Abstract
Objective
Surgical resection of thalamic and brainstem cerebral cavernous malformations (CCMs) is associated with significant operative morbidity, but it may be outweighed, in some cases, by the neurological damage from recurrent hemorrhage in these eloquent areas. The goals of this retrospective cohort study are to describe the technical nuances of surgical approaches and determine the postoperative outcomes for CCMs of the thalamus and brainstem.
Materials and Methods
We reviewed an institutional database of patients harboring thalamic or brainstem CCMs, who underwent surgical resection from 2010 to 2014. The baseline and follow-up neuroimaging and clinical findings of each patient and the operative details of each case were evaluated.
Results
A total of eight patients, including two with thalamic and six with brainstem CCMs, were included in the study cohort. All patients had progressive neurological deterioration from recurrent CCM hemorrhage, and the median modified Rankin Scale (mRS) at presentation was 3. The median CCM maximum diameter and volume were 1.7 cm and 1.8 cm3, respectively. The thalamic CCMs were resected using the anterior transcallosal transchoroidal and supracerebellar infratentorial approaches each in one case (13%). The brainstem CCMs were resected using the retrosigmoid and suboccipital trans-cerebellomedullary fissure approaches each in three cases (38%). After a median follow-up of 11.5 months, all patients were neurologically stable or improved, with a median mRS of 2. The rate of functional independence (mRS 0-2) was 63%.
Cerebral cavernous malformations (CCM) are commonly localized to deep regions of the brain, such as the thalamus and brainstem. Thalamic and brainstem CCMs account for approximately one-third of CCMs.41)42) The annual hemorrhage risk of these deep-seated CCMs has been reported, in some series, to be significantly higher than superficially located CCMs.57) Specifically, the hemorrhage risk of brainstem CCMs with a history of clinically overt hemorrhage may be as high as 20% per year.2) Due to the increased propensity for symptomatic CCMs to hemorrhage and the exquisitely sensitive nature of the thalamus and brainstem, intervention should be considered for appropriately selected lesions.24)38)
However, thalamic and brainstem CCMs present a significant surgical challenge, and are associated with relatively high rates of operative morbidity and mortality.41)58) While radiosurgery has been employed as a minimally invasive therapy for surgically unfavorable CCMs, the efficacy of this approach is controversial. Thus, surgery remains the gold standard of treatment for symptomatic CCMs which necessitate intervention. The aims of this retrospective cohort study are to (1) evaluate the technical aspects of common surgical approaches to CCMs of the thalamus and brainstem using specific case examples and (2) determine the postoperative outcomes for patients with thalamic and brainstem CCMs in the modern era.
We performed a retrospective evaluation of an institutional review board (IRB) approved database of CCM patients who underwent surgical management by the senior author (K.C.L.) at the University of Virginia from July 2010 to December 2014. The inclusion criteria were (1) CCM localization in the thalamus or brainstem and (2) sufficient data regarding baseline neurological status, intraoperative details, and postoperative outcomes. Patients with vascular malformations other than CCMs, such as cerebral arteriovenous malformations (AVM) and dural arteriovenous fistulas, were excluded.
The following baseline data were extracted from directed chart review: (1) patient attributes, (2) CCM characteristics, and (3) surgical details. The patient attributes were gender, age, presenting symptoms, and modified Rankin Scale (mRS) score at presentation. The CCM characteristics were size (maximum diameter and volume) and location. The surgical details were approach taken to access the lesion, use of supplementary localization techniques (e.g. electrophysiologic monitoring of neurological function, stereotactic neuronavigation), administration of intraoperative medications, and technical aspects of the surgical procedure, including patient positioning, skin incision, craniotomy or craniectomy, dural opening, intradural dissection, and CCM identification and resection.
Follow-up was classified as perioperative or longitudinal. Perioperative follow-up comprised all events from the end of surgery to hospital discharge, including postoperative complications, duration of hospital stay, discharge destination, and mRS at discharge. Longitudinal follow-up comprised all events from hospital discharge to the most recent clinical follow-up, including neuroimaging documentation of the absence of presence of residual CCM, mRS at last clinical follow-up, and duration of radiologic and clinical follow-up. The necessity for additional procedures after CCM resection was also noted for each patient.
A total of eight patients, two with thalamic CCMs (25%) and six with brainstem CCMs (75%), were included in the study cohort. The affected brainstem regions were the pons and medulla each in two patients (25%), and the midbrain and pontomesencephalic junction each in one patient (13%). Thin-slice (1 mm thickness) magnetic resonance imaging (MRI), T1-weighted with and without contrast and T2-weighted sequences, was performed for each patient. Based on the location of the lesion, the neurosurgeon (K.C.L.) decided on the surgical approach. Consideration was given to the accessibility of the lesion, closest pial border, operative corridor afforded by the approach, and morbidity of the approach. All patients presented with progressively worsening symptoms from mass effect after recurrent CCM hemorrhage. The median mRS at presentation was 3 (range 3 to 4). The median CCM maximum diameter and volume were 1.7 cm (range 1.1 to 2.8 cm) and 1.8 cm3 (range 0.6 to 8.7 cm3), respectively.
All surgical procedures were performed under general anesthesia, with the patient's head affixed in a three-point fixation Mayfield Skull Clamp System (Integra, Plainsboro, NJ, USA). After appropriate patient positioning for the planned surgical approach, the StealthStation (Medtronic, Minneapolis, MN, USA) frameless stereotactic neuronavigation system was registered with the patient's neuroimaging. Intraoperative electrophysiologic neurological monitoring of motor and somatosensory evoked potentials (MEP and SSEP, respectively) were utilized in all cases, and brainstem evoked potentials (BSEPs) were used for all brainstem CCMs. Near the time of skin incision and prior to dural opening, mannitol 1 gm/kg and dexamethasone 10 mg were administered, and hyperventilation to a PCO2 of 25 mmHg was performed to reduce brain swelling and intracranial pressure.
The operating microscope was routinely used for all intradural dissection, and both gross intraoperative findings and neuronavigation were used to identify a CCM's location. Afterwards, a combination of hemosiderin staining of the pial surface, when present, and surface anatomical landmarks were used, in conjunction with neuromonitoring, to determine the pial entry point for accessing the lesion. The dura was closed in a watertight fashion when possible, otherwise a dural substitute graft was sutured to the native dura to cover the dural defect. When a craniotomy was performed, the bone flap was plated back to the skull with titanium plates and screws. When a craniectomy was performed, a titanium mesh plate was placed over the cranial defect. Closure was performed in a standard layered fashion.
A 69 year-old female presented with several months of progressively worsening altered mental status and ataxia (mRS score 3 at presentation). MRI showed a 2.3 cm CCM in the right anterior medial thalamus (Fig. 1). We proceeded with surgical resection of the lesion via an anterior transcallosal transchoroidal approach. The patient was placed in a supine position, and a bicoronal skin incision was made. A left parasagittal craniotomy was performed, two-thirds anterior to the coronal suture. The dura covering the medial left frontal lobe was reflected medially over the superior sagittal sinus. We proceeded into the interhemispheric fissure to expose the dorsal surface of the corpus callosum.
A callosotomy was performed, located 1.5 cm posterior to the genu of the corpus callosum and measuring approximately 3 cm in length, in order to enter the lateral ventricle. We determined that we were in the right lateral ventricle, but the right foramen of Monro was obliterated by mass effect from the thalamic CCM. A septostomy was performed to facilitate cerebrospinal fluid (CSF) egress into the contralateral ventricle. After the anterior septal vein was coagulated and divided, the choroidal fissure of the right lateral ventricle, lateral to the fornix and medial to the choroid plexus, was opened in order to access the third ventricle. The CCM did not present to the ependymal surface and, thus, could not be readily visualized. The ependyma over the anterior medial thalamus was opened, and the CCM was immediately encountered. Due to the large size of the lesion, it was resected in a piecemeal fashion with standard microsurgical technique.
An external ventricle drain (EVD) was left in the third ventricle for 48 hours postoperatively. The patient had an uncomplicated postoperative course and was discharged from the hospital to an inpatient rehabilitation facility (mRS score 3 at discharge) on POD 10. Follow-up MRI, performed 5 months after surgery, showed a small residual CCM. At 11 months clinical follow-up, there was no evidence of postoperative intracranial hemorrhage, although the patient was neurologically unchanged, with a mRS score of 3.
A 50 year-old male presented with two months of progressively worsening headache, diplopia, and ataxia (mRS score 3 at presentation). MRI showed a 1.7 cm CCM in left posterior medial thalamus and midbrain (Fig. 2). We proceeded with surgical resection of the lesion via a supracerebellar infratentorial approach. The patient was placed in a prone position, with capital flexion, and a straight incision was made in the midline from the vertex to the C4 spinous process. A median suboccipital craniotomy was performed in order to expose the torcula and suboccipital dura. The suboccipital dura was reflected superiorly over the torcula and bilateral transverse sinuses. The occipital sinus was ligated, and the cerebellar hemispheres and vermis were retracted inferiorly in order to proceed through the supracerebellar infratentorial corridor. Two precentral cerebellar veins were divided to improve visualization of the deep anatomy.
