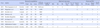
Int.=intervention group; Cont.=Control group; SL=stage of labor; MD=modee of delivery; BL=Blood loss; HL=Hemoglobin level; Oxy.=Oxytocin; Anal.=analgesics; PL=Perineal laceration; FH=fetal heart; NO=neonatal outcomes; Eiv.=evidence; UPPI=upright position with providing information; HKP=hands and knees position; SSP=supported sitting position; SP=sitting position; RSA=Republic of South Africa; UP=upright position; UAP=upright, ambulatory position; ASP=ambulatory, squatting position.
Summary Statement
▪ What is already known about this topic:
Supine position in labor may have adverse physiological effects on the condition of the woman and her baby and on the progression of labor.
▪ What this paper adds:
There is evidence that an mother's upright position in the second stage of labor reduces incidence of length of the second stage of labor, episiotomy, and an abnormal fetal heart rate.
▪ Implications for practice, education, and policy
These results have important implications for the development of nurse's active role and nursing intervention in normal vaginal delivery.
References
1. Allahbadia GN, Vaidya PR. Squatting position for delivery. J Indian Med Assoc. 1993. 91:13–16.
2. Altman D, Ragnar I, Ekström A, Tydén T, Olsson SE. Anal sphincter lacerations and upright delivery postures- a risk analysis from a randomized controlled trial. Int Urogynecol J Pelvic Floor Dysfunct. 2007. 18:141–146. http://dx.doi.org/10.1007/s00192-006-0123-9.
3. Baek MH, Chun SH, Lee SJ, Kim YJ, Choi JH, Park MI, et al. Computerized analysis of fetal heart rate in normal term pregnant women categorized by birth weight and fetal sex. Korean J Perinatol. 2008. 19:142–149.
4. Bidwell S, Jensen MF. Using a search protocol to identify sources of information: The COSI model. 2004. Bethesda, MD: National Information Center on Health Services Research and Health Care Technology, US National Library of Medicine.
5. Bomfim-Hyppólito S. Influence of the position of the mother at delivery over some maternal and neonatal outcomes. Int J Gynaecol Obstet. 1998. 63:Suppl 1. S67–S73. http://dx.doi.org/10.1016/S00207292(98)00186-6.

6. Cho WB. An experimental study on the effects of nursing care according to change of position during labor. J Nurs Acad Soc. 1978. 8:139–151.

7. de Jong PR, Johanson RB, Baxen P, Adrians VD, van der Westhuisen S, Jones PW. Randomised trial comparing the upright and supine positions for the second stage of labour. Br J Obstet Gynaecol. 1997. 104:567–571. http://dx.doi.org/10.1111/j.1471-0528.1997.tb11534.x.
8. de Jonge A, van Diem M, Scheepers P, van der Pal-de Bruin K, Lagro-Janssena A. Increased blood loss in upright birthing positions originates from perineal damage. BJOG. 2007. 114:349–355. http://dx.doi.org/10.1111/j.1471-0528.2006.01210.x.

9. Downe S, Gerrett D, Renfrew MJ. A prospective randomised trial on the effect of position in the passive second stage of labour on birth outcome in nulliparous women using epidural analgesia. Midwifery. 2004. 20:157–168. http://dx.doi.org/10.1016/S0266-6138(03)00052-4.

10. Gupta JK, Nikodem C. Maternal posture in labour. Eur J Obstet Gynecol Reprod Biol. 2000. 92:273–277. http://dx.doi.org/10.1016/S0301-2115(99)00272-9.

11. Gupta JK, Hofmeyr GJ, Smyth R. Position in the second stage of labour for women without epidural anaesthesia. Cochrane Database Syst Rev. 2012. 05. 16. 5:CD002006.

12. Higgins J, Green S, editors. The Cochrane Collaboration. Cochrane handbook for systematic reviews of interventions version 5.1.0. 2011. Retrieved March 30, 2011. from http://www.cochrane-handbook.org.
13. Hur MH, Han SH. Clinical trial of aromatherapy on postpartum mother's perineal healing. J Korean Acad Nurs. 2004. 34:53–62.

14. Kim GJ, Kim SY, Yun SJ, Lee SP, Choe YD, Lee UD. Aortic compression to control massive postpartum hemorrhage. Korean J Obstet Gynecol. 2003. 46:1577–1584.
15. Kim HS. The comparison of perception of birth experience to women who had a traditional delivery and those who selected their type of delivery. 2003. Seoul: Ewha Womans University;Unpublished doctoral dissertation.
16. Kim SK, Kim YK, Cho AJ, Kim HR, Lim SE. The 2009 National Survey on Fertility, Family Health and Welfare in Korea. 2009. Seoul: Korea Institute for Health and Social Affairs.
17. Lawrence A, Lewis L, Hofmeyr GJ, Dowswell T, Styles C. Maternal positions and mobility during first stage labour. Cochrane Database Syst Rev. 2009. 15(2):CD003934.

18. MacLennan AH, Crowther C, Derham R. Does the option to ambulate during spontaneous labour confer any advantage or disadvantage? J Matern Fetal Med. 1994. 3:43–48.

19. Miquelutti MA, Cecatti JG, Makuch MY. Upright position during the first stage of labor: A randomised controlled trial. Acta Obstet Gynecol Scand. 2007. 86:553–558. http://dx.doi.org/10.1080/00016340601185251.

20. Nam JH, Sung KW, Jeong WY, Lee KY, Kang SW. Comparison for second stage of labor and perinatal outcomes between birth chair and recumbent position. Paper presented at fall conference of Korean Society of Obstetrics & Gynecology. 1990. 132.
21. Park MI, Lee WJ, Lee CH, Kim KD, Yun MK, Park YS, et al. Multivariate analysis of variables affecting on fetal heart rate. Korean J Obstet Gynecol. 1999. 42:1769–1776.
22. Scottish Intercollegiate Guidelines Network. Methodology checklist 2: Controlled trials. 2004. Retrieved January 20, 2010. from http://www.sign.ac.uk/methodology/checklists.html.
23. Seo K, Kim M. Guidelines for preconception care: from the maternal and child health perspectives of Korea. J Korean Med Assoc. 2011. 54:845–850. http://dx.doi.org/10.5124/jkma.2011.54.8.845.

24. Stremler R, Hodnett E, Petryshen P, Stevens B, Weston J, Willan AR. Randomized controlled trial of handsand-knees positioning for occipitoposterior position inlabor. Birth. 2005. 32:243–251. http://dx.doi.org/10.1111/j.0730-7659.2005.00382.x.
25. Thies-Lagergren L, Kvist LJ, Christensson K, Hildingsson I. No reduction in instrumental vaginal births and no increased risk for adverse perineal outcome in nulliparous women giving birth on a birth seat: Results of a Swedish randomized controlled trial. BMC Pregnancy Childbirth. 2011. 11:22. http://dx.doi.org/10.1186/1471-2393-11-22.

26. Waldenström U, Gottvall K. A randomized trial of birthing stool or conventional semirecumbent position for second-stage labor. Birth. 1991. 18:5–10. http://dx.doi.org/10.1111/j.1523-536X.1991.tb00045.x.

27. Zwelling E. The Emergence of High-Tech Birthing. J Obstet Gynecol Neonatal Nurs. 2008. 37:85–93. http://dx.doi.org/10.1111/j.1552-6909.2007.00211.x.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download