Abstract
An intracranial saccular aneurysm is uncommonly diagnosed in a patient with closed head trauma. We herein present a patient with delayed rebleeding of a cerebral aneurysm misdiagnosed as traumatic subarachnoid hemorrhage (SAH). A 26-year-old female visited our emergency department because of headache after a motorcycle accident. Brain computed tomography (CT) showed a right-side dominant SAH in Sylvian fissure. Although traumatic SAH was strongly suggested because of the history of head trauma, we performed a CT angiogram to exclude any vascular abnormalities. The CT angiogram showed no vascular abnormality. She was discharged after conservative treatment. One day after discharge, she returned to the emergency department because of mental deterioration. Brain CT showed diffuse SAH, which was dominant in the right Sylvian fissure. The CT angiogram revealed a right middle cerebral artery bifurcation aneurysm. During operation, a non-traumatic true saccular aneurysm was found. The patient recovered fully after successful clipping of the aneurysm and was discharged without neurologic deficit.
Normal findings on a CT angiogram do not always exclude aneurysmal SAH. Follow-up vascular study should be considered in trauma patients who are highly suspicious of aneurysmal rupture.
Subarachnoid hemorrhage (SAH) is the most frequent intracranial lesion in patients with head trauma.6) Traumatic SAH is found in 15-40% of severe head injuries.5) Rupture of a cerebral aneurysm is an important differential diagnosis of traumatic SAH, especially in cases of a vague traumatic event without a witness. However, there are few reports on the relationship between head trauma and rupture of a cerebral aneurysm. We report a rare case of delayed rebleeding of a cerebral aneurysm misdiagnosed as traumatic SAH.
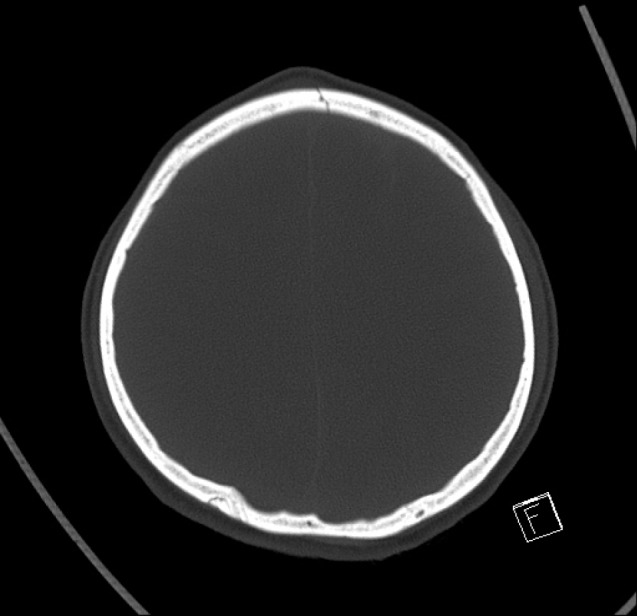
A 26-year-old female visited our emergency department because of headache after a motorcycle accident. On arrival in the emergency room, she was drowsy but there was no other neurologic deficit. Brain computed tomography (CT) showed focal SAH in the right Sylvian fissure (Fig. 1). The CT bone window setting revealed a left frontal bone fracture and a frontal scalp contusion (Fig. 2). Although definite evidence of trauma was present on CT, we performed a CT angiogram to exclude aneurysmal SAH. Because the CT angiogram showed no aneurysm or vascular abnormality (Fig. 3), traumatic SAH was diagnosed. She was treated conservatively for 10 days and discharged without neurologic deficit.
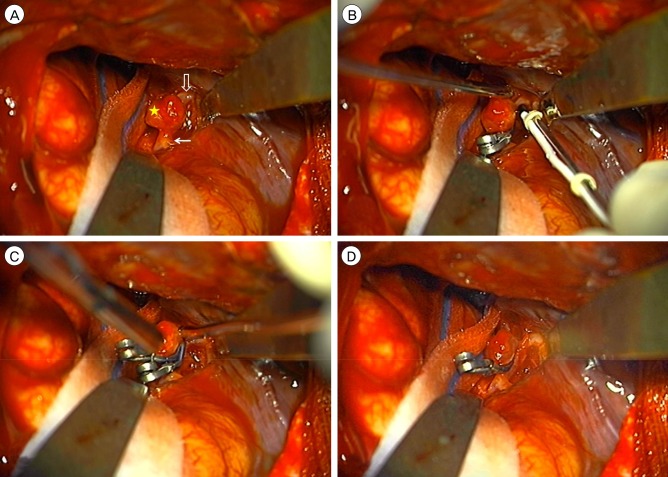
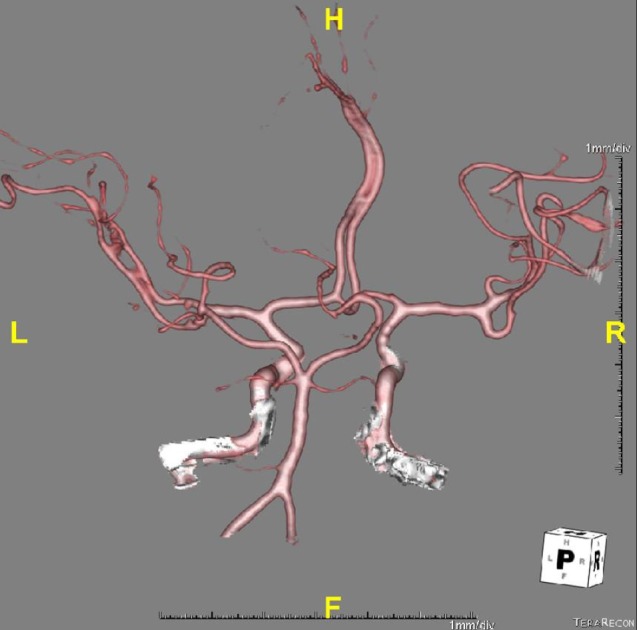
One day after discharge, she returned to the emergency department because of mental deterioration. She had a severe, bursting headache during a telephone call and lost consciousness. She was stuporous and CT showed a diffuse SAH, which was dominant in the right Sylvian fissure (Fig. 4). Due to a high degree of suspicion that a cerebral aneurysm had ruptured, a CT angiogram was immediately performed and demonstrated a 4 × 4 mm right middle cerebral artery (MCA) bifurcation aneurysm (Fig. 5). Based on the clinical history and radiologic findings, a traumatic aneurysm was initially suspected. The patient underwent pterional craniotomy and aneurysmal neck clipping (Fig. 6B, C, D). During operation, we tried several times of clip reposition in order to complete clipping. Despite these manipulations, there was no bleeding around the aneurysmal neck. Given this consideration, the aneurysm was considered true saccular aneurysm rather than pseudoaneurysm (Fig. 6A). Postoperatively, the patient recovered fully and was discharged without neurologic deficit after 21 days.
SAH associated with trauma may also rarely be associated with either traumatic or non-traumatic aneurysms, as a rupture of pre-existing aneurysm, or acute or late development of a traumatic aneurysm.9) Although 2.8-28% of patients with aneurysmal SAH experience head trauma prior to the hemorrhage,5) the relationship between head trauma and a pre-existing intracranial aneurysm is rarely discussed in the literature. The relationship of trauma to rupture of a cerebral aneurysm is controversial and a causal relationship can be difficult to ascertain.3) Some authors concluded that head injury itself is rarely the primary cause of the fatal rupture of a saccular aneurysm. However, a thin aneurysmal sac could be ruptured by