At the tentorial incisura, the splenium of the corpus callosum and confluence of the venous structures at the vein of Galen were identified. The quadrigeminal cistern was opened to release CSF and promote brain relaxation. The arachnoid adhesions tethering the cerebellar vermis to the deep venous complex were released, and dissection was continued under the left basal vein of Rosenthal, lateral to the divided precentral cerebellar vein. The tectum, perforator arteries, and a large developmental venous anomaly were noted, and hemosiderin staining of the pial surface of the supracollicular area was visualized. The supracollicular area was opened at the site of hemosiderin staining in order to enter the CCM. The lesion was resected with standard microsurgical technique, in a piecemeal fashion. The CCM was initially dissected inferiorly and its capsule was retracted cephalad, away from the superior colliculus. Next, the lesion was retracted medially, so that the lateral border of the capsule could be dissected away from the pulvinar. At the conclusion of the resection, the third ventricle was visualized.
The patient had a complicated postoperative course, including a cerebellar hemorrhage treated with EVD placement and suboccipital craniectomy with expansion duraplasty, respiratory failure requiring tracheostomy, and persistent dysphagia requiring percutaneous endoscopic gastrostomy (PEG) tube placement. The patient was discharged to an inpatient rehabilitation facility (mRS score 3 at discharge) two weeks after CCM resection. Over the course of the next 18 months, the patient subsequently underwent CSF diversion with ventriculoperitoneal shunt placement for hydrocephalus, pseudomeningocele repair, multiple shunt revisions, and suboccipital titanium mesh cranioplasty with lysis of adhesions. In total, the patient underwent nine additional surgical procedures after the initial resection. Follow-up MRI, performed 19 months after surgery, showed residual CCM. At 20 months clinical follow-up, the patient was able to walk independently, but continued to experience persistent headaches and diplopia, for a mRS score of 3.
Three patients with dorsolateral midbrain or pontine CCMs underwent resection via a retrosigmoid approach ipsilateral to the lesion (38%). For all patients, a lumbar drain was placed preoperatively and removed at the end of surgery. The patient was placed in a three-quarter prone position, with the head rotated to the side ipsilateral to the lesion and in capital flexion. A sigmoid incision was made from 3 cm posterior to the superior border of the pinna, across the asterion to the nuchal midline. A retrosigmoid craniectomy and partial posterior mastoidectomy were performed to expose the inferior border of the transverse sinus and posterior border of the sigmoid sinus, and 50 mL of CSF was released from the lumbar drain prior to dural opening to promote brain relaxation.
The dura was opened in a cruciate fashion, and the arachnoid of the cisterna magna was opened to release additional CSF (i.e., Dandy's maneuver). The lateral aspect of the cerebellar hemisphere was retracted medially to expose the facial and vestibulocochlear nerves. The junction of the tentorium with its attachment to the petrous bone was followed medially until the trigeminal nerve was encountered. The superior petrosal vein was coagulated and divided, and the arachnoid of the ambient and quadrigeminal cisterns was opened to allow further CSF egress. The details of each CCM resection varied among patients and are described below.
A 70 year-old female presented with six months of progressively worsening right-sided hemiparesis (mRS score 3 at presentation). MRI showed a 2.1 cm CCM in the left midbrain tegmentum (Fig. 3). From a left retrosigmoid approach, the CCM could not be readily visualized at the pial surface. The trochlear nerve was identified, and the tentorium was divided in order to explore cephalad and medially. The lateral pontomesencephalic sulcus was opened longitudinally, and the CCM was immediately encountered below the pial surface. The lesion was resected with standard microsurgical technique, in a piecemeal fashion. During the resection, the right-sided hemibody SSEPs were lost without changes in MEPs. No residual CCM was evident on MRI performed on POD 1. Postoperatively, the patient developed contralateral, right frontal subdural and intracerebral hematomas, which were managed conservatively. She was discharged from the hospital to an inpatient rehabilitation facility (mRS score 3 at discharge) on POD 6. At 2 months clinical follow-up, the patient had improved to a mRS score of 2.
A 44 year-old female presented with one month of progressively worsening left-sided hemibody sensory loss, headache, diplopia, and ataxia (mRS score 3 at presentation). MRI showed a 1.1 cm CCM in the right pons, immediately caudal to the pontomesencephalic junction (Fig. 4). From a right retrosigmoid approach, the superior cerebellar artery (SCA) was noted to be coursing over the approximate location of the lesion and was therefore circumferentially dissected from its arachnoid attachments to allow for mobilization. Since the CCM was subpial, a longitudinal incision was made in the lateral pontomesencephalic sulcus to access the lesion. Dissecting above and below the SCA, the CCM was resected in a piecemeal fashion with standard microsurgical technique. Toward the end of the resection, the left-sided hemibody SSEPs were lost, while the MEPs remained stable. The patient had an uncomplicated postoperative course and was discharged from the hospital to an inpatient rehabilitation facility (mRS score 3 at discharge) on POD 4. At 21 months radiologic and clinical follow-up, no residual CCM was evident on MRI, and the patient had improved to a mRS score of 1 and was able to return to work.
A 42 year-old female presented with three months of progressively worsening headaches, diplopia, and left-sided dysmetria (mRS score 3 at presentation). MRI showed a 1.4 cm CCM in the right midbrain and pons, at the pontomesencephalic junction (Fig. 5). From a right retrosigmoid approach, the CCM, which did not broach the pial surface, could not be readily visualized. After identifying the relevant local anatomy, a myelotomy was made in the infracollicular area, medial to the origin of the trochlear nerve. The CCM was encountered approximately 0.5 mm deep to the pial surface, and resected in a piecemeal fashion with standard microsurgical technique. During wound closure, the left-sided SSEPs and MEPs were lost. The patient had an uncomplicated postoperative course and was discharged from the hospital to an inpatient rehabilitation facility (mRS score 3 at discharge) on POD 5. At 8 and 12 months radiologic and clinical follow-up, respectively, no residual CCM was evident on MRI, and the patient had improved to a mRS score of 2.
Three patients with dorsomedian pontine or medullary CCMs underwent resection via a suboccipital trans-cerebellomedullary fissure approach (38%). The patient was placed in a prone position with capital flexion. A longitudinal midline incision was made from the inion to the C4 spinous process, and a suboccipital craniotomy or craniectomy and C1 laminectomy were performed. The dura was opened in a Y-shaped fashion, and the arachnoid of the cisterna magna was opened to release CSF and expose the cerebellar tonsils.
The cerebellomedullary fissures were opened bilaterally to access the dorsal surface of the medulla and floor of the fourth ventricle. The cerebellar tonsils were retracted superolaterally, and the vermis was retracted superiorly to maintain the operative view. Depending on the craniocaudal location of the CCM, the tela choroidea of the fourth ventricle was opened bilaterally to increase the surgical corridor superiorly, up to the cerebral aqueduct. The details of each CCM resection varied among patients and are described below.
A 28 year-old male presented with one month of progressively worsening bilateral upper extremity sensory loss and ataxia (mRS score 3 at presentation). MRI showed a 1.5 cm CCM in the dorsomedian medulla (Fig. 6). From a suboccipital trans-cerebellomedullary fissure approach, the lesion could be visualized at the pial surface of the dorsal medulla. The posterior median sulcus overlying the CCM was opened, and the lesion was resected in a piecemeal fashion with standard microsurgical technique. During dural closure, the SSEPs of the bilateral upper extremities were lost, followed by the loss of bilateral lower extremity SSEPs. The dura was re-opened in order to explore the surgical cavity, but no hematoma or other anomaly was identified to explain the loss of electrophysiologic signals. The patient had an uncomplicated postoperative course and was discharged from the hospital to an inpatient rehabilitation facility (mRS score 3 at discharge) on POD 6. At 23 and 21 months radiologic and clinical follow-up, respectively, no residual CCM was evident on MRI, and the patient had improved to a mRS score of 2.
A 40 year-old male presented with six months of progressively worsening left-sided hemifacial and right-sided hemibody sensory alteration (mRS score 3 at presentation). MRI showed a 1.6 cm CCM in the right dorsomedian medulla (Fig. 7). From a suboccipital trans-cerebellomedullary fissure approach, the lesion was readily visualized at the medulla's caudal pial surface. A vertical myelotomy was performed along the posterior median sulcus, which was overlying the lesion, and the CCM resection was initiated by internal debulking. A circumferential dissection was then performed around the collapsed CCM capsule with standard microsurgical technique, and the remainder of the lesion was removed in a piecemeal fashion. No residual CCM was evident on MRI performed on POD 1. Postoperatively, the patient suffered from persistent dysphagia, requiring PEG tube placement on POD 6. He was discharged to home two weeks after surgery, at which time he had improved to a mRS score of 2. Unfortunately, the patient was subsequently lost to follow-up.
