This article has been
cited by other articles in ScienceCentral.
Abstract
A 71-year-old man with acute basilar artery occlusion was referred for endovascular treatment 6 hours after the onset of stroke with a Glasgow Coma Score of 3 and National Institutes of Health Stroke Scale of 27. A cerebral arteriogram revealed occlusion of the left vertebral artery proximally and thromboembolic occlusion of the basilar tip. Direct aspiration and mechanical thrombectomy with various stent retrievers failed to reconstitute arterial flow in the basilar artery. Thrombolysis in cerebral infarction 2b recanalization was achieved only after placement of double Catch Mini stent retrievers through 2 microcatheters, on both side branches of the basilar bifurcation in a kissing fashion and retrieving them simultaneously. It was possible to perform this maneuver through a single distal access catheter without any complications. On follow-up the patient awakened and was able to follow commands on his right side. To our knowledge, dual mechanical thrombectomy with stent retrievers has not been reported in the posterior circulation previously. This technique may be useful in retrieving thrombi located at major intracranial bifurcations of the posterior circulation which do not recanalize with standard mechanical thrombectomy procedures. Although bilateral access to the basilar artery through both vertebral arteries is an advantage in posterior circulation for this technique, dual mechanical thrombectomy can also be performed through a unilateral access.
Go to :

Keywords: Endovascular procedures, Intracranial embolism and thrombosis, Thrombectomy, Thrombolytic therapy, Stroke, Basilar artery
INTRODUCTION
In a significant number of acute occlusions of a large anterior circulation artery
9) and in approximately 20% of acute stroke cases secondary to thromboembolic occlusion of the basilar artery (BA), it is not possible to achieve thrombolysis in cerebral infarction (TICI) 2b/3 flow with endovascular treatment.
