INTRODUCTION
The dorsal wall aneurysms can be defined as the aneurysms arising at nonbranching sites on dorsal wall of the supraclinoid internal carotid artery (ICA). Sometimes it found on the anteromedial wall of the supraclinoid segment of ICA.
12) In morphological aspect, the dorsal wall aneurysm can be divided into blood blister-like aneurysm (BBA) and saccular type aneurysm.
4)13) Because of its small-sized, broad-base thin neck, fragility, tendency to intraoperative bleeding,
4)6)9)12)13)18) sometimes that makes it difficult for neurosurgeons.
In 1969, Sundt and Murphy described the first case of BBA
14) in neurovascular history. This kind of dorsal wall aneurysm have been challenged by many neurosurgeons with various modalities (conventional clip, clip with wrapping, using Sundt [encircling] clip, trapping, and stent assisted coil, etc).
2)5)7)9)10)11)16)17)18) Although the advancement in microneurosurgery and endovascular techniques have been archived, the optimal treatment of BBA remained controversy. The dorsal wall aneurysm comprise 0.9–6.5% of all ICA aneurysm,
12) furthermore BBA comprise much smaller percentage of all ICA aneurysm. But because the treatment of choice (TOC) has not been established. It is challenging until now.
We analyzed retrospectively 17 cases of ruptured-BBA for 14 years. And, its surgical and clinical outcomes correlated with the surgical options among these various surgical modalities.
RESULTS
Patient characteristics
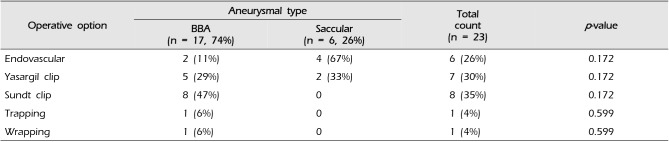
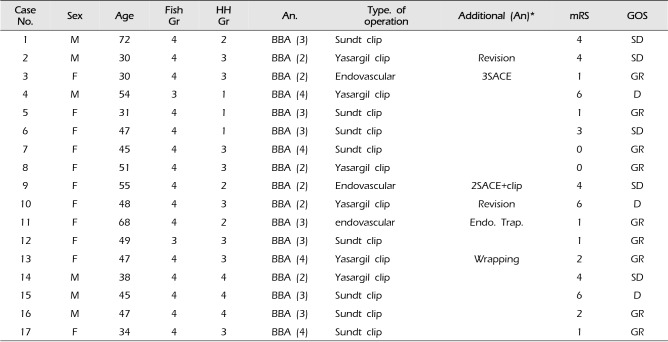
During 14 years, 23 cases of the ruptured-dorsal wall aneurysms were treated by 3 surgeons. Among 23 cases, 17 cases were patients of BBA. In BBA cases, the female predominance was observed (M:F = 6:11) and a mean age was 46.5 years old (range, 30–72 years old). In Hunt-Hess grading system, there were 3 (17.6%) patients in grade 1, 3 (17.6%) patients in grade 2, 8 (47.1%) patients in grade 3, and 3 (17.6%) patients in grade 4. In Fisher grading system, there were except 2 (11.8%) patients of grade 3, 15 (88.2%) BBA-patients were grade 4 in brain CT. Furthermore, there were 2 patients, underwent rebleeding (case 2, 15), and 3 patients taken aspirin, other anti-platelet agent or both (case 1, 9, 14). And 2 patients get delayed operation (case 2, 17) due to configuration change in follow up TFCA. (
Table 2,
3)
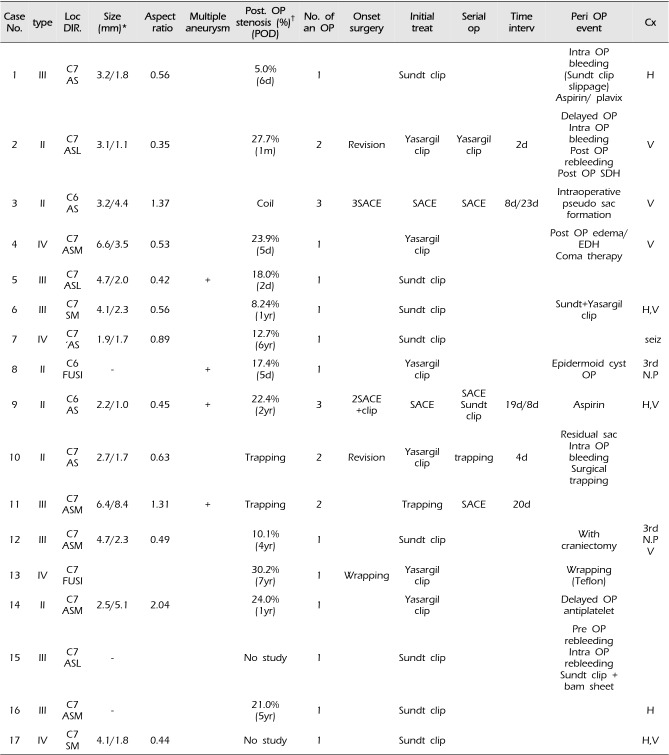
Aneurismal morphologic characteristics
16 patients were performed preoperative TFCA, and only 1 case didn't have preoperative TFCA due to pre-operative rebleeding. Along the Bojanowski's classification, we were able to classify our BBA cases into 4 subtypes. 6 cases (35.3%) were type 2 (berry like) type, 7 cases (41.2%) were type 3 (longitudinal) type, and 4 (23.5%) cases were type 4 (circumferential) type.