A 28 year-old female presented with one week of progressively worsening right-sided headache and hearing loss, diplopia, bilateral upper extremity sensory loss, dysarthria, and dysphagia (mRS score 4 at presentation). MRI showed a 2.8 cm CCM in the left pons (Fig. 8). From a suboccipital trans-cerebellomedullary fissure approach, the anatomical landmarks at the floor of the fourth ventricle were identified and confirmed with electrophysiologic stimulation and BSEPs. A longitudinal myelotomy was performed in the infrafacial triangle, bounded by the posterior median sulcus medially, facial colliculus superiorly and laterally, and stria medullaris inferiorly. The opening was approximately 5 mm lateral to the posterior median sulcus and measured approximately 8 mm in length. The CCM was noted beneath the pial surface, and subacute blood products extravasated under pressure after the capsule was opened. The remainder of the CCM was resected with standard microsurgical technique in a piecemeal fashion. At the end of the resection, the BSEPs for the glossopharyngeal and vagus nerves and the left-sided hemibody SSEPs were lost. No residual CCM was evident on MRI performed on POD 1. Postoperatively, the patient suffered from persistent dysphagia and pharyngeal edema, requiring PEG tube placement and tracheostomy, respectively, on POD 4. She was transferred to a transitional care hospital two weeks after surgery in neurological stable condition. At 2 months clinical follow-up, the patient is improved from her preoperative functional status and able to walk with assistance, although she remains with a mRS score of 4.
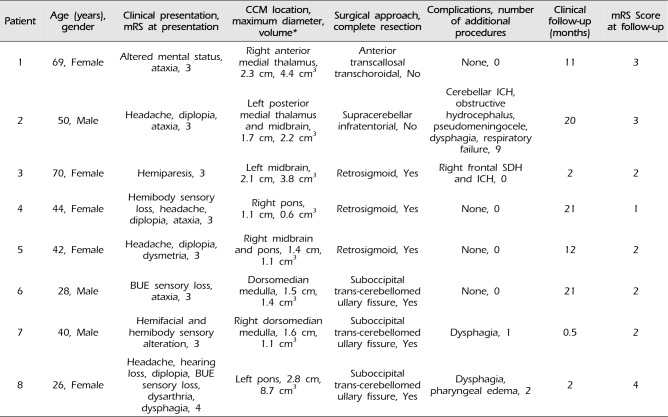
Table 1 summarizes the baseline characteristics and postoperative outcomes of the study cohort. Complete resection was achieved in six patients (75%), including all patients with brainstem CCMs (100%). Perioperative complications were present in four patients (50%), including three patients who required additional procedures (38%). At a median follow-up of 11.5 months (range 0.5 to 21 months), the median mRS score was 2 (range 1 to 4). Functional outcome was improved, at follow-up, in five patients (63%), stable in three (38%), and worse in none. Five patients were functionally independent, defined as mRS 2 or less (63%).
The management of thalamic and brainstem CCMs remains controversial. The elevated risk of both initial and repeat hemorrhage for these deep-seated CCMs compared to cortical CCMs favors intervention, whereas the relatively high rate of neurological morbidity associated with surgical resection of these lesions supports a more conservative approach.41)42) Although radiosurgery is a conceptually attractive alternative to surgical resection of eloquent CCMs, the radiosurgery-induced complication rate is significantly higher for CCMs than for AVMs, and CCMs cannot be radiologically monitored for obliteration after radiosurgery.3)5)6)8)9)10)12)13)14)15)16)17)18)19)20)21)22)23)25)26)27)28)29)30)31)32)33)34)35)36)37)43)44)49)50)52)53)56)59)63)64)65)66)67)68) Instead, the proposed effect of radiosurgery on CCMs is a decreased risk of symptomatic hemorrhages, which is controversial due to temporal clustering of CCM hemorrhages.4) Thus, surgical resection remains the gold standard of CCM intervention and is warranted for appropriately selected patients harboring thalamic and brainstem CCMs.
The following patient and lesion characteristics should be considered when deciding on the surgical approach for deep-seated CCMs. First, the patient's neurological and clinical status at presentation should dictate the decision for intervention versus conservative management. Patients with symptomatic CCM hemorrhage, including progressive neurological deterioration from multiple hemorrhages, are preferred candidates for intervention. In patients with focal neurological deficits from CCM hemorrhage, an approach through a region related to the pre-existing deficit should be utilized in favor of one which may incur additional injury. We typically waited one to two weeks after a clinically symptomatic hemorrhage to perform surgical intervention, in order to allow liquefaction of the hematoma but with the goal of intervening before contraction and gliotic scarring of the hematoma. Additionally, medical comorbidities should be limited and clinical optimized to ensure the patient will be able to tolerate the physiologic stress of general anesthesia and major intracranial surgery. Next, the location of CCM presentation to the pial surface, or the closest pial border for subpial lesions, will determine the site of entry and, consequently, the surgical approach. Finally, the size and morphology of the CCM should be carefully assessed at the time of intervention, as these lesions have been shown to be dynamic, rather than static.7) Furthermore, a new hemorrhage may yield a previously treacherous surgical route, and even small morphological alterations of brainstem CCMs can force revisions of the original surgical plan.
Numerous approaches have been proposed for to gain access to thalamic and brainstem CCMs.1)39)40)47)55)62) When feasible, we advocate for the use of existing subarachnoid corridors to deep-seated lesions, such as the quadrigeminal cistern through a supracerebellar infratentorial approach (Patient 2) and the cerebellopontine cistern through a retrosigmoid approach (Patients 3-5).11) The retrosigmoid approach is the workhorse of skull base surgery in the posterior fossa and, in combination with adequate brain relaxation, allows a fairly generous operative corridor for CCMs in the ventrolateral or dorsolateral pons.54) Although we generally avoid the sitting position due to the increased risk of venous air embolism and surgeon preference, it has certain advantages over prone and supine positions which may be considered by those who have gained sufficient experience and comfort with this position.46) Sharp dissection and opening of the tela choroidea, such as the choroidal fissure through an anterior transcallosal transchoroidal approach (Patient 1) or the cerebellomedullary fissure through a suboccipital approach to the fourth ventricle (Patients 6-8), can minimize violation of normal brain parenchyma.45) The trans-cerebellomedullary fissure approach allows a broad exposure of the floor of the fourth ventricle without compromising the vermis, which can lead to cerebellar mutism and truncal ataxia.48) Some cerebrovascular surgeons caution against accessing brainstem CCMs through the floor of the fourth ventricle due to the high density of critical structures, especially in the midline. However, we have found that the use of previously defined safe entry zones on the posterior surface of the brainstem and floor of the fourth ventricle can be utilized for dorsally located brainstem CCMs with limited neurological morbidity.40)
Regardless of the approach, routine use of intraoperative neuronavigation and electrophysiologic monitoring is crucial to supplementing intraoperative identification of landmarks for determining the safest site of entry, due to the distortion of normal anatomy by CCMs. This is especially true for lesions which do not present to the pial surface or stain it with hemosiderin. By utilizing commonly employed surgical approaches, we were able to improve or maintain the functional status of all patients in our study cohort. Although 38% of patients required additional procedures after CCM resection, five patients were functionally independent (63%) at clinical follow-up (median duration 11.5 months). The majority of perioperative complications for thalamic and brainstem CCMs have been shown to abate over time, but the combined rate of long-term surgical morbidity and mortality remains significant, exceeding 10% in most large series.41)42)58) Samii et al. reported new cranial nerve, motor, and sensory deficits in 47%, 8%, and 33% of patients after surgical resection of brainstem CCMs, respectively.61) Thus, despite every effort to optimize patient outcomes, safe and successful surgery of thalamic and brainstem CCMs remains one of the most formidable challenges facing modern neurosurgeons.
The limitations of our study should be noted. The study design is retrospective and describes the experience of a single surgeon (K.C.L.) at a single center, which subjects our findings to the selection and referral biases of the physician and institution. Since the surgeon was not present at our institution prior to 2010, the cohort size is relatively small, which restricts our ability to perform any meaningful statistical analysis. The number of cases was also too small to adequately assess the safety and efficacy of the surgical techniques and approaches employed in this study. Additionally, certain surgical corridors, such as transpetrosal approaches which may be preferred for more cranially or ventrally located midbrain CCMs, which were not utilized for our patient cohort.60) However, we believe that highlighting the technical aspects of the common approaches employed in our study may provide valuable insights regarding the modern management of patients harboring CCMs of the thalamus and brainstem. Furthermore, prospective studies remain necessary to determine the long-term benefit of intervention for CCM patients and the patient and lesion characteristics most likely to benefit from surgical resection.51)
The thalamus and brainstem are highly eloquent brain regions which exhibit poor tolerance to CCM hemorrhage. Partial CCM resection may offer temporary neurological benefit by decompressing the local mass effect of a hematoma, but since residual CCM remains prone to hemorrhage, the goal of surgery is complete extirpation. Selection of the optimal surgical approach is important for maximizing the operative field, which is typically quite small for deep-seated lesions, thus limiting manipulation of the lesion and reducing the likelihood of total resection. Appreciation of the technical nuances of the surgical approaches for thalamic and brainstem CCM resection, identification of the anatomical landmarks of safe entry zones, and use of stereotactic image-guided neuronavigation may reduce operative morbidity and mortality and improve long-term patient outcomes.
References
1. Abla AA, Turner JD, Mitha AP, Lekovic G, Spetzler RF. Surgical approaches to brainstem cavernous malformations. Neurosurg Focus. 2010; 9. 29(3):E8.

