Abstract
There are a number of complications associated with ventriculoperitoneal shunt (VPS) surgery. The authors present a rare case of iatrogenic common carotid artery injury during VPS surgery.
Ventriculoperitoneal shunt (VPS) surgery is the most common treatment for hydrocephalus. However, VPS surgery is associated with relatively high incidence of complications such as overdrainage of cerebrospinal fluid, infection and shunt malfunction. In this report, we report an intraoperative common carotid artery injury that occurred during VPS surgery. This case report gives a detailed example of this unreported complication, which necessitates an earlier intervention to result in a favorable outcome.
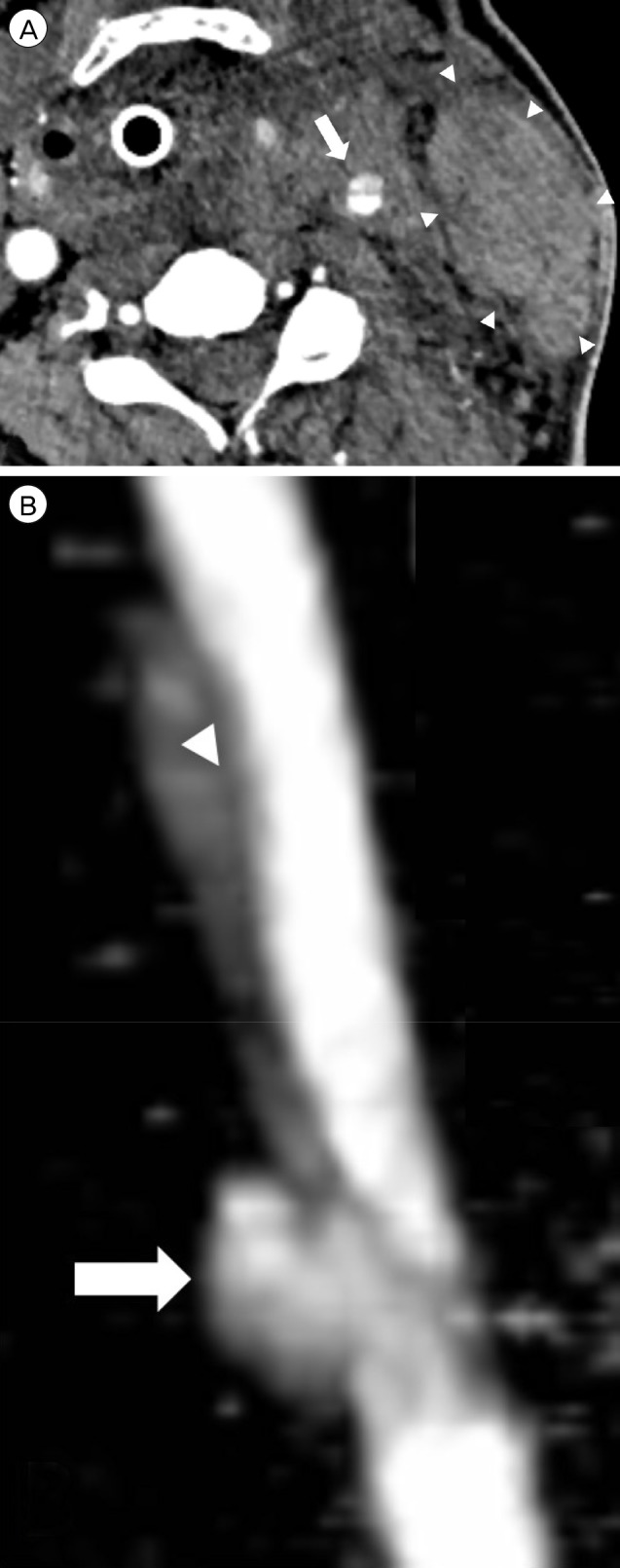
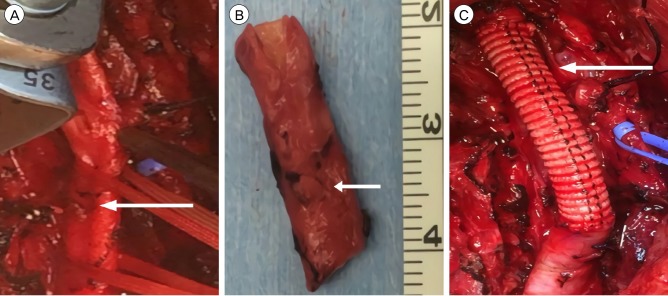
A 44-year-old male patient was diagnosed with hydrocephalus due to congenital aqueductal stenosis, and had been treated with VPS surgery at the age of 13 years. He subsequently underwent four revision operations to correct shunt malfunctions. He presented with gait disturbance, urinary incontinence, and mild dementia with an onset 4 months prior. Brain computed tomography (CT) showed ventriculomegaly with distal catheter malfunction on the shunt function test. A VPS revision surgery was planned, via the left frontal burr hole at Kocher's point. The distal catheter did not pull through the existing pathway due to adhesion with surrounding tissue and re-tunneling was decided. During tunneling from the peritoneum to the burr hole with a shunt passer, the neck became swollen. Although there was no change in vital signs, sudden neck swelling doubted bleeding. The surgery was immediately halted. Without extubation an emergency CT angiography of the neck was performed, which revealed accidental dissection of the left common carotid artery with a large amount of hematoma (Fig. 1). The heart surgery team was contacted; they resected the ruptured left common carotid artery, which was replaced with a vascular graft (Fig. 2). On the following day, the patient underwent a VPS surgery via the right Kocher's point. The postoperative follow-up imaging study, demonstrated a decreased ventricle size and a patent left common carotid artery graft, without any contrast leakage. The patient recovered uneventfully with slightly improved gait ataxia and was transferred to a rehabilitation hospital. Follow up brain CT and neck CT angiography, after 2 months, revealed decreased ventricle size and a patent common carotid artery graft. Thereafter, his cognition is deteriorating. However, his mother refused consent for further evaluation. Currently, a year after the operation, he is residing at a nursing home for supportive care.
VPS surgery is the most common procedure for treating hydrocephalus; however, it is associated with a relatively high incidence of complications.5) Complications associated with shunt procedures include overdrainage, infection, valve failure, breakage of the catheter, and catheter obstruction. It is also possible for shunt components to extrude through the skin, particularly after multiple operations, migrate, or perforate into different cavities or viscera.1)4)6)9) Iatrogenic pneumothorax after a VPS surgery and jugular vein injury during the tunneling process has also been reported.2)7)8) However, to our knowledge, intraoperative common carotid artery injury, during VPS surgery, has not been reported.
In this case, multiple revision VPS history might be the reason for common carotid artery injury. Adhesion with surrounding tissue due to multiple VPS surgeries makes tunneling with a shunt passer difficult. We suggest that particular precaution to avoid carotid artery injury should be taken, especially in revision VPS surgery. Additionally, early identification of the injury event and timely intervention can prevent further serious complications and can favorably alter the prognosis. However, a lack of follow-up is the limitation of this case report.
Intraoperative common carotid artery injury during VPS surgery has not been reported. The consequences of carotid artery injury can be fetal with high mortality.3) This case report gives a detailed example of this unreported complication, which necessitates an earlier intervention to result in a favorable outcome.
References
1. Cheng JY, Lo WC, Liang HH, Kun IH. Migration of ventriculoperitoneal shunt into the stomach, presenting with gastric bleeding. Acta Neurochir (Wien). 2007; 12. 149(12):1269–1270. PMID: 17999030.

