Abstract
Unruptured cerebral aneurysms sometimes present with visual symptomsdue to compression of the visual pathways. However, until now, unruptured anterior communicating artery (ACoA) aneurysms presenting visual field defects have been extremely rare. The authors report the case of a 51-year-old woman who presented with left homonymous hemianopsia. Radiological findings demonstrated an ACoA aneurysm filled with thrombus, that was compressing the optic chiasm and post-chiasmal tract. The patient underwent clipping of the aneurysm, which resolved the visual field defect. In cases of visual field defects, an ACoA aneurysm should be included in the differential diagnosis.
Most cerebral aneurysms show no apparent symptom until ruptured, but some manifest clinical symptoms by compressing the brain tissue. Notably, several reports described cerebral aneurysms presenting with visual dysfunction caused by compression of the visual pathways, and these aneurysms commonly arise from the cavernous, ophthalmic and supra-clinoid segments of internal carotid artery.3)9)12) However, an unruptured aneurysm of anterior communicating artery (ACoA) is a highly unusual cause of visual dysfunction.3)6)11) Therefore, we report a case of an unruptured ACoA aneurysm presenting with homonymous hemianopsia, and review the relevant literature.
A 51-year-old woman, without any history of medical illness, presented with a 2-day history of headache and visual field defect. Laboratory data and neurological examination results on admission were unremarkable. Static visual field tests showed left homonymous hemianopsia (Fig. 1A, B). A computerized tomographic angiogram of the brain revealed a 12 × 10 mm unruptured saccular aneurysm arising from the right side of the ACoA. Magnetic resonance (MR) imagingshowed a partially thrombosed aneurysm of the ACoA compressing the optic chiasm and postchiasmatic optic tract. On T2-weighted fluid-attenuated inversion recovery (FLAIR) MR imaging, the right post-chiasmal optic tract showed high signal intensity suggesting compressive neuropathy (Fig. 2). An internal carotid angiography confirmed the presence of a 11 × 4 × 2 mm thrombosed saccular aneurysm, projecting posteroinferiorly with a neck of 1.7 mm (Fig. 3). A right frontotemporal craniotomy and trans-Sylvian approach were performed. A neck of the ACoA aneurysm, and the bilateral A1 and A2 segments of the anterior cerebral artery were identified (Fig. 4). The patient underwent neck clipping of the ACoA aneurysm. Postoperatively, the patient noted improvement of her headache and visual field loss (Fig. 1C, D).
symptom, the incidence of internal carotid (IC) aneurysm is relatively high. Date et al.3) reported that IC-ophthalmic aneurysms had a 25% incidence rate, IC-cavernous aneurysms had a 21% incidence rate and ACoA aneurysms had only a 1% incidence rate. We found a total of 14 cases of unruptured ACoA aneurysms presenting with visual dysfunction in our review.1)5)10)12) The reason why ACoA aneurysms rarely present with visual symptom is that these types of aneurysms tend to rupture in an early stage, so the occurrence of a large or giant aneurysm which can compress the optic nerve is extremely rare.11)12) In the literature, unruptured ACoA aneurysms with visual symptoms were generally large, as in the current case.1)3)5)10) Visual symptoms include visual field defects and reduced visual acuity. The symptoms vary widely, so there was no typical clinical presentation identified in the literature.1)3)5)10)
Based on the previous research, there are two possible mechanisms to explain the visual dysfunction caused by a cerebral aneurysm. First, visual symptoms might be related to the direct compression of visual pathways by a large or giant aneurysm arising from the internal carotid artery or the anterior part of the Circle of Willis.3)11)12) Second, poor blood circulation caused by occlusion or distortion of the ophthalmic artery or of small arteries that are responsible for the blood supply of the chiasma can also cause such visual symptoms.3)12) Recovery of visual function can be expected when surgical treatment is performed before the visual dysfunction becomes irreversible.3) According to the literature, treatment within 3 to 8 months after the onset of symptoms demonstrated good visual outcomes.3)4) The present case had only two days between the onset of visual symptoms and surgical treatment. These previous studies suggest that early diagnosis and treatment of aneurysms that compress the visual pathway is important for preventing permanent visual loss.
In cases of endovascular treatment for large and giant intracranial aneurysms, volume expansion, which occurs secondary to thrombus formation, has been described in previous studies.2)13) Volume expansion can induce visual dysfunction by compressing the brain tissue.7)8) However, patients who underwent endovascular treatment for inoperable giant cerebral aneurysms with visual loss experienced improved visual outcomes compared with untreated patients.14) Therefore, endovascular treatment can be an alternative therapy when surgical treatment is not available.
In conclusion, we described a case of an ACoA aneurysm presenting with left homonymous hemianopsia. An unruptured ACoA aneurysm should be considered in the differential diagnosis of patients who experience visual dysfunction, though it is rare. In patients with visual dysfunction caused by an aneurysm, early diagnosis and surgical treatment appear to be important for obtaining a good visual outcome.
Figures and Tables
Fig. 1
Preoperative static visual field tests, right eye (A) and left eye (B), showing a left homonymous hemianopsia. Impovement of the visual fields in right eye (C) and left eye (D) at two months after surgery.

