This article has been
cited by other articles in ScienceCentral.
Abstract
The most common complication of coil embolization for cerebral aneurysms is thrombo-embolic stroke; in rare cases, these strokes, can present with central retinal artery occlusion. At our institution, a 53-year-old woman underwent stent-assisted coiling of the aneurysm. The patient's vision was improved immediately after intra-arterial thrombolysis and had further improved 8 months later. This report describes our experience of a rare case of central retinal artery occlusion after coil embolization that was successfully treated by intra-arterial thrombolysis.
Go to :

Keywords: Central retinal artery occlusion, Embolization, Thrombolysis, Paraclinoid aneurysm
INTRODUCTION
Advances in microcatheter technology, endovascular techniques, and embolization materials have increased the popularity of neuro-interventional therapy for paraclinoid aneurysms. The most common complication of coil embolization for cerebral aneurysms is thrombo-embolic stroke; in rare cases, these strokes can present with ipsilateral loss of vision caused by central retinal artery occlusion (CRAO).
7) In this report, we describe a patient who experienced a sudden loss of vision eight hours after coiling of a paraclinoid aneurysm and was successfully treated by intra-arterial thrombolysis; we also review other relevant cases reported in the literature.
Go to :

CASE REPORT
A 53-year-old woman visited our institution due to a headache. The computer tomography (CT) angiography revealed the unruptured aneurysm at the left internal carotid artery (ICA). Trans-femoral cerebral angiography (TFCA) performed in other hospital indicated that the paraclinoid segment and contained an aneurysm that measured 6.7 mm in diameter and had a bleb. We planned stent-assisted coiling of the aneurysm. After we administered aspirin (300 mg) and clopidogrel (300 mg) to the patients before the procedure, a total of 6 bare platinum coils (Target®Nano, Stryker Neurovascular, Fremont, CA, USA) were packed into the aneurysm with the stent system. Anticoagulation was initiated by the injection of a bolus of 3,000 IU heparin (Green Cross Corp., Yongin, Korea) that was intravenously administered immediately after femoral puncture, followed by an hourly intermittent bolus injection of 1,000 IU heparin. Coil embolization was performed through a single femoral access in the case with a 7F guiding catheter (Boston Scientific, Natick, MA, USA). Because the selection for the aneurysm was difficult, the guide wire was frequently passed by the ophthalmic artery. A partial coil packing of an an aneurysm was performed to reduce the risk of an unexpected rupture of an aneurysm due to interference between the two microcatheters prior to the advancement of the Neuroform EZ stent delivery system (Stryker Neurovascular, Fremont, CA, USA) into the delivery XT-27 microcatheter (Stryker Neurovascular, Fremont, CA, USA).
