Abstract
Pure subdural hematomas caused by a ruptured intracranial aneurysm are extremely rare. We describe the case of a 42-year-old woman who presented with headache without evidence of head trauma. Magnetic resonance angiography and conventional cerebral angiography revealed a ruptured aneurysm at the right middle cerebral artery bifurcation. The patient underwent surgical treatment and had a good outcome without any neurological deficit. The mechanisms and clinical characteristics of this condition are discussed.
In most cases, subdural hematomas (SDHs) are caused by head trauma.7)33) Spontaneous SDH is an uncommon condition, found in only 2.6% of acute subdural hematoma (ASDH) cases. Underlying etiologies for spontaneous SDH include ruptured aneurysms with or without concomitant subarachnoid hemorrhage (SAH), arteriovenous malformations, meningiomas, dural metastatic diseases, and hematologic or solid neoplasm.7)
Spontaneous pure ASDH without concomitant SAH due to the rupture of a cerebral aneurysm is extremely rare and only 40 cases were reported between 1981 and 2012.9)23)35) We report a case of spontaneous ASDH without evidence of SAH caused by a ruptured aneurysm at the middle cerebral artery (MCA) bifurcation, presenting with repeated sentinel headaches.
A 42-year-old woman was admitted to our institution with a history of sudden onset headache without any accompanying neurological deficit. A week prior to admission, the patient experienced two episodes of transient headache, each lasting a few hours. She had noted occasional headaches over the last few years; however, they did not last more than a few minutes and were not severe. She had no definite history of head trauma, hypertension, or coagulopathy.
The initial computed tomography (CT) scan of the brain revealed an ASDH without evidence of any other type of hemorrhage including SAH (Fig. 1), and laboratory studies, including coagulopathy screening, showed no abnormalities. For further evaluation, magnetic resonance angiography (MRA) and subsequent conventional cerebral angiography were conducted, revealing a right middle cerebral artery bifurcation aneurysm (Fig. 2).
An aneurysmal neck clipping surgery was performed on the second day of hospitalization. A right pterional approach was used as usual, but when a semi-lunar shaped dural incision was made, only a dark bloody SDH without SAH was noted. There was no discoloration of brain parenchyma; no hematoma was observed in the subarachnoid space. After total removal of the SDH, sylvian fissure dissection was performed and the aneurysm was identified at the middle cerebral artery bifurcation. The aneurysmal dome extended antero-inferiorly and laterally and was tightly adherent to the arachnoid membrane (Fig. 3). Postoperative CT revealed resolution of the ASDH without any complications related to the surgery. The patient's hospitalization was uneventful and a follow-up three-dimensional CT angiography performed 1 year after the operation showed no remnant or recurrent aneurysm (Fig. 4).
The mechanism of ASDH caused by rupture of an intracranial aneurysm is different from that of ASDH caused by trauma and tearing of cortical and bridging veins.10) According to previous studies, various mechanisms have been suggested to explain the occurrence of ASDH without SAH after aneurysm rupture. First, previous repeated minor ruptures of the aneurysm occur, causing small bleeds and the formation of tight adhesions between the aneurysm and the neighboring arachnoid membrane. Eventually, massive bleeding fills the subdural space directly after a major rupture occurs.8)16)23)25) Second, massive high-pressure bleeding causes laceration of the arachnoid membrane with bleeding into the subdural space.8)14)15)16)18) Third, the rupture of a subdural carotid artery aneurysm results in a pure ASDH.12)15)24) Fourth, the cavernous sinus wall is eroded by the acute enlargement of an intracavernous aneurysm after thrombosis, leading to pure ASDH.18)35)