1)8) Dual mechanical thrombectomy using 2 stent retrievers simultaneously for the treatment of acute anterior circulation has been recently described.
5) This is the first reported case of dual mechanical thrombectomy demonstrating successful retrieval of resistant thrombus located within the posterior circulation.
Go to :

CASE REPORT
A 71-year-old man was referred to us 6 hours after losing consciousness with a Glasgow Coma Score of 3 and National Institutes of Health Stroke Scale (NIHSS) of 27. His pertinent medical and surgical history included chronic atrial fibrillation, congestive heart failure, hypertension and diabetes. Cranial computed tomography (CT) angiography showed occlusion of the left vertebral artery (VA), the distal third of the BA, the proximal posterior cerebral arteries (PCAs) and the superior cerebellar arteries (SCAs). Intravenous tissue plasminogen activator had not been started due to delayed presentation, and mechanical thrombectomy was requested at 7 hours after the onset of symptoms. Due to the premorbid condition of the patient, we proceeded with mechanical thrombectomy.
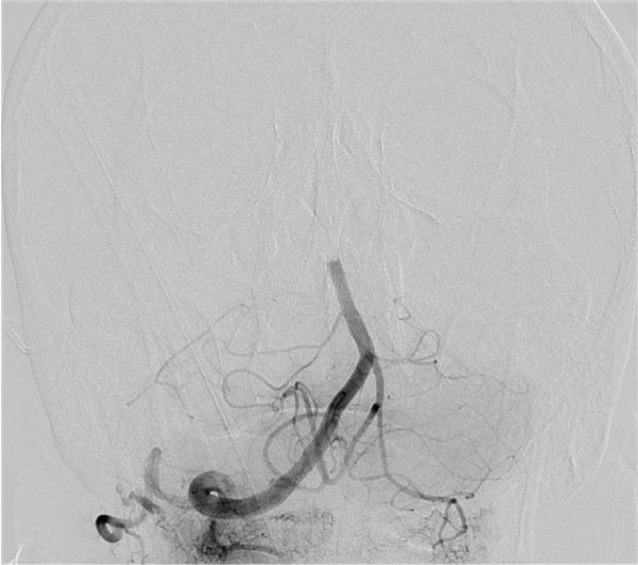
A cerebral angiogram was performed via a 6F 65 cm Destination sheath (Terumo, Tokyo, Japan) under general anesthesia and systemic heparinization. The angiogram revealed total occlusion of the distal BA without opacification of PCAs and SCAs bilaterally (
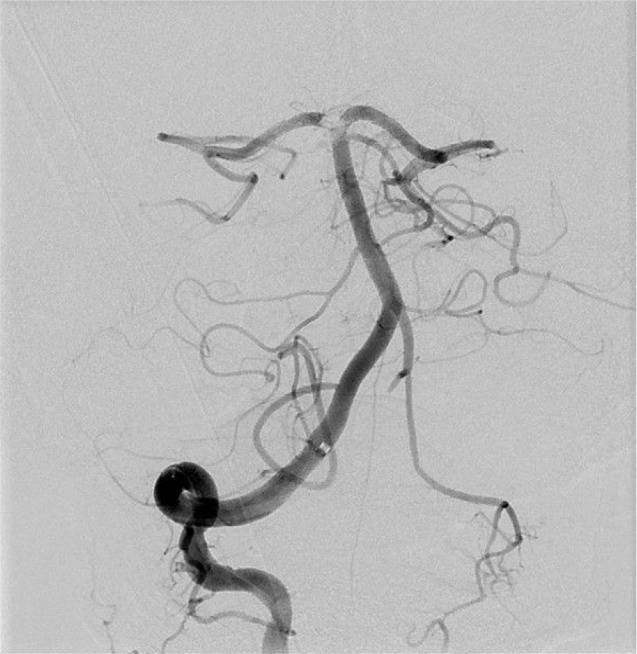
Fig. 1). The left VA did not opacify proximally suggesting severe hypoplasia or thrombotic occlusion. The left V4 segment and the left posterior inferior cerebellar artery (PICA) were supplied retrogradely from the BA. A DAC 057 (Concentric Medical, Mountain View, CA, USA) catheter was used to catheterize the right V4 segment. Further access into the BA for thromboaspiration was attempted but secondary to arterial tortuosity, this was not possible by direct advancement of DAC 57 over a Vasco 21 microcatheter (Balt, Montmorency, France) or by using coaxial system composed of an innermost Prowler Select Plus catheter (Codman Neurovascular, Raynham, MA, USA) placed through a DAC 