Abstract
Purpose
The purpose of this study was to evaluate the effects of clinical practice and simulation-based practice for obstetrical nursing in terms of self-efficacy, practice satisfaction, and practice stress.
Methods
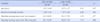
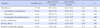
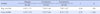
A non-equivalent control group post test design was used. The participants were 171 junior nursing students, 103 in the experimental group, and 68 in the control group. Simulation-based practice consisted of nursing assessment during labor, nursing assessment and intervention for normal and high risk mother, nursing education for mother and family during labor, and open lab. The experimental group participated in simulation-based practice for two days and the control group participated in clinical practice at delivery room for two weeks.
Figures and Tables
Summary Statement
▪ What is already known about this topic?
Simulation-based practice was useful in improving self-confidence and students expressed satisfaction with simulation-based practice.
▪ What this paper adds?
Simulation-based practice group showed higher level of self-efficacy and satisfaction than clinical practice group. Practice stress was also higher in simulation-based practice group than clinical practice group.
▪ Implications for practice, education and/or policy
The effects of Simulation-based practice for obstetrical nursing should be compared to clinical practice. Strategies to reduce stress level of simulation-based practice was needed.
References
1. Alinier G, Hunt B, Gordon R, Harwood C. Effectiveness of intermediate-fidelity simulation training technology in undergraduate nursing education. J Adv Nurs. 2006. 54:359–369. http://dx.doi.org/10.1111/j.1365-2648.2006.03810.x.

2. Baillie L, Cruzio J. Students' and facilitators' perceptions of simulation in practice learning. Nurse Educ Pract. 2009. 9:297–306. http://dx.doi.org/10.1016/j.nepr.2008.08.007.

3. Chang S, Kwon E, Kwon YO, Kwon HK. The effects of simulation training for new graduate critical care nurses on knowledge, self-efficacy, and performance ability of emergency situation at intensive care unit. J Korean Acad Adult Nurs. 2010. 22:375–383.
4. Choi JY. Simulation based education as an educational strategy for nursing students. Chonnam J Nurs Sci. 2010. 15(1):47–57.
5. Chung CW, Kim HS, Park YS. Effects of high-fidelity simulation-based education on maternity nursing. Perspect Nurs Sci. 2011. 8(2):86–96.
6. Corbridge SJ, McLaughlin R, Tiffen J, Wade L, Templin R, Corbridge TC. Using simulation to enhance knowledge and confidence. Nurse Pract. 2008. 33(6):12–13.
7. Dayal AK, Fisher N, Magrane D, Goffman D, Bernstein PS, Katz NT. Simulation training improves medical students' learning experiences when performing real vaginal deliveries. Simul Healthc. 2009. 4:155–159. http://dx.doi.org/10.1097/SIH.0b013e3181b3e4ab.

8. Haskvitz LM, Koop EC. Students struggling in clinical? a new role for the patient simulator. J Nurs Educ. 2004. 43:181–184.

9. Hodge M, Martin CT, Tavernier D, Perea-Ryan M, Alcala-Van Houten L. Integrating simulation across the curriculum. Nurse Educ. 2008. 33:210–214. http://dx.doi.org/10.1097/01.NNE.0000312221.59837.38.

10. Hofmann B. Why simulation can be efficient: On the preconditions of efficient learning on complex technology based practice. BMC Med Educ. 2009. 9:48. http://dx.doi.org/10.1186/1472-6920-9-48.

11. Holmstrom SW, Downes K, Mayer JC, Learman LA. Simulation training in an obstetric clerkship: A randomized controlled trial. Obstet Gynecol. 2011. 118:649–654. http://dx.doi.org/10.1097/AOG.0b013e31822ad988.
12. Jude DC, Gilbert GG, Magrane D. Simulation training in the obstetrics and gynecology clerkship. Am J Obstet Gynecol. 2006. 195:1489–1492. http://dx.doi.org/10.1016/j.ajog.2006.05.003.