In the present case, intraoperative findings revealed a tight adhesion between the aneurysmal dome and the arachnoid membrane. The patient reported recurrent episodes of sentinel headache, suggesting that repeated small bleedings led to formation of the tight adhesion. These findings are consistent with the first mechanism described above.
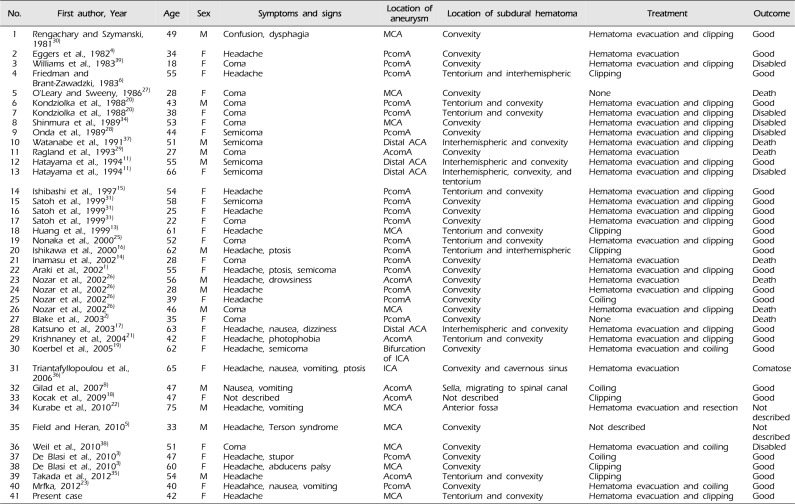
Including the present case, we analyzed 41 cases reported with pure ASDH caused by the rupture of an intracranial aneurysm and have summarized them in Table 1. Of these, 10 were caused by the rupture of an MCA aneurysm, including the present case. In those cases, ASDH was located at the convexity in seven cases, at both the tentorium and convexity in two cases (including the present case), and at the anterior fossa in one case. Six of these 10 cases underwent hematoma evacuation and clipping, as in the present case, and two cases underwent clipping only. In one case, surgery could not be performed, and in another case, treatment was not described. These 10 cases presented with a variety of symptoms and signs and experienced different outcomes. Four cases were comatose at admission, and, in these patients, the final outcomes were poor; two patients died and the other two patients were disabled. The other six cases presented with an alert to confused mental status with headache and/or other minor neurological deficits; in four cases, the final outcomes were reported to be good, and there was no description of outcome in the other two cases.
Among all 41 cases analyzed, 17 patients presented with a semi-comatose to comatose mental status on admission, and only five of these patients (29%) had good outcomes. Six patients died and another six patients were disabled. The remaining 24 cases with a relatively good neurological status had generally good outcomes. Excluding two cases without outcome description, 91% (20/22 patients) had good outcomes, one patient died, and one patient remained comatose. Based on these results, it appears that a favorable neurological status at admission is a predictive factor for a good outcome. These findings are consistent with those of Schuss et al. who studied patients with ASDH and SAH, and concluded that a good neurological status at admission is a predictive factor for a good outcome.32)
The rupture of an intracranial aneurysm may be the cause of a pure ASDH in patients without a history of trauma, but this is often mistakenly ruled out because of the absence of SAH. Subsequently, determining the correct cause and providing the proper treatments in these patients may be delayed.
Therefore, when a patient presents with a pure SDH without a history of trauma or coagulopathy, imaging studies, such as three-dimensional CT angiography or MRA, should be performed to evaluate for vascular lesions to determine the underlying cause and to guide optimal treatment for the patient.
References
1. Araki T, Sampei T, Murata H, Fujiwara H, Taki W. A case of internal carotid-posterior communicating artery aneurysm presenting pure acute subdural hematoma. No Shinkei Geka. 2002; 8. 30(8):861–866. PMID: 12187732.
2. Blake G, James M, Ramjit C, Char G, Hunter R, Crandon I. Acute subdural haematoma without subarachnoid haemorrhage caused by rupture of an intracranial aneurysm. West Indian Med J. 2003; 3. 52(1):80–81. PMID: 12806769.
3. De Blasi R, Salvati A, Renna M, Chiumarulo L. Pure subdural hematoma due to cerebral aneurysmal rupture: an often delayed diagnosis. Cardiovasc Intervent Radiol. 2010; 8. 33(4):870–873. PMID: 20012041.