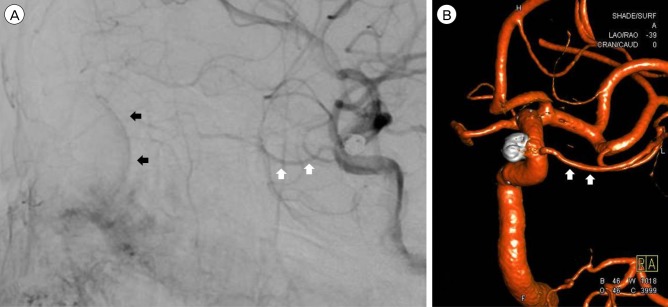
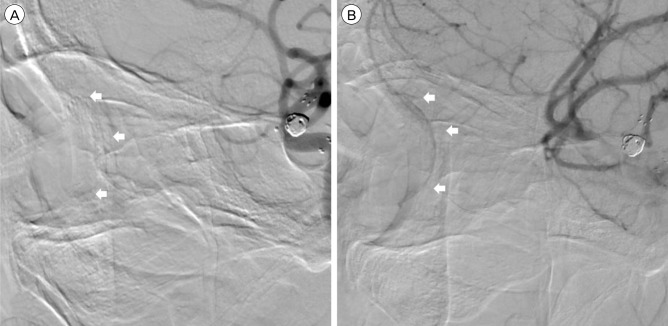
Post-procedural angiography revealed complete obliteration of the aneurysm, and the ophthalmic artery remained patent with a choroidal blush (
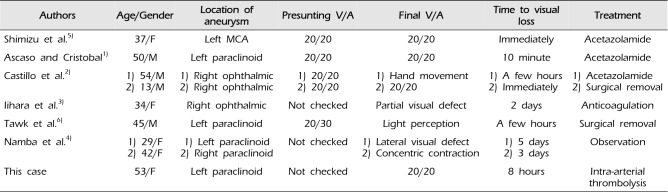
Fig. 1). However, eight hours later, the patient experienced suddenly complete visual loss in her left eye without other neurological deficits. Because we suspected the injury of ophthalmic artery by the guide wire passed frequently, the TFCA was immediately preformed without the CT or the magnetic resonance imaging. A follow-up angiogram of the left ICA revealed that the choroidal blush which presented immediately after coiling of the aneurysm, could not be visualized (
Fig. 2A) without any external carotid artery collaterals. Therefore, we performed emergent intra-arterial thrombolysis to treat this patient in accordance with a diagnosis of CRAO based on clinical examination and angiographic images. After this microcatheter (Excelsior® SL-10, Stryker Neurovascular, Fremont, CA, USA) was placed in the proximal segment of the ophthalmic artery, 100,000 IU of urokinase (Creen Cross, Corp., Yongin, Korea) and 500 mcg of Aggrastat (a glycoprotein IIb/IIIa inhibitor, tirofiban, MSD, Kenilworth, NJ, USA) were hand-injected. The patient's left eye exhibited marked improvement in vision (up to finger counting). A left ICA angiogram after thrombolysis revealed improved visualization of the choroidal blush (
Fig. 2B). A complete ophthalmological confirmed that the patient's vision had partially recovered and that she could count fingers.
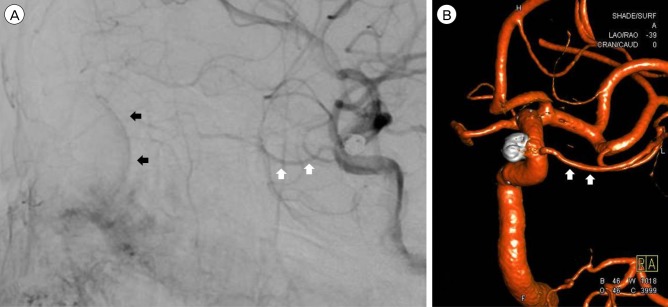 | Fig. 1Postcoiling angiogram demonstrates the complete obliteration of the aneurysm. (A) A lateral view and (B) a 3D reconstructed angiogram demonstrate the complete obliteration of the aneurysm with nine platinum coils. The ophthalmic artery (white arrows) and a contrast enhancement of the posterior eye bulb, a phenomenon known as -choroidal blush (black arrows) are visible immediately proximal to the aneurysm and remain patent in the post-embolization angiogram.
|
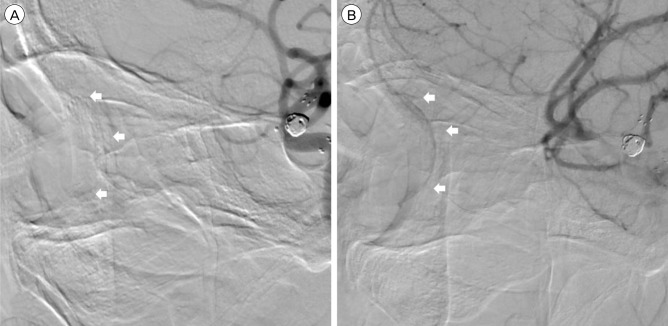 | Fig. 2After intra-arterial thrombolysis, the intensity of the choroidal blush is increased. (A) A left ICA angiogram (lateral view) before thrombolysis demonstrates the absence of the choroidal blush (white arrow). (B) A left ICA angiogram (lateral view) obtained after intra-arterial thrombolysis with 500,000 U of urokinase and 1,000 mcg of Aggrastat demonstrates an increase in the intensity of the choroidal blush (white arrow). ICA = internal carotid artery.