38 catheter (Concentric Medical, Mountain View, CA, USA), which in turn, was placed within the DAC 57 catheter. Consequently, the tip of the DAC 57 catheter was left at the V4 segment and the Vasco-21 microcatheter was navigated over a Synchro 14 wire (Boston Scientific, Natick, MA, USA) to traverse the thrombus and navigate the microcatheter into the right PCA. Mechanical thrombectomy was performed with a Revive stent retriever (Codman Neurovascular) deployed from the right P2-P3 junction proximally to the midbasilar artery. Thrombectomy was repeated 2 more times with the same device, 2 times with another Revive device and finally 2 times with a Catch Mini Plus thrombectomy device (Balt) deployed through an Echelon 10 microcatheter (ev3 Endovascular, Plymouth, MN, USA). Thrombectomies were performed by accessing both PCAs in a consecutive manner and resulted in TICI 2b flow but a persistent clot was still present at the top of the BA, and the right SCA remained occluded (
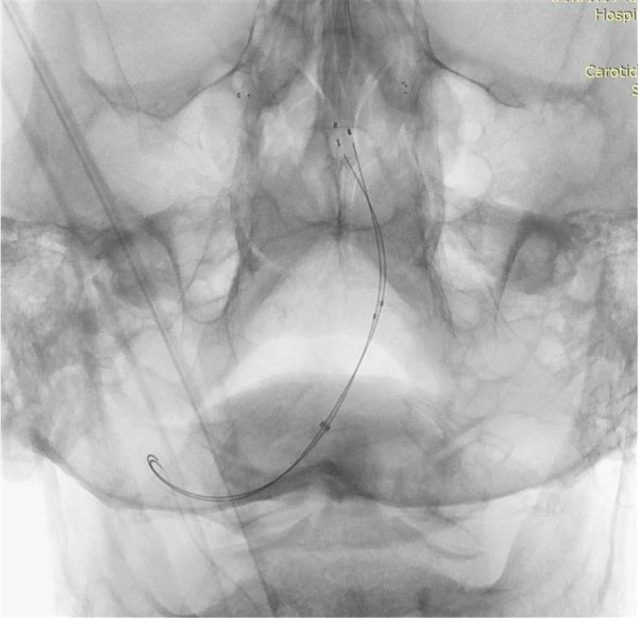
Fig. 2). Finally, two Echelon 10 microcatheters were placed through the DAC 57 catheter and both PCAs were accessed. Two Catch Mini devices were placed through these microcatheters extending from PCAs proximally to the BA in a kissing fashion (
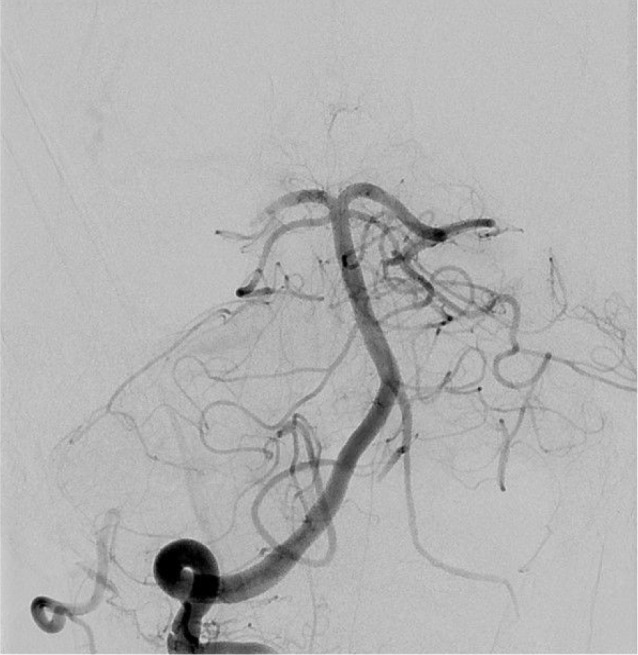
Fig. 3). Both stent retrievers were pulled back simultaneously, and the thrombus was confined between the devices similar to a nut in a nutcracker. Post-procedure angiogram showed complete recanalization of the BA and proximal PCAs (
Fig. 4). There was distal embolic occlusion of the right distal PCA, which we decided not to treat intra-arterially. A flat panel CT scan obtained immediately post-procedure was negative for intracranial hemorrhage. Needle-to-recanalization time was 90 minutes.
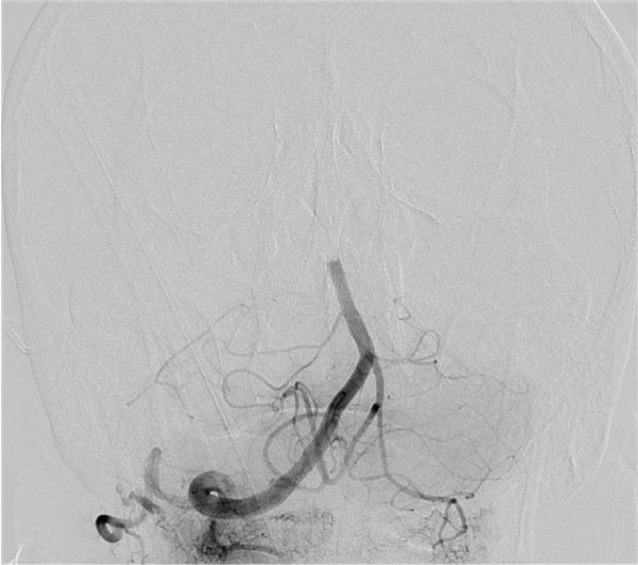 | Fig. 1Anteroposterior view of the digital subtraction angiogram revealing total occlusion of the distal third of the basilar artery without opacification of the posterior cerebral and superior cerebellar arteries bilaterally.