4. Eggers FM, Tomsick TA, Lukin RR, Chambers AA. Recognition of subdural hematoma secondary to ruptured aneurysm by computerized tomography. Comput Radiol. 1982; Sep-Oct. 6(5):309–313. PMID: 7172650.

5. Field TS, Heran MK. Teaching NeuroImages: middle cerebral artery aneurysm rupture presenting as pure acute subdural hematoma. Neurology. 2010; 1. 74(4):e13. PMID: 20101029.

6. Friedman MB, Brant-Zawadzki M. Interhemispheric subdural hematoma from ruptured aneurysm. Comput Radiol. 1983; Mar-Apr. 7(2):129–134. PMID: 6851500.

7. Gerard C, Busl KM. Treatment of acute subdural hematoma. Curr Treat Options Neurol. 2014; 1. 16(1):275. PMID: 24363148.

8. Gilad R, Fatterpekar GM, Johnson DM, Patel AB. Migrating subdural hematoma without subarachnoid hemorrhage in the case of a patient with a ruptured aneurysm in the intrasellar anterior communicating artery. AJNR Am J Neuroradiol. 2007; Nov-Dec. 28(10):2014–2016. PMID: 17921232.

9. Gong J, Sun H, Shi XY, Liu WX, Shen Z. Pure subdural haematoma caused by rupture of middle cerebral artery aneurysm: case report and literature review. J Int Med Res. 2014; 4. 42(3):870–878. PMID: 24691457.

10. Handel SF, Perpetuo FOL, Handel CH. Subdural hematomas due to ruptured cerebral aneurysms: angiographic diagnosis and potential pitfall for CT. AJR Am J Roentgenol. 1978; 3. 130(3):507–509. PMID: 415559.

11. Hatayama T, Shima T, Okada Y, Nishida M, Yamane K, Okita S, et al. Ruptured distal anterior cerebral artery aneurysms presenting with acute subdural hematoma: report of two cases. No Shinkei Geka. 1994; 6. 22(6):577–582. PMID: 8015681.
12. Ho TL, Lee KW, Lee HJ. Acute massive subdural hematoma caused by rupture of internal carotid artery aneurysm during angiography: a case report. Emerg Radiol. 2002; 10. 9(4):237–239. PMID: 15290570.

13. Huang D, Abe T, Kojima K, Tanaka N, Watanabe M, Ohkura A, et al. Intracystic hemorrhage of the middle fossa arachnoid cyst and subdural hematoma caused by ruptured middle cerebral artery aneurysm. AJNR Am J Neuroradiol. 1999; 8. 20(7):1284–1286. PMID: 10472987.
14. Inamasu J, Saito R, Nakamura Y, Ichikizaki K, Suga S, Kawase T, et al. Acute subdural hematoma caused by ruptured cerebral aneurysms: diagnostic and therapeutic pitfalls. Resuscitation. 2002; 1. 52(1):71–76. PMID: 11801351.

15. Ishibashi A, Yokokura Y, Sakamoto M. Acute subdural hematoma without subarachnoid hemorrhage due to ruptured intracranial aneurysm - case report. Neurol Med Chir (Tokyo). 1997; 7. 37(7):533–537. PMID: 9259152.
16. Ishikawa E, Sugimoto K, Yanaka K, Ayuzawa S, Iguchi M, Moritake T, et al. Interhemispheric subdural hematoma caused by a ruptured internal carotid artery aneurysm: case report. Surg Neurol. 2000; 7. 54(1):82–86. PMID: 11024512.