being thrust against a bony structure such as the anterior or posterior clinoid process.3) Another report postulated that no relationship, or at best a very weak one, exists between closed head injury and the rupture of saccular aneurysms.7) Cummings et al.3) reported 5 (8%) of 60 patients with traumatic SAH harbored pre-existing intracranial saccular aneurysms. Of the 5 cases of aneurysm, the 3 patients who had SAH in the basal cisterns were highly suspicious for aneurysmal bleed, and the bleed may have precipitated the trauma. However, an unclear history from the patients made it very difficult to conclude what really happened. The 2 patients with a clear trauma history had highly non-suspicious CT. However, angiography did reveal a pre-existing unruptured aneurysm, which was confirmed intraoperatively. The relationships between head injury and pre-existing aneurysms have been summarized as follows: First, rupture of the aneurysm caused the trauma. Second, head impact caused rupture of the aneurysm. Third, an unruptured aneurysm was incidentally discovered during evaluation of head trauma.3)
In our case, the CT angiography on re-admission revealed a right MCA bifurcation aneurysm, which was not found on initial admission. Thus, a traumatic aneurysm was initially suspected based on the clinical history, presentation, and radiological findings. However, there was no evidence of traumatic intracranial aneurysm intraoperatively. The authors suspected that rupture of the aneurysm caused the head trauma. Initial negative findings on angiography may be attributed to thrombosis or focal vasospasm of the aneurysmal neck due to rupture of the aneurysm. The incidence of angiogram negative SAH is approximately 9-30% and 10% of repeat angiograms detect hidden aneurysms inducing SAH.1) The causes of angiogram negative SAH include thrombosed aneurysm, local vasospasm, parenchymal bleeding around an aneurysm, and high intracranial pressure.2) In this case, the authors suspected that thrombosis of the aneurysm occurred by hemostatic homeostasis after rupture to prevent further bleeding. Statistically 13-20% of giant aneurysms and 1-2% of non-giant aneurysms can be thrombosed, and the factors associated with thrombosis are a small aneurysmal neck, intraluminal thrombosis, and aneurysm age.2) The other possibility is focal vasospasm of the aneurysmal neck after rupture. SAH induces vasospasm of the parent artery or aneurysmal neck, so hemodynamic change can occur in the aneurysmal sac or neck. Lastly, the aneurysmal orifice can be temporarily occluded, and blood flow to the aneurysmal sac is blocked.2)8)
There is a well-known relationship between trauma and SAH.6) Eisenberg et al.4) reported that SAH was found in 39% of 753 patients with severe head trauma. Based on initial CT on admission, the hemorrhage induced by tearing of intracranial vessels, more frequently involves a few sulci of the cerebral convexity, and less often, the fissures and basal cisterns. The greatest accumulation of SAH occurs contralateral to the side of impact.3)5) The superficial parietal and temporal branches of the MCA are particularly vulnerable, and usually a sub-branch attached to the arachnoid proper is torn where the major branch passes over the crest of a convolution.10) SAH on the convexity may also occur by tearing of the superior cerebral veins where they enter the superior sagittal sinus.3) As mentioned above, traumatic SAH tends to localize in the sulci of the cerebral convexity, with greater accumulation contralateral to the side of impact. Therefore, aneurysmal SAH should be suspected when SAH involves the Sylvian fissure and basal cistern. In our case, focal SAH was found in the right Sylvian fissure, which was not contralateral to the side of impact. In addition, the location of SAH was almost identical between the initial admission and readmission brain CT. Thus, we concluded that SAH resulted from aneurysmal rupture.
During initial patient evaluation, neurosurgeons should maintain a high degree of suspicion when post-traumatic SAH involves the basal cisterns or Sylvian fissure. The work-up should proceed to definitively rule out an aneurysm in patients that present with a CT suspicious for aneurysm but negative for SAH.
References
1. Aarabi B. Management of traumatic aneurysms caused by high-velocity missile head wounds. Neurosurg Clin N Am. 1995; 10. 6(4):775–797. PMID: 8527918.