|
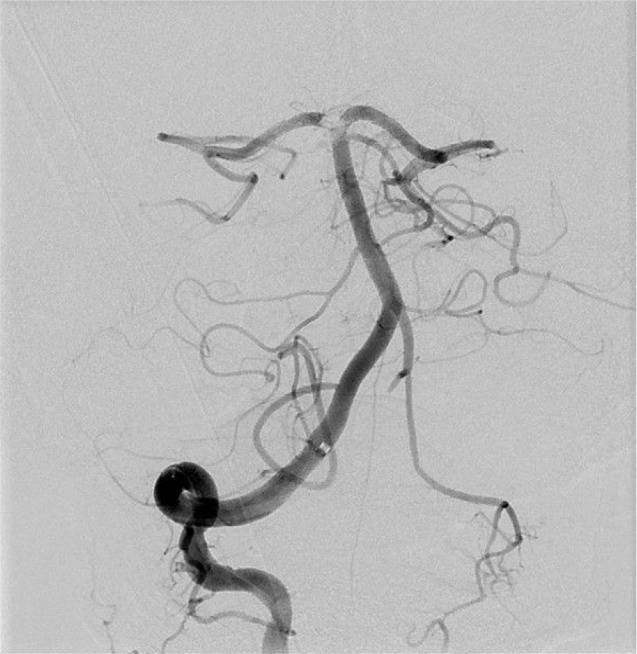 | Fig. 2Anteroposterior view following multiple thrombectomy attempts with a single stent retriever reveal a residual clot persisting at the bifurcation of the basilar artery that was impeding blood flow.
|
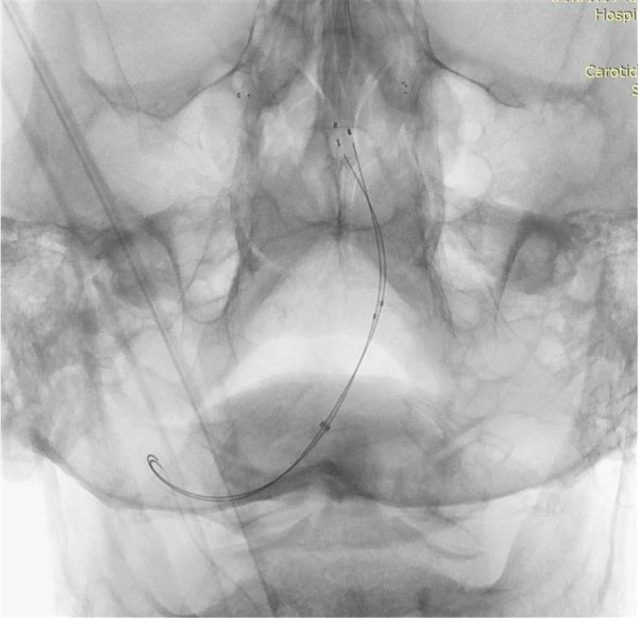 | Fig. 3Native image of the angiogram in anteroposterior view showing two Catch Mini devices (placed simultaneously) extending from the posterior cerebral arteries to the midbasilar segment.
|
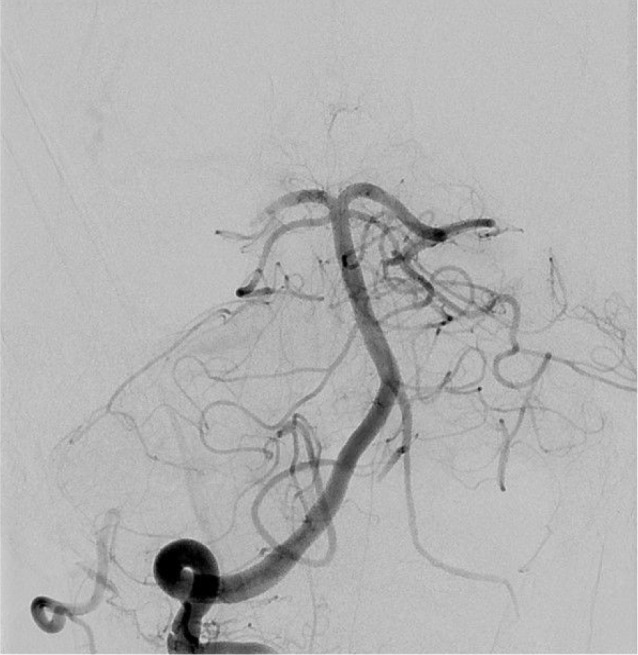 | Fig. 4Post-procedure angiogram after simultaneous retrieval of both stent retrievers demonstrates patency of the basilar artery, superior cerebellar arteries and left posterior cerebral artery. Occlusion of the distal right posterior cerebral artery and the left superior cerebellar arteries were due to clot fragmentation.