2. Aiba T, Tanaka R, Koike T, Kameyama S, Takeda N, Komata T. Natural history of intracranial cavernous malformations. J Neurosurg. 1995; 7. 83(1):56–59. PMID: 7782850.

3. Awad AJ, Walcott BP, Stapleton CJ, Ding D, Lee CC, Loeffler JS. Repeat radiosurgery for cerebral arteriovenous malformations. J Clin Neurosci. 2015; 6. 22(6):945–950. PMID: 25913746.

4. Barker FG 2nd, Amin-Hanjani S, Butler WE, Lyons S, Ojemann RG, Chapman PH, et al. Temporal clustering of hemorrhages from untreated cavernous malformations of the central nervous system. Neurosurgery. 2001; 7. 49(1):15–24. discussion 24-5. PMID: 11440436.

5. Buell TJ, Ding D, Starke RM, Webster Crowley R, Liu KC. Embolization-induced angiogenesis in cerebral arteriovenous malformations. J Clin Neurosci. 2014; 11. 21(11):1866–1871. PMID: 25001989.

6. Chen CJ, Chivukula S, Ding D, Starke RM, Lee CC, Yen CP, et al. Seizure outcomes following radiosurgery for cerebral arteriovenous malformations. Neurosurg Focus. 2014; 9. 37(3):E17.

7. Clatterbuck RE, Moriarity JL, Elmaci I, Lee RR, Breiter SN, Rigamonti D. Dynamic nature of cavernous malformations: a prospective magnetic resonance imaging study with volumetric analysis. J Neurosurg. 2000; 12. 93(6):981–986. PMID: 11117871.