13. Kim YH, Jang KS. Effects of a simulation-based education on cardio-pulmonary emergency care knowledge, clinical performance ability and problem solving process in new nurses. J Korean Acad Nurs. 2011. 41:245–255. http://dx.doi.org/10.4040/jkan.2011.41.2.245.
14. Kim Y, Chun NM, Lee EH, Cho IS, Ahn SH, Kim JI, et al. Student experience and satisfaction with clinical nursing practice in women's health nursing. Korean J Women Health Nurs. 2011. 17:225–242. http://dx.doi.org/10.4069/kjwhn.2011.17.3.225.

15. Korean Society of Women Health Nursing. Learning objectives of maternity nursing. 2009. Seoul: Korean Society of Women Health Nursing.
16. Larew C, Lessans S, Spunt D, Foster D, Covington BG. Innovations in clinical simulation: Application of Benner's theory in an interactive patient care simulation. Nurs Educ Perspect. 2006. 27:16–21.
17. Lasater K. High-fidelity simulation and the development of clinical judgement: Student's experience. J Nurs Educ. 2007. 46:269–276.
18. Lee JH, Kim SS, Yeo KS, Cho SJ, Kim HL. Experience among undergraduate nursing students on high-fidelity simulation education: A focus group study. J Korean Acad Soc Nurs Educ. 2009. 15:183–193. http://dx.doi.org/10.5977/JKASNE.2009.15.2.183.
19. Lee MS, Hahn SW. Effect of simulation-based practice on clinical performance and problem solving process for nursing students. J Korean Acad Soc Nurs Educ. 2011. 17:226–234. http://dx.doi.org/10.5977/JKASNE.2011.17.2.226.

20. Lee SJ, Roh YS, Kim JO, Jang KI, Ryoo EN, Park YM. Comparison of multi-mode simulation and SimMan® simulation on evaluation of nursing care for patients with dyspnea. J Korean Acad Soc Nurs Educ. 2010. 16:51–60. http://dx.doi.org/10.5977/JKASNE.2010.16.1.051.
21. Lee SO, Eom MR, Lee JH. Use of simulation in nursing education. J Korean Acad Soc Nurs Educ. 2007. 13:90–94.
22. Lee WS, Kim MO. Effects and adequacy of high-fidelity simulation-based training for obstetrical nursing. J Korean Acad Nurs. 2011. 41:433–443. http://dx.doi.org/10.4040/jkan.2011.41.4.433.

23. Liaschenko J, Peter E. Nursing ethics and conceptualizations of nursing: Profession, practice and work. J Adv Nurs. 2004. 46:488–495. http://dx.doi.org/10.1111/j.1365-2648.2004.03011.x.

24. Lim KC. Directions of simulation-based learning in nursing practice education: A systematic review. J Korean Acad Soc Nurs Educ. 2011. 17:246–256. http://dx.doi.org/10.5977/JKASNE.2011.17.2.246.

25. Nehring WM, Lashley FR. Current use and opinions regarding human patient simulators in nursing education: An international survey. Nurs Educ Perspect. 2004. 25:244–248.
26. Park JH, Jung E, Ko JK, Yoo HB. Delivery training for undergraduate medical students using birth simulator. Korean J Obstet Gynecol. 2008. 51:950–956.
27. Reynolds A, Ayres-de-Campos D, Bastos LF, van Meurs WL, Bernardes J. Impact of labor and delivery simulation classes in undergraduate medical learning. Med Educ Online. 2008. 13:14. http://dx.doi.org/10.3885/meo.2008.Res00285.

28. Seong KY. Effects of practice nursing education: Using standardized patients on subcutaneous insulin injection. 2008. Daejeon: Eulji University;Unpublished master's thesis.
29. Yang JJ. Development and evaluation of a simulation-based education course for nursing students. J Korean Acad Adult Nurs. 2008. 20:548–560.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download