17. Katsuno M, Murai Y, Teramoto A. Acute subdural hematoma without subarachnoid hemorrhage following rupture of a distal anterior cerebral artery aneurysm: a case report. No To Shinkei. 2003; 5. 55(5):435–438. PMID: 12833887.
18. Kocak A, Ates O, Durak A, Alkan A, Cayil S, Sarac K. Acute subdural hematomas caused by ruptured aneurysms: experience from a single Turkish center. Turk Neurosurg. 2009; 10. 19(4):333–337. PMID: 19847751.
19. Koerbel A, Ernemann U, Freudenstein D. Acute subdural haematoma without subarachnoid haemorrhage caused by rupture of an internal carotid artery bifurcation aneurysm: case report and review of literature. Br J Radiol. 2005; 7. 78(931):646–650. PMID: 15961850.

20. Kondziolka D, Bernstein M, ter Brugge K, Schutz H. Acute subdural hematoma from ruptured posterior communicating artery aneurysm. Neurosurgery. 1988; 1. 22(1Pt1):151–154. PMID: 3344078.

21. Krishnaney AA, Rasmussen PA, Masaryk T. Bilateral tentorial subdural hematoma without subarachnoid hemorrhage secondary to anterior communicating artery aneurysm rupture: a case report and review of the literature. AJNR Am J Neuroradiol. 2004; Jun-Jul. 25(6):1006–1007. PMID: 15205138.
22. Kurabe S, Ozawa T, Fujiwara H, Watanabe T, Aiba T. Peripheral intracranial aneurysm causing subdural hematoma without subarachnoid hemorrhage. Neurology. 2010; 1. 74(3):268. PMID: 20083805.

23. Mrfka M, Pistracher K, Augustin M, Kurschel-Lackner S, Mokry M. Acute subdural hematoma without subarachnoid hemorrhage or intraparenchymal hematoma caused by rupture of a posterior communicating artery aneurysm: case report and review of the literature. J Emerg Med. 2013; 6. 44(6):e369–e373. PMID: 23561314.
24. Nishikawa T, Ueba T, Kajiwara M, Yamashita K. Bilateral acute subdural hematomas with intracerebral hemorrhage without subarachnoid hemorrhage, caused by rupture of an internal carotid artery dorsal wall aneurysm. Case report. Neurol Med Chir (Tokyo). 2009; 4. 49(4):152–154. PMID: 19398858.
25. Nonaka Y, Kusumoto M, Mori K, Maeda M. Pure acute subdural haematoma without subarachnoid haemorrhage caused by rupture of internal carotid artery aneurysm. Acta Neurochir (Wien). 2000; 8. 142(8):941–944. PMID: 11086835.

26. Nozar A, Philippe D, Fabrice P, Silvia M, Marc T. Acute pure spontaneous subdural haematoma from ruptured intracranial aneurysms. Interv Neuroradiol. 2002; 12. 8(4):393–398. PMID: 20594500.

27. O'Leary PM, Sweeny PJ. Ruptured intracerebral aneurysm resulting in a subdural hematoma. Ann Emerg Med. 1986; 8. 15(8):944–946. PMID: 3740583.
28. Onda J, Kodama Y, Emoto K, Yuki K. A case report of "pure" acute subdural hematoma secondary to ruptured intracranial aneurysm. Kyukyu Igaku. 1989; 13:631–634.
29. Ragland RL, Gelber ND, Wilkinson HA, Knorr JR, Tran AA. Anterior communicating artery aneurysm rupture: an unusual cause of acute subdural hemorrhage. Surg Neurol. 1993; 11. 40(5):400–402. PMID: 8211657.

30. Rengachary SS, Szymanski DC. Subdural hematomas of arterial origin. Neurosurgery. 1981; 2. 8(2):166–172. PMID: 7207782.