8. Cohen-Inbar O, Ding D, Chen CJ, Sheehan JP. Stereotactic radiosurgery for deep intracranial arteriovenous malformations, part 1: brainstem arteriovenous malformations. J Clin Neurosci. 2016; 2. 24:30–36. PMID: 26740034.

9. Cohen-Inbar O, Ding D, Sheehan JP. Stereotactic radiosurgery for deep intracranial arteriovenous malformations, part 2 basal ganglia and thalamus arteriovenous malformations. J Clin Neurosci. 2016; 2. 24:37–42. PMID: 26732284.

10. Conger JR, Ding D, Raper DM, Starke RM, Durst CR, Liu KC, et al. Preoperative embolization of cerebral arteriovenous malformations with silk suture and particles: technical considerations and outcomes. J Cerebrovasc Endovasc Neurosurg. 2016; 6. 18(2):90–99. PMID: 27790398.

11. de Oliveira JG, Lekovic GP, Safavi-Abbasi S, Reis CV, Hanel RA, Porter RW, et al. Supracerebellar infratentorial approach to cavernous malformations of the brainstem: surgical variants and clinical experience with 45 patients. Neurosurgery. 2010; 2. 66(2):389–399. PMID: 20042987.
12. Ding D. Mechanisms of cyst formation after radiosurgery for intracranial arteriovenous malformations. Clin Neurol Neurosurg. 2014; 9. 124:192–193. PMID: 25070227.

13. Ding D. Pathogenesis of radiosurgery-induced cyst formation in patients with cerebral arteriovenous malformations. Acta Neurochir (Wien). 2015; 5. 157(5):775–777. PMID: 25749841.

14. Ding D, Liu KC. Predictive capability of the Spetzler-Martin versus supplementary grading scale for microsurgical outcomes of cerebellar arteriovenous malformations. J Cerebrovasc Endovasc Neurosurg. 2013; 12. 15(4):307–310. PMID: 24729957.

15. Ding D, Quigg M, Starke RM, Xu Z, Yen CP, Przybylowski CJ, et al. Radiosurgery for temporal lobe arteriovenous malformations: effect of temporal location on seizure outcomes. J Neurosurg. 2015; 10. 123(4):924–934. PMID: 25884262.

16. Ding D, Quigg M, Starke RM, Yen CP, Przybylowski CJ, Dodson BK, et al. Cerebral arteriovenous malformations and epilepsy, part 2: predictors of seizure outcomes following radiosurgery. World Neurosurg. 2015; 9. 84(3):653–662. PMID: 26026628.

17. Ding D, Sheehan JP, Starke RM, Durst CR, Raper DM, Conger JR, et al. Embolization of cerebral arteriovenous malformations with silk suture particles prior to stereotactic radiosurgery. J Clin Neurosci. 2015; 10. 22(10):1643–1649. PMID: 26186966.

18. Ding D, Starke RM, Kano H, Lee JY, Mathieu D, Pierce J, et al. Stereotactic radiosurgery for Spetzler-Martin Grade III arteriovenous malformations: an international multicenter study. J Neurosurg. 2017; 3. 126(3):859–871. PMID: 27081906.

19. Ding D, Starke RM, Kano H, Mathieu D, Huang P, Kondziolka D, et al. Radiosurgery for cerebral arteriovenous malformations in a randomized trial of unruptured brain arteriovenous malformations (ARUBA)-eligible patients: a multicenter study. Stroke. 2016; 2. 47(2):342–349. PMID: 26658441.
20. Ding D, Starke RM, Kano H, Mathieu D, Huang PP, Feliciano C, et al. International multicenter cohort study of pediatric brain arteriovenous malformations. Part 1: predictors of hemorrhagic presentation. J Neurosurg Pediatr. 2017; 2. 19(2):127–135. PMID: 27911248.

21. Ding D, Starke RM, Kano H, Mathieu D, Huang PP, Kondziolka D, et al. Stereotactic radiosurgery for a randomized trial of unruptured brain arteriovenous malformations (ARUBA)-Eligible Spetzler-Martin Grade I and II arteriovenous malformations: a multicenter study. World Neurosurg. 2017; 3. 23. [Epub ahead of print].
22. Ding D, Starke RM, Liu KC, Crowley RW. Cortical plasticity in patients with cerebral arteriovenous malformations. J Clin Neurosci. 2015; 12. 22(12):1857–1861. PMID: 26256067.

23. Ding D, Starke RM, Quigg M, Yen CP, Przybylowski CJ, Dodson BK, et al. Cerebral arteriovenous malformations and epilepsy, part 1: predictors of seizure presentation. World Neurosurg. 2015; 9. 84(3):645–652. PMID: 25753234.

24. Ding D, Starke RM, Crowley RW, Liu KC. Endoport-assisted microsurgical resection of cerebral cavernous malformations. J Clin Neurosci. 2015; 6. 22(6):1025–1029. PMID: 25769248.

25. Ding D, Starke RM, Yen CP, Sheehan JP. Radiosurgery for cerebellar arteriovenous malformations: does infratentorial location affect outcome? World Neurosurg. 2014; Jul-Aug. 82(1-2):e209–e217. PMID: 24530455.

26. Ding D, Xu Z, Shih HH, Starke RM, Yen CP, Cohen-Inbar O, et al. Worse outcomes after repeat vs initial stereotactic radiosurgery for cerebral arteriovenous malformations: a retrospective matched-cohort study. Neurosurgery. 2016; 11. 79(5):690–700. PMID: 27759676.
27. Ding D, Xu Z, Shih HH, Starke RM, Yen CP, Sheehan JP. Stereotactic radiosurgery for partially resected cerebral arteriovenous malformations. World Neurosurg. 2016; 1. 85:263–272. PMID: 26459698.

28. Ding D, Xu Z, Starke RM, Yen CP, Shih HH, Buell TJ, et al. Radiosurgery for cerebral arteriovenous malformations with associated arterial aneurysms. World Neurosurg. 2016; 3. 87:77–90. PMID: 26732956.

29. Ding D, Xu Z, Yen CP, Starke RM, Sheehan JP. Radiosurgery for cerebral arteriovenous malformations in elderly patients: effect of advanced age on outcomes after intervention. World Neurosurg. 2015; 9. 84(3):795–804. PMID: 25997797.

30. Ding D, Xu Z, Yen CP, Starke RM, Sheehan JP. Radiosurgery for unruptured cerebral arteriovenous malformations in pediatric patients. Acta Neurochir (Wien). 2015; 2. 157(2):281–291. PMID: 25514868.

31. Ding D, Yen CP, Starke RM, Xu Z, Sheehan JP. Effect of prior hemorrhage on intracranial arteriovenous malformation radiosurgery outcomes. Cerebrovasc Dis. 2015; 39(1):53–62. PMID: 25547253.

32. Ding D, Yen CP, Starke RM, Xu Z, Sheehan JP. Radiosurgery for ruptured intracranial arteriovenous malformations. J Neurosurg. 2014; 8. 121(2):470–481. PMID: 24655098.

33. Ding D, Yen CP, Starke RM, Xu Z, Sun X, Sheehan JP. Outcomes following single-session radiosurgery for high-grade intracranial arteriovenous malformations. Br J Neurosurg. 2014; 10. 28(5):666–674. PMID: 24372542.