|
The patient was weaned off of sedation during the following week. Follow-up magnetic resonance imaging studies were remarkable for a territorial infarction of the right occipital lobe, a segmental infarction in the left cerebellar hemisphere and a wedge-shaped right pontine infarction. His inpatient course was complicated by repetitive bouts of infections and critical illness neuromyopathy. At the time of discharge, the patient was awake and able to obey verbal commands; his discharge NIHSS was 21, but the examination was confounded by the underlying neuromyopathy, which together with the deficits associated with stroke, leaved the patient in a quadriparetic and bed-ridden state. Ten months later, the patient was admitted to our hospital secondary to acute deterioration of his general clinical condition associated with a generalized skin rash. He expired 3 days later due to sepsis; the origin of the infection remains unknown.
Go to :

DISCUSSION
Among the 3 types of treatments of acute ischemic stroke (mechanical thrombectomy, intravenous thrombolysis and intra-arterial thrombolysis), mechanical thrombectomy has the highest recanalization rate for posterior circulation and anterior circulation acute large artery occlusions (around 80% and 90% respectively).
1)8) In the anterior circulation, mechanical thrombectomy has become a standard of care.
7) Although the effect of recanalization on clinical outcomes in the posterior circulation remains to be proven, endovascular treatment is typically attempted based on the grim prognosis up to 48 hours after symptoms.
1)2) Acceptable morbidity and mortality with 75–100% recanalization rates can be achieved with various mechanical thrombectomy/thromboaspiration devices.
7)8)
However, sometimes due to a snagging-like phenomenon, thrombi located in major arterial bifurcations may be difficult or impossible to retrieve with a single stent retriever device during mechanical thrombectomy.
4) Occasionally, creative techniques have to be performed to achieve recanalization for these unrelenting occlusions. For example, a two-catheter technique utilizing sequential withdrawal of bilaterally placed Merci devices (Concentric Medical) with bilateral proximal vertebral occlusion has been utilized to achieve basilar patency.
1) Similarly, a case series demonstrated dual stent retriever thrombectomy (DST) is feasible and appears to be safe in the anterior circulation.
5) Dual mechanical thrombectomy has not been reported in the posterior circulation in the literature previously to our knowledge.
In the previously reported series describing DST, the technique of device placement had to be modified when distal access catheters (DAC) were used. Since 2 large-bore microcatheters (with 0.021 to 0.026 inch luminal diameter) would not fit through a single distal access catheter, the authors had to remove the first microcatheter totally after deploying the first stent retriever, to make room for the second microcatheter within the DAC. They had to place the devices in a “T” configuration to prevent placement of the second device through the struts of the first device since it was not possible to place the devices simultaneously. Unlike this previous report we used a newer stent retriever that can be navigated through a small-caliber (inner lumen 0.0165 inch) microcatheter and this permits simultaneous placement of both microcatheters through a single distal access catheter/intracranial aspiration catheter. As a result, placement of stent retrievers in not only a “T” configuration but also in a “double-barrel Y” fashion is possible through aspiration catheters (such as 5 MAX ACE, Penumbra, Alameda, CA, USA or DAC 57, Concentric Medical). In the previous report, such a “parallel Y” thrombectomy was only possible with the use a proximal balloon-tip guide catheter instead of a DAC. These balloon-tip guide catheters are useful in the anterior circulation secondary to the absence of prominent collaterals to the cervical internal carotid artery. On the other hand due to the persistence of antegrade blood flow through the contralateral VA or frequent occurrence of ipsilateral cervical collaterals when it the VA is proximally occluded, thrombectomy techniques based on unilateral or bilateral proximal occlusion are likely to be less successful in the posterior circulation. Besides, many operators prefer a trial of direct clot aspiration and if necessary, continue with stent retrievers in both anterior and posterior circulation acute stroke treatments.
3)6) Such a combination invariably necessitates a DAC and is feasible for dual thrombectomy with the materials and technique described. Dual thrombecomy may be used as a potentially life-saving procedure in the posterior circulation when basilar thrombectomy with aspiration thrombectomy or conventional single-device mechanical thrombectomy fails.
Go to :

CONCLUSION
Dual thrombectomy may be utilized in acute posterior circulation thrombotic occlusions. It is possible to perform the technique using a distal access catheter through a unilateral VA approach.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download