In angiography, except 3cases of C6 segment, every BBA located in C7 segment. And except fusiform aneurysm, most of all BBA located on antero-superior wall of ICA trunk (medial or lateral direction of the vessel wall). Size was various but except 3 cases (case 3, 11, 14), the aspect ratio (height/neck[mm]) lesser than 1.
There was 3 cases of configurationally change of aneurysms (case 2, 3, 14). One case (case 3) revealed intra operative pseudo-sac formation and the other 2 (case 2, 14) revealed the newly developed aneurysms, which was not detected in the first study performed on admission (
Table 3).
Preoperative evaluation
There were several preoperative options for the evaluation of a SAH patient. First of all, initial CT and CT angiography checked, and if the cause of rupture was estimated to be a BBA, TFCA had to performed as soon as possible.
When preoperative TFCA was decided to perform, temporary ICA occlusion test was done, for the evaluation of collaterals from anterior communicating (Acom) artery and posterior communicating (Pcom) artery. And External carotid artery (ECA) angiography was performed. For the preparation of possible EC-IC bypass.
Surgical procedure
Surgical procedure was proceeded as soon as possible. For internal cerebral pressure control, pre-operative continuous lumbar drainage procedure was done under general anesthesia state. When unexpected brain swelling was occurred, intraoperative extra ventricular drainage through Paine's point was done. (case 13, 15, 17) As the preparation about premature rupture of BBA, and cervical dissection had to be done before craniotomy in the early years of the treatment. But recently, the site of cervical ICA was marked before surgical drab.
Every surgical approach was done pterionally, and the superficial temporal artery was preserved during scalp dissection for the preparation of possible bypass. After craniotomy, anterior clinoid process was drilled out intradurally or extradurally, and optic canal was partially unroofed. Furthermore, optic sheath was opened if possible. Most of cases, 3rd cranial nerve, Pcom artery, and anterior choroidal artery were identified.
When targeted aneurysm was exposed, the permanent clip was applied after proximal control with temporary clip(s) in intracranial and/or extra cranial method.
Aneurysms were clipped by Sundt clip, conventional Yasargil clip or both (Sundt clip enforced by Yasargil clip) after peri-aneurysmal dissection was done. After the aneurysm was clipped, intraoperative transcranial Doppler was used for the evaluation of arterial patency. Sometimes, clip adjustment was done depending on the result of TCD.