31. Satoh K, Sasaki T, Osato T, Ozaki Y, Masui S, Hyogo T, et al. Intracranial aneurysm presenting as acute subdural hematoma without subarachnoid hemorrhage: report of three cases. J Hokkaido Brain Res Found. 1999; 8:27–31.
32. Schuss P, Konczalla J, Platz J, Vatter H, Seifert V, Güresir E. Aneurysm-related subarachnoid hemorrhage and acute subdural hematoma: single-center series and systematic review. J Neurosurg. 2013; 5. 118(5):984–990. PMID: 23289820.

33. Shin DW, Choi CY, Lee CH. Spontaneously rapid resolution of acute subdural hemorrhage with severe midline shift. J Korean Neurosurg Soc. 2013; 11. 54(5):431–433. PMID: 24379953.

34. Shinmura F, Nakajima S, Maruyama T, Azuma S. A case of ruptured middle cerebral artery aneurysm with acute subdural hematoma after clipping of the aneurysm nine years previously. No Shinkei Geka. 1989; 12. 17(12):1175–1179. PMID: 2693986.
35. Takada T, Yamamoto T, Ishikawa E, Zaboronok A, Kujiraoka Y, Akutsu H, et al. Acute subdural hematoma without subarachnoid hemorrhage caused by ruptured A1-A2 junction aneurysm. Neurol Med Chir (Tokyo). 2012; 6. 52:430–434. PMID: 22729076.

36. Triantafyllopoulou A, Beaumont A, Ulatowski J, Tamargo RJ, Varelas PN. Acute subdural hematoma caused by an unruptured, thrombosed giant intracavernous aneurysm. Neurocrit Care. 2006; 5(1):39–42. PMID: 16960293.

37. Watanabe K, Wakai S, Okuhata S, Nagai M. Ruptured distal anterior cerebral artery aneurysms presenting as acute subdural hematoma - report of three cases. Neurol Med Chir (Tokyo). 1991; 8. 31(8):514–517. PMID: 1722880.
38. Weil AG, McLaughlin N, Lessard-Bonaventure P, Bojanowski MW. A misleading distal anterior cerebral artery aneurysm. Surg Neurol Int. 2010; 9. 1:55. PMID: 20975973.

39. Williams JP, Joslyn JN, White JL, Dean DF. Subdural hematoma secondary to ruptured intracranial aneurysm: computed tomographic diagnosis. J Comput Tomogr. 1983; 5. 7(2):142–153. PMID: 6872560.