2. Hermann EJ, Zimmermann M, Marquardt G. Ventriculoperitoneal shunt migration into the pulmonary artery. Acta Neurochir (Wien). 2009; 6. 151(6):647–652. PMID: 19350205.

3. Inamasu J, Guiot BH. Iatrogenic carotid artery injury in neurosurgery. Neurosurg Rev. 2005; 10. 28(4):239–247. PMID: 16091974.

4. Keong NC, Czosnyka M, Czosnyka Z, Pickard JD. Clinical Evaluation of Adult Hydrocephalus. Youmans Neurological Surgery. Ed 6. Philadelphia: WB Saunders;2011. p. 494–514.
5. Merkler AE, Ch'ang J, Parker WE, Murthy SB, Kamel H. The rate of complications after ventriculoperitoneal shunt surgery. World Neurosurg. 2017; 2. 98:654–658. PMID: 27826086.

6. Oktem IS, Akdemir H, Koc K, Menku A, Tucer B, Selcuklu A, et al. Migration of abdominal catheter of ventriculoperitoneal shunt into the scrotum. Acta Neurochir (Wien). 1998; 140(2):167–170. PMID: 10398996.
7. Rizk E, Dias MS, Verbrugge J, Boop FA. Intracardiac migration of a distal shunt catheter: an unusual complication of ventricular shunts. Report of 2 cases. J Neurosurg Pediatr. 2009; 6. 3(6):525–528. PMID: 19485740.
8. Schul DB, Wolf S, Lumenta CB. Iatrogenic tension pneumothorax resulting in pneumocephalus after insertion of a ventriculoperitoneal shunt: an unusual complication. Acta Neurochir (Wien). 2010; 1. 152(1):143–144. PMID: 19399364.

9. Wiwattanadittakul N, Katanyuwong K, Jetjumnong C, Sittiwangkul R, Makonkawkeyoon K. Pericardial effusion and cardiac tamponade after ventriculoperitoneal shunt placement: a case report. Acta Neurochir (Wien). 2016; 10. 158(10):2019–2021. PMID: 27502774.

Fig. 1
(A) Axial CT angiography after VPS surgery showing dissection of the left common carotid artery (arrow) with a large hematoma (arrow heads). (B) Reconstructed image of the dissected left common carotid artery. Pseudoaneurysm (arrow) and intramural hematoma (arrow head). CT = computed tomography; VPS = ventriculoperitoneal shunt.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download