Microsurgical treatment
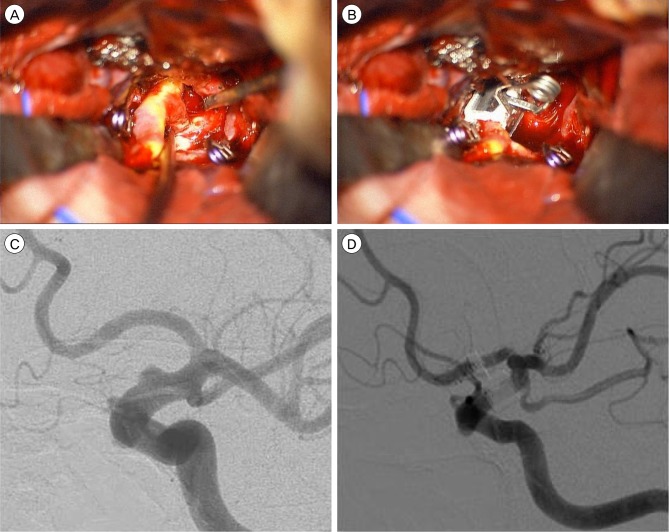
Among 17 BBA-patients, 14 patients got microsurgical clip operation initially. 8 (47. 0%) patients were clipped with Sundt clip. (
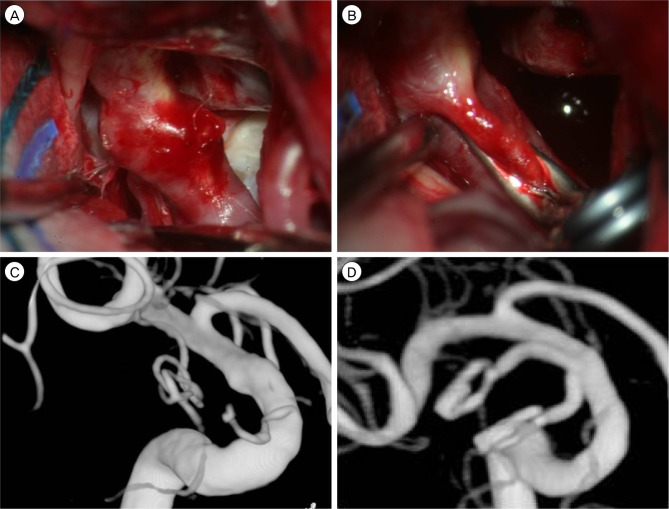
Fig. 1) 5 (29.4%) patients were clipped with conventional Yasargil clip (
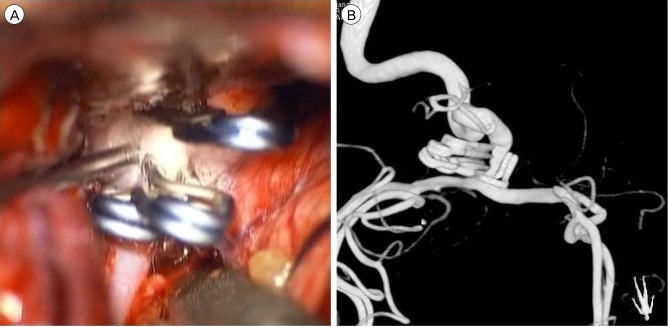
Fig. 2) and 1 (6%) patient was clipped aneurysm with wrapping (
Fig. 3). In two cases using conventional Yasargil clip, additional operation was needed after initial operation. One case (case 2) was due to post-operative rebleeding and the other case (case 10) was due to residual aneurysm sac, found in follow up angiography. (Finally, surgical trapping was done due to intraoperative aneurysmal rupture in re-operation). In cases using Sundt clip initially, there was no additional operation. But, there were 2 cases with additional work. In one case (case 6), additional two Yasargil clips were used for the both sides of aneurysmal margin after Sundt clip was applied. And the other case (case 15), bam sheet was used for control the tearing wall of aneurysm due to intraoperative rupture.