Fig. 1
Initial brain imaging findings of case. Computed tomography scans (A, B) shows no evidence of subarachnoid hemorrhage at the basal cistern and the sylvian fissure and there is only acute subdural hematoma on the right fronto-temporo-parietal area.
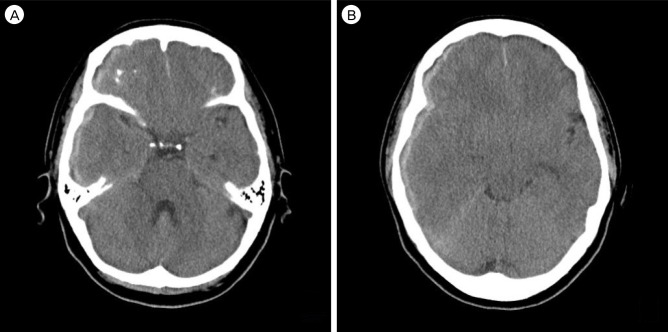
Fig. 2
Magnetic resonance angiography (A, B; white arrows) and conventional cerebral angiography (C, D; white arrows) show the presence of the right middle cerebral artery bifurcation aneurysm extending antero-inferiorly and laterally.
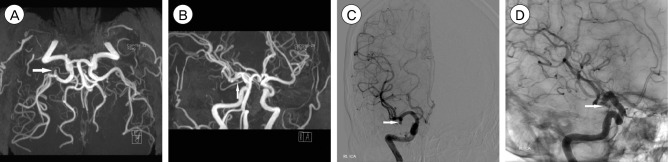
Fig. 3
Intraoperative photographs shows the aneurysmal sac penetrating into subdural space (A; white arrow). Permanent 7 mm straight mini-clip was introduced to the neck portion of the aneurysm successfully (B).
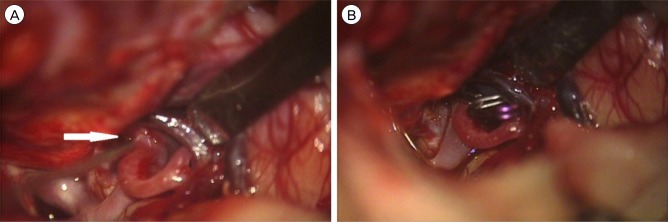
Fig. 4
Follow-up computed tomography angiography 1-year after the operation. The clip is observed in the source image of the computed tomography angiography (A), and there was no evidence of the remnant aneurysm (A, B).
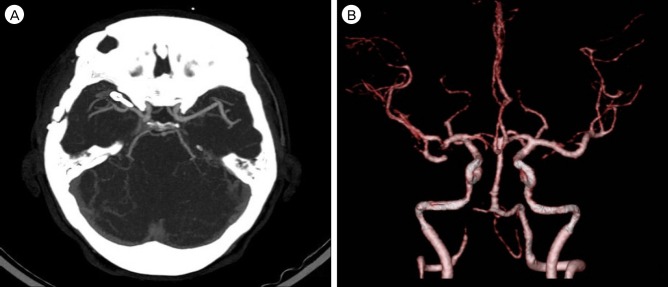
Table 1
Cases of pure acute subdural hematoma caused by the rupture of intracranial aneurysm
| No. | First author, Year | Age | Sex | Symptoms and signs | Location of aneurysm | Location of subdural hematoma | Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|
| 1 | Rengachary and Szymanski, 198130) | 49 | M | Confusion, dysphagia | MCA | Convexity | Hematoma evacuation and clipping | Good |
| 2 | Eggers et al., 19824) | 34 | F | Headache | PcomA | Convexity | Hematoma evacuation | Good |
| 3 | Williams et al., 198339) | 18 | F | Coma | PcomA | Convexity | Hematoma evacuation and clipping | Disabled |
| 4 | Friedman and Brant-Zawadzki, 19836) | 55 | F | Headache | PcomA | Tentorium and interhemispheric | Clipping | Good |
| 5 | O'Leary and Sweeny, 198627) | 28 | F | Coma | MCA | Convexity | None | Death |
| 6 | Kondziolka et al., 198820) | 43 | M | Coma | PcomA | Tentorium and convexity | Hematoma evacuation and clipping | Good |
| 7 | Kondziolka et al., 198820) | 38 | F | Coma | PcomA | Tentorium and convexity | Hematoma evacuation and clipping | Disabled |
| 8 | Shinmura et al., 198934) | 53 | F | Coma | MCA | Convexity | Hematoma evacuation and clipping | Disabled |
| 9 | Onda et al., 198928) | 44 | F | Semicoma | PcomA | Convexity | Hematoma evacuation and clipping | Disabled |
| 10 | Watanabe et al., 199137) | 51 | M | Semicoma | Distal ACA | Interhemispheric and convexity | Hematoma evacuation and clipping | Death |
| 11 | Ragland et al., 199329) | 27 | M | Coma | AcomA | Convexity | Hematoma evacuation | Death |
| 12 | Hatayama et al., 199411) | 55 | M | Semicoma | Distal ACA | Interhemispheric and convexity | Hematoma evacuation and clipping | Good |
| 13 | Hatayama et al., 199411) | 66 | F | Semicoma | Distal ACA | Interhemispheric, convexity, and tentorium | Hematoma evacuation and clipping | Disabled |
| 14 | Ishibashi et al., 199715) | 54 | F | Headache | PcomA | Tentorium and convexity | Hematoma evacuation and clipping | Good |
| 15 | Satoh et al., 199931) | 58 | F | Semicoma | PcomA | Convexity | Hematoma evacuation and clipping | Good |