34. Ding D, Yen CP, Starke RM, Xu Z, Sun X, Sheehan JP. Radiosurgery for Spetzler-Martin Grade III arteriovenous malformations. J Neurosurg. 2014; 4. 120(4):959–969. PMID: 24460487.

35. Ding D, Yen CP, Xu Z, Starke RM, Sheehan JP. Radiosurgery for low-grade intracranial arteriovenous malformations. J Neurosurg. 2014; 8. 121(2):457–467. PMID: 24605839.

36. Ding D, Yen CP, Xu Z, Starke RM, Sheehan JP. Radiosurgery for patients with unruptured intracranial arteriovenous malformations. J Neurosurg. 2013; 5. 118(5):958–966. PMID: 23530863.

37. Ding D, Yen CP, Xu Z, Starke RM, Sheehan JP. Radiosurgery for primary motor and sensory cortex arteriovenous malformations: outcomes and the effect of eloquent location. Neurosurgery. 2013; 11. 73(5):816–824. PMID: 23867301.
38. Garcia RM, Ivan ME, Lawton MT. Brainstem cavernous malformations: surgical results in 104 patients and a proposed grading system to predict neurological outcomes. Neurosurgery. 2015; 3. 76(3):265–277. discussion 277-8. PMID: 25599205.
39. Garrett M, Spetzler RF. Surgical treatment of brainstem cavernous malformations. Surg Neurol. 2009; 12. 72(Suppl 2):S3–S9. discussion S9-10. PMID: 19665186.

40. Giliberto G, Lanzino DJ, Diehn FE, Factor D, Flemming KD, Lanzino G. Brainstem cavernous malformations: anatomical, clinical, and surgical considerations. Neurosurg Focus. 2010; 9. 29(3):E9.

41. Gross BA, Batjer HH, Awad IA, Bendok BR. Brainstem cavernous malformations. Neurosurgery. 2009; 5. 64(5):E805–E818. discussion E818. PMID: 19404127.

42. Gross BA, Batjer HH, Awad IA, Bendok BR. Cavernous malformations of the basal ganglia and thalamus. Neurosurgery. 2009; 7. 65(1):7–18. discussion 18-9. PMID: 19574821.

43. Hong CS, Peterson EC, Ding D, Sur S, Hasan D, Dumont AS, et al. Intervention for a randomized trial of unruptured brain arteriovenous malformations (ARUBA) - Eligible patients: an evidence-based review. Clin Neurol Neurosurg. 2016; 11. 150:133–138. PMID: 27656780.

44. Ilyas A, Chen CJ, Ding D, Taylor DG, Moosa S, Lee CC, et al. Volume-staged versus dose-staged stereotactic radiosurgery outcomes for large brain arteriovenous malformations: a systematic review. J Neurosurg. 2017; 1. 1–11. [Epub ahead of print].

45. Kawashima M, Matsushima T, Nakahara Y, Takase Y, Masuoka J, Ohata K. Trans-cerebellomedullary fissure approach with special reference to lateral route. Neurosurg Rev. 2009; 10. 32(4):457–464. PMID: 19609581.

46. Leslie K, Hui R, Kaye AH. Venous air embolism and the sitting position: a case series. J Clin Neurosci. 2006; 5. 13(4):419–422. PMID: 16678719.

47. Li D, Zhang J, Hao S, Tang J, Xiao X, Wu Z, et al. Surgical treatment and long-term outcomes of thalamic cavernous malformations. World Neurosurg. 2013; May-Jun. 79(5-6):704–713. PMID: 22381871.

48. Matsushima T, Abe H, Kawashima M, Inoue T. Exposure of the wide interior of the fourth ventricle without splitting the vermis: importance of cutting procedures for the tela choroidea. Neurosurg Rev. 2012; 10. 35(4):563–571. discussion 571-2. PMID: 22527626.

49. Moosa S, Chen CJ, Ding D, Lee CC, Chivukula S, Starke RM, et al. Volume-staged versus dose-staged radiosurgery outcomes for large intracranial arteriovenous malformations. Neurosurg Focus. 2014; 9. 37(3):E18.

50. Mouchtouris N, Jabbour PM, Starke RM, Hasan DM, Zanaty M, Theofanis T, et al. Biology of cerebral arteriovenous malformations with a focus on inflammation. J Cereb Blood Flow Metab. 2015; 2. 35(2):167–175. PMID: 25407267.

51. Moultrie F, Horne MA, Josephson CB, Hall JM, Counsell CE, Bhattacharya JJ, et al. Outcome after surgical or conservative management of cerebral cavernous malformations. Neurology. 2014; 8. 83(7):582–589. PMID: 24994841.

52. Oermann EK, Ding D, Yen CP, Starke RM, Bederson JB, Kondziolka D, et al. Effect of prior embolization on cerebral arteriovenous malformation radiosurgery outcomes: a case-control study. Neurosurgery. 2015; 9. 77(3):406–417. discussion 417. PMID: 25875580.
53. Oermann EK, Rubinsteyn A, Ding D, Mascitelli J, Starke RM, Bederson JB, et al. Using a machine learning approach to predict outcomes after radiosurgery for cerebral arteriovenous malformations. Sci Rep. 2016; 2. 09. 6:21161. PMID: 26856372.

54. Ohue S, Fukushima T, Friedman AH, Kumon Y, Ohnishi T. Retrosigmoid suprafloccular transhorizontal fissure approach for resection of brainstem cavernous malformation. Neurosurgery. 2010; 6. 66(6 Suppl Operative):306–312. discussion 312-3. PMID: 20489521.

55. Pandey P, Westbroek EM, Gooderham PA, Steinberg GK. Cavernous malformation of brainstem, thalamus, and basal ganglia: a series of 176 patients. Neurosurgery. 2013; 4. 72(4):573–589. discussion 588-9. PMID: 23262564.
56. Patibandla MR, Ding D, Xu Z, Sheehan JP. Stereotactic radiosurgery for pediatric high-grade brain arteriovenous malformations: our experience and review of literature. World Neurosurg. 2017; 3. 23. [Epub ahead of print].

57. Porter PJ, Willinsky RA, Harper W, Wallace MC. Cerebral cavernous malformations: natural history and prognosis after clinical deterioration with or without hemorrhage. J Neurosurg. 1997; 8. 87(2):190–197. PMID: 9254081.

58. Porter RW, Detwiler PW, Spetzler RF, Lawton MT, Baskin JJ, Derksen PT, et al. Cavernous malformations of the brainstem: experience with 100 patients. J Neurosurg. 1999; 1. 90(1):50–58. PMID: 10413155.

59. Przybylowski CJ, Ding D, Starke RM, Yen CP, Quigg M, Dodson B, et al. Seizure and anticonvulsant outcomes following stereotactic radiosurgery for intracranial arteriovenous malformations. J Neurosurg. 2015; 6. 122(6):1299–1305. PMID: 25614948.

60. Recalde RJ, Figueiredo EG, de Oliveira E. Microsurgical anatomy of the safe entry zones on the anterolateral brainstem related to surgical approaches to cavernous malformations. Neurosurgery. 2008; 3. 62(3 Suppl 1):9–15. discussion 15-7. PMID: 18424962.