Endovascular treatment
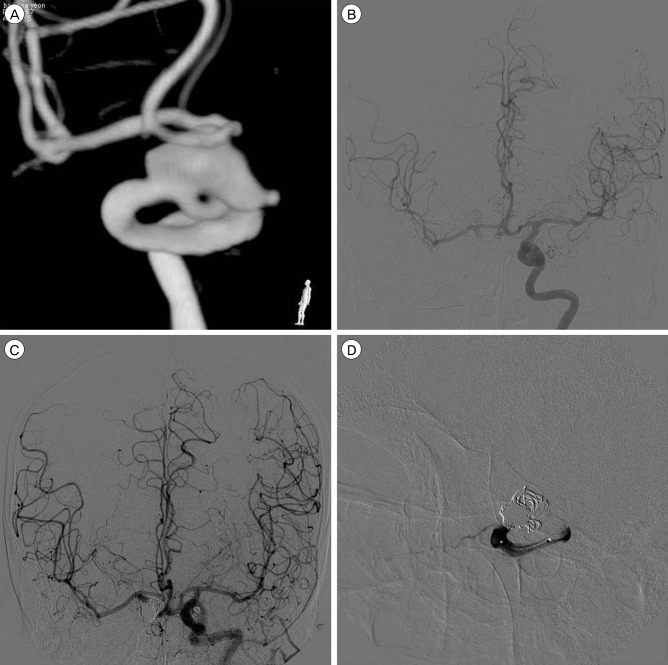
In 17 BBA patients, 2 (11.7%) patients underwent endovascular coiling, and 1 (6%) patient receive endovascular trapping of involved ICA (
Fig. 4). In one case (case 3), the morphology of aneurysm was similar to saccular type aneurysm and stent assisted coil embolization was tried initially. But the ruptured point of aneurysm was changed and pseudo sac formation was occurred during coil embolization. Consequently two additional reinforcing procedures including stent in stent technique were needed due to recannalization. The patient (case 9) who had been taken aspirin due to angina pectoris, had two additional aneurysms in both paraclinoid ventral walls. After additional two endovascular procedures, clipping using Sundt clip had to be done because of recurred recannalization. After Sundt clip application, there was no more recurrence in follow up checks for 6 years.
There was one case of endovascular trapping (case 11). In pre-operative TFCA, there were BBA and two additional aneurysms (Pcom artery aneurysm and saccular dorsal wall aneurysm) on the opposite side in involved ICA trunk. The collaterals through Acom and Pcom arteries were good. So, initially the endovascular trapping for the ruptured BBA and simple coiling for the unruptured Pcom artery aneurysm was done. 3 weeks later (after the condition of patient was improved), additional stent application was done for the small dorsal wall aneurysm. In this stage, coiling through the stent was failed.
Surgical outcome
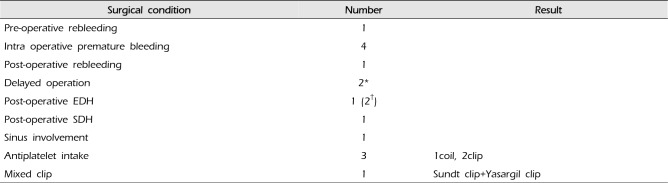
In 8 patients, treated with a Sundt clip, the technical success rate was 100% and there was no additional operation for aneurysmal treatment. In contrast, when Yasargil clip was applied, the rate of revision was 40% (2 cases from 5 Yasargil clip cases). And in endovascular coiling cases, 100% of revision rate was estimated. Revision was due to post-operative rebleeding or recurrence of aneurysm. In Sundt clip size (diameter × length, mm), 3 × 3 clip, 3 × 5 and 4 × 3 clip was used in 1 each case, 4 × 5 clip was used in 2 cases, 3.5 × 3 clip was used in 3 case.