| 16 | Satoh et al., 199931) | 25 | F | Headache | PcomA | Convexity | Hematoma evacuation and clipping | Good |
| 17 | Satoh et al., 199931) | 22 | F | Coma | PcomA | Convexity | Hematoma evacuation and clipping | Good |
| 18 | Huang et al., 199913) | 61 | F | Headache | MCA | Tentorium and convexity | Clipping | Good |
| 19 | Nonaka et al., 200025) | 52 | F | Coma | PcomA | Tentorium and convexity | Hematoma evacuation and clipping | Good |
| 20 | Ishikawa et al., 200016) | 62 | M | Headache, ptosis | PcomA | Tentorium and interhemispheric | Clipping | Good |
| 21 | Inamasu et al., 200214) | 28 | F | Coma | PcomA | Convexity | Hematoma evacuation | Death |
| 22 | Araki et al., 20021) | 55 | F | Headache, ptosis, semicoma | PcomA | Convexity | Hematoma evacuation and clipping | Good |
| 23 | Nozar et al., 200226) | 56 | M | Headache, drowsiness | AcomA | Convexity | Hematoma evacuation | Death |
| 24 | Nozar et al., 200226) | 28 | M | Headache | PcomA | Convexity | Hematoma evacuation and clipping | Good |
| 25 | Nozar et al., 200226) | 39 | F | Headache | PcomA | Convexity | Coiling | Good |
| 26 | Nozar et al., 200226) | 46 | M | Coma | MCA | Convexity | Hematoma evacuation and clipping | Death |
| 27 | Blake et al., 20032) | 35 | F | Coma | PcomA | Convexity | None | Death |
| 28 | Katsuno et al., 200317) | 63 | F | Headache, nausea, dizziness | Distal ACA | Interhemispheric and convexity | Hematoma evacuation and clipping | Good |
| 29 | Krishnaney et al., 200421) | 42 | F | Headache, photophobia | AcomA | Tentorium and convexity | Hematoma evacuation and clipping | Good |
| 30 | Koerbel et al., 200519) | 62 | F | Headache, semicoma | Bifurcation of ICA | Convexity | Hematoma evacuation and coiling | Good |
| 31 | Triantafyllopoulou et al., 200636) | 65 | F | Headache, nausea, vomiting, ptosis | ICA | Convexity and cavernous sinus | Hematoma evacuation | Comatose |
| 32 | Gilad et al., 20078) | 47 | M | Nausea, vomiting | AcomA | Sella, migrating to spinal canal | Coiling | Good |
| 33 | Kocak et al., 200918) | 47 | F | Not described | AcomA | Not described | Clipping | Good |
| 34 | Kurabe et al., 201022) | 75 | M | Headache, vomiting | MCA | Anterior fossa | Hematoma evacuation and resection | Not described |
| 35 | Field and Heran, 20105) | 33 | M | Headache, Terson syndrome | MCA | Convexity | Not described | Not described |
| 36 | Weil et al., 201038) | 51 | F | Coma | MCA | Convexity | Hematoma evacuation and coiling | Disabled |
| 37 | De Blasi et al., 20103) | 47 | F | Headache, stupor | PcomA | Convexity | Coiling | Good |
| 38 | De Blasi et al., 20103) | 60 | F | Headache, abducens palsy | MCA | Convexity | Clipping | Good |
| 39 | Takada et al., 201235) | 54 | M | Headache | AcomA | Tentorium and convexity | Clipping | Good |
| 40 | Mrfka, 201223) | 40 | F | Headahce, nausea, vomiting | PcomA | Convexity | Hematoma evacuation and coiling | Good |
| 41 | Present case | 42 | F | Headache | MCA | Tentorium and convexity | Hematoma evacuation and clipping | Good |




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download