61. Samii M, Eghbal R, Carvalho GA, Matthies C. Surgical management of brainstem cavernomas. J Neurosurg. 2001; 11. 95(5):825–832. PMID: 11702873.

62. Sinson G, Zager EL, Grossman RI, Gennarelli TA, Flamm ES. Cavernous malformations of the third ventricle. Neurosurgery. 1995; 7. 37(1):37–42. PMID: 8587688.

63. Starke RM, Ding D, Kano H, Mathieu D, Huang PP, Feliciano C, et al. International multicenter cohort study of pediatric brain arteriovenous malformations. Part 2: Outcomes after stereotactic radiosurgery. J Neurosurg Pediatr. 2017; 2. 19(2):136–148. PMID: 27911249.

64. Starke RM, Kano H, Ding D, Lee JY, Mathieu D, Whitesell J, et al. Stereotactic radiosurgery for cerebral arteriovenous malformations: evaluation of long-term outcomes in a multicenter cohort. J Neurosurg. 2017; 1. 126(1):36–44. PMID: 26943847.

65. Starke RM, Sheehan JP, Ding D, Liu KC, Kondziolka D, Crowley RW, et al. Conservative management or intervention for unruptured brain arteriovenous malformations. World Neurosurg. 2014; 11. 82(5):e668–e669. PMID: 25053376.

66. Starke RM, Yen CP, Chen CJ, Ding D, Mohila CA, Jensen ME, et al. An updated assessment of the risk of radiation-induced neoplasia after radiosurgery of arteriovenous malformations. World Neurosurg. 2014; Sep-Oct. 82(3-4):395–401. PMID: 23403354.

67. Starke RM, Yen CP, Ding D, Sheehan JP. A practical grading scale for predicting outcome after radiosurgery for arteriovenous malformations: analysis of 1012 treated patients. J Neurosurg. 2013; 10. 119(4):981–987. PMID: 23829820.

68. Yen CP, Ding D, Cheng CH, Starke RM, Shaffrey M, Sheehan J. Gamma Knife surgery for incidental cerebral arteriovenous malformations. J Neurosurg. 2014; 11. 121(5):1015–1021. PMID: 25148009.