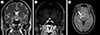
Fig. 2
(A, B) CoronalT2-weighted and T1-weighted with contrast images revealing a thrombosed aneurysm compressing the right side of the optic chiasm and postchiasmatic optic tract. (C) Axial T2-weighted FLAIR image showing the high signal intensity (arrow) of the right post-chiasmal optic tract.
References
1. Aoki N. Partially thrombosed aneurysm presenting as the sudden onset of bitemporal hemianopsia. Neurosurgery. 1988; 03. 22(3):564–566.

2. Carneiro A, Rane N, Küker W, Cellerini M, Corkill R, Byrne JV. Volume changes of extremely large and giant intracranial aneurysms after treatment with flow diverter stents. Neuroradiology. 2014; 01. 56(1):51–58.

3. Date I, Asari S, Ohmoto T. Cerebral aneurysms causing visual symptoms: their features and surgical outcome. Clin Neurol Neurosurg. 1998; 12. 100(4):259–267.

4. Ferguson GG, Drake CG. Carotid-ophthalmic aneurysms: visual abnormalities in 32 patients and the results of treatment. Surg Neurol. 1981; 07. 16(1):1–8.

5. Hagihara N, Abe T, Yoshioka F, Watanabe M, Tabuchi K. Photophobia as the visual manifestation of chiasmal compression by unruptured anterior communicating artery aneurysm. Case report. Neurol Med Chir (Tokyo). 2009; 04. 49(4):159–161.
6. Höök O, Norlén G. Aneurysms of the anterior communicating artery. Acta Neurol Scand. 1964; 09. 40(3):219–240.

7. La Pira B, Brinjikji W, Hunt C, Chen JJ, Lanzino G. Reversible edema-like changes along the optic tract following Pipeline-assisted coiling of a large anterior communicating artery aneurysm. J Neuroophthalmol. 2017; 06. 37(2):154–158.

8. McAuliffe W, Wycoco V, Rice H, Phatouros C, Singh TJ, Wenderoth J. Immediate and midterm results following treatment of unruptured intracranial aneurysms with the pipeline embolization device. AJNR Am J Neuroradiol. 2012; 01. 33(1):164–170.

9. Moteki Y, Kawamoto T, Namioka T, Yokote A, Kawamata T. Progressive visual field defect caused by an unruptured middle cerebral artery aneurysm. Clin Neurol Neurosurg. 2013; 10. 115(10):2182–2185.

10. Norwood EG, Kline LB, Chandra-Sekar B, Harsh GR 3rd. Aneurysmal compression of the anterior visual pathways. Neurology. 1986; 08. 36(8):1035–1041.

11. Park JH, Park SK, Kim TH, Shin JJ, Shin HS, Hwang YS. Anterior communicating artery aneurysm related to visual symptoms. J Korean Neurosurg Soc. 2009; 09. 46(3):232–238.

12. Peiris JB, Ross Russell RW. Giant aneurysms of the carotid system presenting as visual field defect. J Neurol Neurosurg Psychiatry. 1980; 12. 43(12):1053–1064.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download