In Yasargil clip, various type of clips were used, sometimes, 2-3 clips were used together. Right angled clip was most used type of clip (6 cases), and bent type clip and ring type clip used in 2 cases, and curved type clip also used in 1 case. There were one case using 2 kinds of clip together (Sundt clip and Yasargil clip) and one case using bam sheet with Sundt clip. In these cases, Yasargil clip and bam sheet were used for reinforcement of a Sundt clip-applied aneurysm. (case 6, case 15)
There was intraoperative premature bleeding in 4 cases, first case occurred when Sundt clip was slipped from ICA trunk (case 1), 2nd case was occurred during repositioning of the Sundt clip due to the low patency of parent artery after clipping. (case 2) In this case, involved ICA was trapped with multiple Yarsagil clip. last 2 cases the intraoperative bleeding occurred during cerebral dissection due to cerebral edema. (case 10, 15) (
Table 3,
4)
The luminal stenosis was occurred not only the cases of using Sundt clip, but also the case of Yasargil clip or wrapping. The severity stenosis of ICA trunk was measured by NASCET method (stenosis (%) = 1-(Dstenosis/Dnormal), D:diameter) The most severe stenosis was 30.2% which case was treated by wrapping (case 13). In Sundt clip case, maximal stenosis was 22.4% (case 9) and minimal stenosis was 5.0% (case 1). In Yarsagil clip, maximal stenosis was 24.0% (case 14) and minimal stenosis was 17.4% (case 8). Furthermore there was no case the luminal stenosis disturb the vascular patency in angiography. (
Table 3) the branches of ICA (Pcom artery, anterior choroidal artery) was preserved and the morphology of these arteries was unchanged.
Clinical outcome
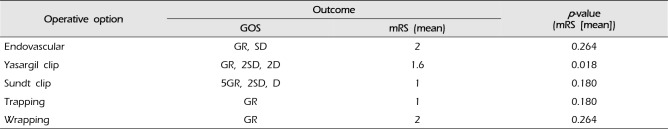
The clinical outcome was evaluated by the mRS and GOS at discharge. The clinical outcomes of each surgical option were estimated by comparing the mean score of the scale. In mRS system, cases of the Sundt clip and endovascular trapping (mean value = 1) were the better than cases of the Yasargil clip (mean value = 1.6) and endovascular coiling (mean value = 2) in clinical status of patients. In GOS scale, there was various levels of status in each case. But comparing the case of Yasargil clip and Sundt clip, the Sundt clip cases were tend to have good results (GR: SD: D=5:2:1) than the Yasargil clip cases (GR: SD: D=1:2:2). (
Table 1,
5) Even though, there was no difference in status of patients, when they had admitted via ER, between the case of Sundt clip and of Yasargil clip. (the mean value of Hunt-Hesse grade was 2.6 in Sundt clip case, 2.8 in Yasargil clip case, and 2.5 in endovascular coiling case)
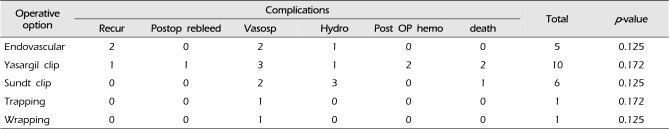
Although there was no statistical significance (
p-value > 0.05), the rate of recurrence and post-operative rebleeding were higher in cases of the endovascular coiling and the Yasargil clipping than in cases of the Sundt clip and endovascular trapping. Other surgical and clinical complications are detailed in
Table 4 and
6.
DISCUSSION
BBA is a kind of dorsal wall aneurysm arising from the trunk of ICA, and its characteristics which having the indefinite neck like fusiform aneurysm, and the fragility due to the lack of internal elastic layer
7) make the hazardous intraoperative and postoperative rebleeding. Furthermore, the acute configurational change
12) makes dynamic variables in the establishment of tactics in treatment of BBA.
After 1995, the time approved by FDA of the United states, the endovascular treatment has widen its influence by developing the stents, new materials and various tactics in the field of coiling. Because the fragile nature of the BBA and incomplete packing with a residual neck can make recurrence of aneurysm, which can be caused regrowing or rebleeding.
12) The endovascular coiling had been thought to be contraindication
7) and until now, although many endovascular trials was challenged, there were a limited result in treatment of BBA (not optimal treatment but optional procedure).
11)
Park et al.
15) suggested the trapping of involved parent ICA (with/without External-internal carotid artery bypass) should be first option for definite treatment in BBA, and they requested several options for the trapping. First of all, the patients have to pass the balloon occlusion test of involved ICA, and the evaluation of collateral circulation should be done by pre-operative TFCA.