Fig. 1
Preoperative MRI, T1-weighted sequence with contrast, (A) axial, (B) sagittal, and (C) coronal views, shows a 2.3 × 2.0 × 1.9 cm CCM in the right anterior medial thalamus, with medial extension into the third ventricle and inferior extension into the cerebral peduncle (circle). Postoperative MRI (follow-up interval 5 months) after resection via an anterior transcallosal transchoroidal approach, T1-weighted sequence without contrast, (D) axial, (E) sagittal, and (F) coronal views, shows dense hemosiderin staining along the right lateral aspect of the surgical cavity, which is suspicious for a small amount of residual CCM (circle). MRI = magnetic resonance imaging; CCM = cerebral cavernous malformation.
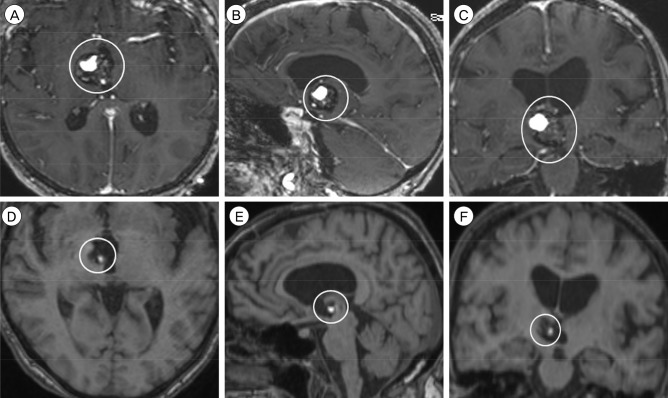
Fig. 2
Preoperative MRI, T1-weighted sequence with contrast, (A) axial, (B) sagittal, and (C) coronal views, shows a 1.7 × 1.5 × 1.7 cm CCM in left posterior medial thalamus and midbrain (circle). Postoperative MRI (follow-up interval 19 months) after resection via a supracerebellar infratentorial approach, T1-weighted sequence with contrast, (D) axial, (E) sagittal, and (F) coronal views, shows a 1.1 × 1.2 × 1.6 cm residual CCM (circle). MRI = magnetic resonance imaging; CCM = cerebral cavernous malformation.
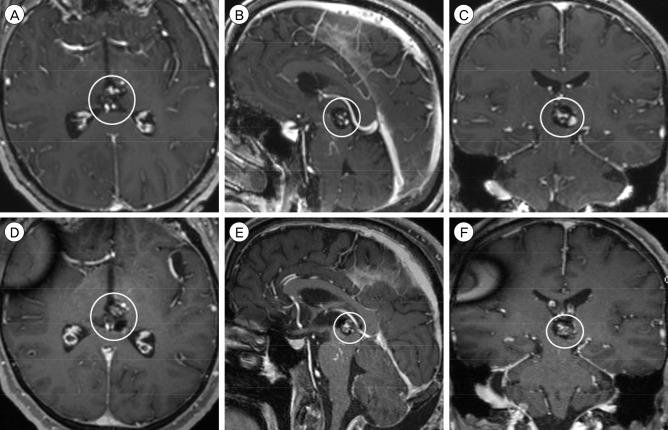
Fig. 3
Preoperative MRI, T1-weighted sequence with contrast, (A) axial, (B) sagittal, and (C) coronal views, shows a 2.1 × 1.9 × 1.9 cm CCM in the left midbrain, centered in the tegmentum (circle). Postoperative MRI (follow-up interval 1 day) after resection via a left-sided retrosigmoid approach, T1-weighted sequence with contrast, (D) axial, (E) sagittal, and (F) coronal views, shows post-surgical changes without evidence of residual CCM. MRI = magnetic resonance imaging; CCM = cerebral cavernous malformation.
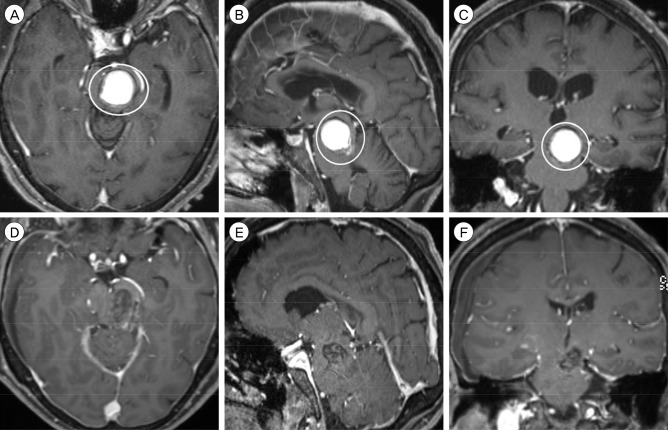
Fig. 4
Preoperative MRI, T1-weighted sequence with contrast, (A) axial, (B) sagittal, and (C) coronal views, shows a 1.0 × 1.0 × 1.1 cm CCM in the right pons, immediately inferior to the pontomesencephalic junction (circle). Postoperative MRI (follow-up interval 21 months) after resection via a right-sided retrosigmoid approach, T1-weighted sequence with contrast, (D) axial, (E) sagittal, and (F) coronal views, shows no evidence of residual CCM. MRI = magnetic resonance imaging; CCM = cerebral cavernous malformation.
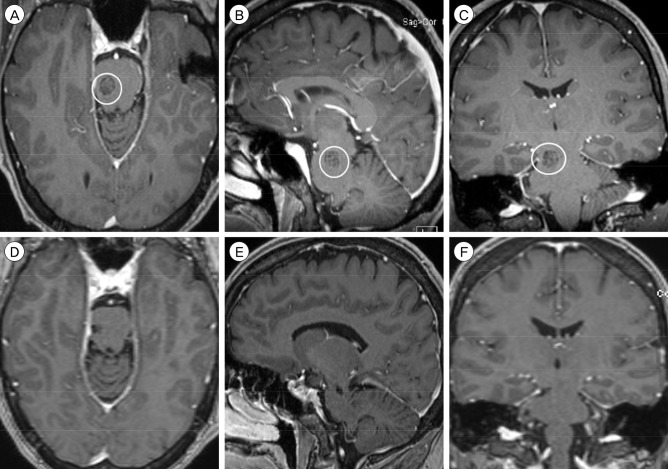
Fig. 5
Preoperative MRI, T1-weighted sequence with contrast, (A) axial, (B) sagittal, and (C) coronal views, shows a 1.4 × 1.2 × 1.3 cm CCM in the right midbrain and pons, centered at the pontomesencephalic junction (circle). Postoperative MRI (follow-up interval 8 months) after resection via a right-sided retrosigmoid approach, T1-weighted sequence with contrast, (D) axial, (E) sagittal, and (F) coronal views, shows no evidence of residual CCM. MRI = magnetic resonance imaging; CCM = cerebral cavernous malformation.
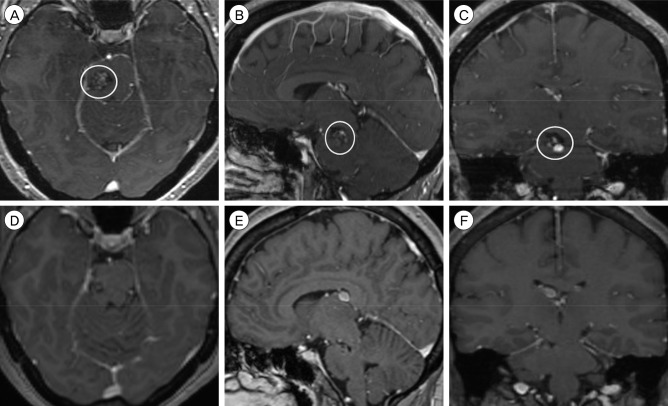
Fig. 6
Preoperative MRI, T1-weighted sequence with contrast, (A) axial, (B) sagittal, and (C) coronal views, shows a 1.5 × 1.4 × 1.3 cm CCM in the dorsomedian medulla (circle). Postoperative MRI (follow-up interval 23 months) after resection via a suboccipital trans-cerebellomedullary fissure approach, T1-weighted sequence with contrast, (D) axial, (E) sagittal, and (F) coronal views, shows no evidence of residual CCM. MRI = magnetic resonance imaging; CCM = cerebral cavernous malformation.
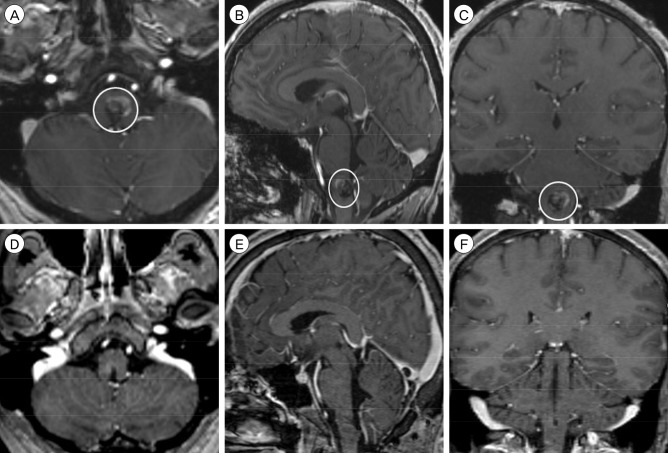
Fig. 7
Preoperative MRI, T1-weighted sequence with contrast, (A) axial, (B) sagittal, and (C) coronal views, shows a 1.6 × 1.2 × 1.1 cm CCM in the right dorsomedian medulla (circle). Postoperative MRI (follow-up interval 1 day) after resection via a suboccipital trans-cerebellomedullary fissure approach, T1-weighted sequence with contrast, (D) axial, (E) sagittal, and (F) coronal views, shows post-surgical changes without evidence of residual CCM. MRI = magnetic resonance imaging; CCM = cerebral cavernous malformation.
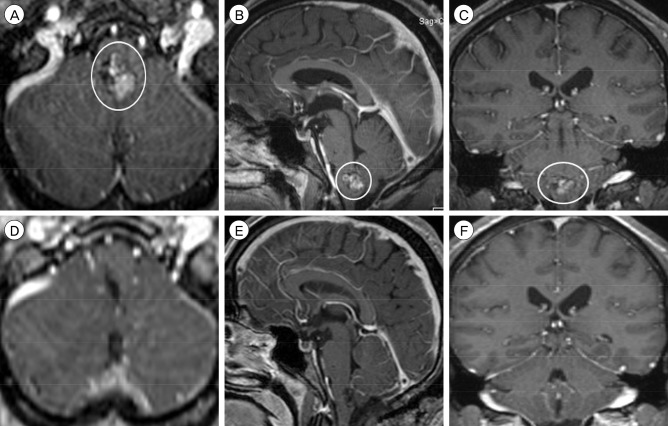
Fig. 8
Preoperative MRI, T1-weighted sequence with contrast, (A) axial, (B) sagittal, and (C) coronal views, shows a 2.8 × 2.7 × 2.3 cm CCM in the left pons. Postoperative MRI (follow-up interval 1 day) after resection via a suboccipital trans-cerebellomedullary fissure approach, T1-weighted sequence with contrast, (D) axial, (E) sagittal, and (F) coronal views, shows post-surgical changes without evidence of residual CCM. MRI = magnetic resonance imaging; CCM = cerebral cavernous malformation.
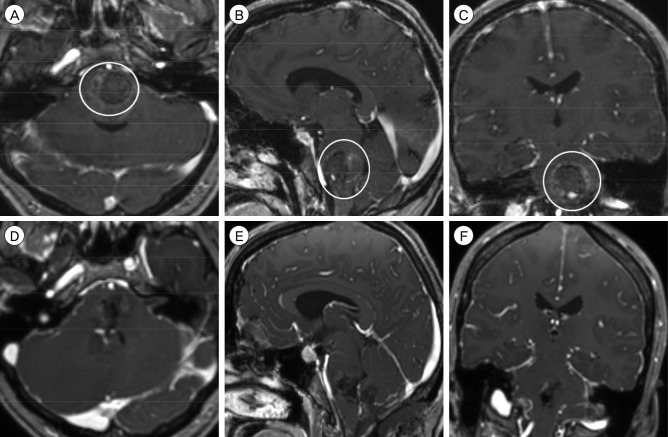
Table 1
Summary surgical approaches and postoperative outcomes for patients with thalamic and brainstem CCMs




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download