|
Go to :

DISCUSSION
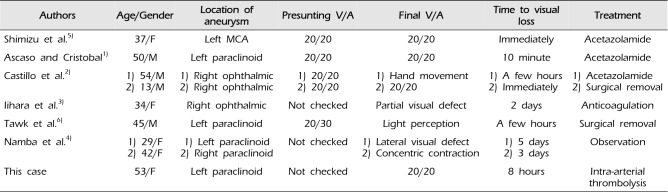
The most common causes of retinal artery occlusion are an embolus and a thrombus, although an embolus is observable in only 20% of patients with retinal artery occlusion. In our review, it was extremely rare that emboli or thrombi from coil embolization of ICA aneurysms caused CRAO (
Table 1).
1)2)3)4)5)6) In the described case, the inadvertent insertion of the microcatheter or microwire into the orifice of the ophthalmic artery might have caused endothelial injury. Despite the continuous flushing of the catheter and systemic heparization, this injury most likely affected thrombus formation near the injured orifice of the ophthalmic artery, resulting in embolic occlusion of the retinal artery.
Table 1
Manifestations of retinal arterial occlusion after coil embolization of ICA aneurysm in the literature
|
Authors |
Age/Gende |
Location of aneurysm |
Presunting V/A |
Final V/A |
Time to visual loss |
Treatment |
|
Shimizu et al.5)
|
37/F |
Left MCA |
20/20 |
20/20 |
Immediately |
Acetazolamide |
|
Ascaso and Cristobal1)
|
50/M |
Left paraclinoid |
20/20 |
20/20 |
10 minute |
Acetazolamide |
|
Castillo et al.2)
|
1) 54/M |
1) Right ophthalmic |
1) 20/20 |
1) Hand movement |
1) A few hours |
1) Acetazolamide |
|
2) 13/M |
2) Right ophthalmic |
2) 20/20 |
2) 20/20 |
2) Immediately |
2) Surgical removal |
|
Iihara et al.3)
|
34/F |
Right ophthalmic |
Not checked |
Partial visual defect |
2 days |
Anticoagulation |
|
Tawk et al.6)
|
45/M |
Left paraclinoid |
20/30 |
Light perception |
A few hours |
Surgical removal |
|
Namba et al.4)
|
1) 29/F |
1) Left paraclinoid |
Not checked |
1) Lateral visual defect |
1) 5 days |
Observation |
|
2) 42/F |
2) Right paraclinoid |
2) Concentric contraction |
2) 3 days |
|
This case |
53/F |
Left paraclinoid |
Not checked |
20/20 |
8 hours |
Intra-arterial |
|
thrombolysis |

Generally, CRAO is associated with a poor visual prognosis, with 61% of patients exhibiting a final visual acuity of 6/120 or worse. However, the visual prognosis for CRAO following coil embolization is not well established. A review of 9 cases, including the described patient, demonstrated that final visual acuity nearly could be returned to the pre-CRAO baseline level if visual loss occurred immediately after coil embolization. In contrast, if visual loss occurred after several hours or days, good recovery of visual acuity was unlikely. This might be related with the fact that earlier symptom onset can influence less delay of the time interval between symptom onset and the treatment. A critical consideration for improving CRAO-induced visual acuity loss is that early identification may be closely related to a patient's final visual acuity.
A meta-analysis reported that intra-arterial thrombolysis could potentially provide benefits relative to other conventional and conservative treatments; in particular, improvements in visual deficits were reported in up to 66% of thrombolysis treated patients. Furthermore, local flushing might support recanalization of the occluded vessel. As a first instance of intra-arterial thrombolysis for CRAO after coil embolization, the patient described in this study was successfully treated by intra-arterial thrombolysis with urokinase. When visual loss occurs abruptly after endovascular coiling, CRAO should be considered as a potential cause of this symptom. Following a diagnosis of CRAO, prompt acute and ongoing management is needed to prevent permanent visual disability. Intra-arterial thrombolysis can be recommended as a treatment option for CRAO after coil embolization.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download