13) Second, even the patients who have good collateral circulation, there are always the risk of ischemic injury by the vasospasm. So, there must be the preoperative preparation for the bypass surgery and the management for vasospasm in advance.
5) As the Kawashima et al.
10) already persisted, the trapping operation can be also worth as the choice of rescue when the surgical outcome of the direct clip or wrapping with clipping was insufficient.
In the case of wrapping, although there have been many trials to find out the proper wrapping materials like, cotton, muscle, fascia, gauze, Teflon, surgical glue, and etc. the essential problem of wrapping has been rebleeding.
8) The higher rate of rebleeding in wrapping alone has been reported and it is the obstacle of treatment. However, wrapping alone may not prevent rebleeding or regrowth of BBA, but wrapping with suturing or clipping can be useful choice for reinforcement of BBA. And new materials, (like silicon sheet) contribute to successful treatment with wrapping for BBA.
8)18)
Based on our results, use of the Sundt clip can be the first choice for treatment in BBA. The surgical and clinical outcomes of the Sundt clip operation were better than other surgical modalities. The Sundt clip operation could maintain the patency of involved vessel (compared with trapping) and solve the technical difficulty of suturing of the diseased vessel wall.
16)
For 14 years, 17 cases of BBA were treated and various surgical options were applied to the case of BBA, along the patients' conditions and medical histories. Besides the surgical modalities reported already (direct surgical clipping[Yasargil clip, Sundt clip], direct clipping with wraping, surgical or endovascular trapping with or without bypass, and endovascular coiling with stent),
15) there were some modification in the use of Sundt clip, such as Sundt clip with Yasargil clip, and Sundt clip with bam sheet. And surgical trapping was applied in case of intra-operative bleeding.
In the cases of Yarsagil clip operation, there was some cases of intraoperative bleeding and post-operative recurrence or rebleeding, and the prognosis was not favorable due to the complications like post-operative hemorrhage.
In the endovascular cases (coiling with stent[s]), the clinical outcome was not bad. But, because of frequent recannalization, additional operations were needed in every case.
In the cases of surgical trapping, which was done in the situation of intraoperative bleeding, it was not appropriate to evaluate the surgical outcome itself. In the case of endovascular trapping and wrapping with clipping, although the surgical and clinical outcomes were good, the insufficiency of number of case makes the statistic result was not meaningful.
The cases of the Sundt clip operation, there were 100% technically success rate, and their surgical and clinical outcomes were favorable. Although there were luminal stenosis (max: 22.4%, min: 5.0%) in follow up TFCA, there was no case which had any symptom associated with the stenosis. Luminal stenosis can be induced by not only Sundt clip but also Yasargil clip. In Yarsagil clip, there were maximal 24.0% and minimal 17.4% stenosis was estimated.
Cho et al.
2) and Cho et al.
3) reported separately the modified application of Sundt clip, which was placed over the stented or stent-associated coiled artery before Sundt clip operation. Besides, in case 5 and 20, there showed the other possibility of reinforcement of Sundt clip by Yasargil clip or bam sheet. This trial of combined maneuver of Sundt clip in treatment of BBA means the possibility of development of Sundt clip operation in the future.
The main problems of the operation using the Sundt clip is the possibility of the sacrifice of the branches of ICA. If the adjustable vessel-encircling clip, made of plastic is possible, this type clip could be modified according to the location of branches in the operating room. And, the clip could preserve the perforators of involved ICA, and make vessel-encircling clip more near to the optimal TOC for BBA.
To analyze what is the best option or optimal choice for treatment about specific disease, there must be enough population in each modality. 17 patients with BBA were not enough to elicit the general sentences. Especially the case of wrapping or endovascular trapping which had only 1 case each, and it was difficult to derive the tactical meaning.
In the processing of estimating in morphological entity of aneurysms by pre op TFCA or CT angiography, the acute configurational change of the BBA, whether the saccular type aneurysm was from BBA or not, was out of consideration in this article.
Finally, in the endovascular treatment, the newly introduced endovascular options, like flow diverter, was not considered in this article. Although the cases of flow diverter was reported with reasonable result. But their efficacy has to be validated in larger series.
5)17)




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download