2. Choi YS, Kim DW, Jang SJ, Kang SD. Recanalization of completely thrombosed non-giant saccular aneurysm mimicking as de novo aneurysm. J Korean Neurosurg Soc. 2010; 10. 48(4):354–356. PMID: 21113364.
3. Cummings TJ, Johnson RR, Diaz FG, Michael DB. The relationship of blunt head trauma, subarachnoid hemorrhage, and rupture of pre-existing intracranial saccular aneurysms. Neurol Res. 2000; 3. 22(2):165–170. PMID: 10763504.

4. Eisenberg HM, Gary HE Jr, Aldrich EF, Saydjari C, Turner B, Foulkes MA, et al. Initial CT findings in 753 patients with severe head injury. A report from the NIH Traumatic Coma Data Bank. J Neurosurg. 1990; 11. 73(5):688–698. PMID: 2213158.
5. Hsieh CT, Lin EY, Tsai TH, Chiang YH, Ju DT. Delayed rupture of pre-existing cerebral aneurysm in a young patient with minor head trauma. J Clin Neurosci. 2007; 11. 14(11):1120–1122. PMID: 17954376.

6. Kakarieka A. Review on traumatic subarachnoid hemorrhage. Neurol Res. 1997; 6. 19(3):230–232. PMID: 9192371.

7. McCormick WF. The relationship of closed-head trauma to rupture of saccular intracranial aneurysms. Am J Forensic Med Pathol. 1980; 9. 1(3):223–226. PMID: 6453526.

8. Ohta H, Sakai N, Nagata I, Sakai H, Shindo A, Kikuchi H. Spontaneous total thrombosis of distal superior cerebellar artery aneurysm. Acta Neurochir (Wien). 2001; 8. 143(8):837–842. discussion 842-3. PMID: 11678406.

9. Suzuki H, Muramatsu M, Shimizu T, Kusano I, Kojima T. Late detection of supraclinoid carotid artery aneurysm after traumatic subarachnoid hemorrhage and occlusion of the ipsilateral cervical internal carotid artery. Stroke. 2001; 9. 32(9):2203–2205. PMID: 11546918.

10. Tatsuno Y, Lindenberg R. Basal subarachnoid hematomas as sole intracranial traumatic lesions. Arch Pathol. 1974; 4. 97(4):211–215. PMID: 4814705.
Fig. 1
Brain CT on initial admission shows focal SAH in the right Sylvian fissure. CT = computed tomography; SAH = subarachnoid hemorrhage.
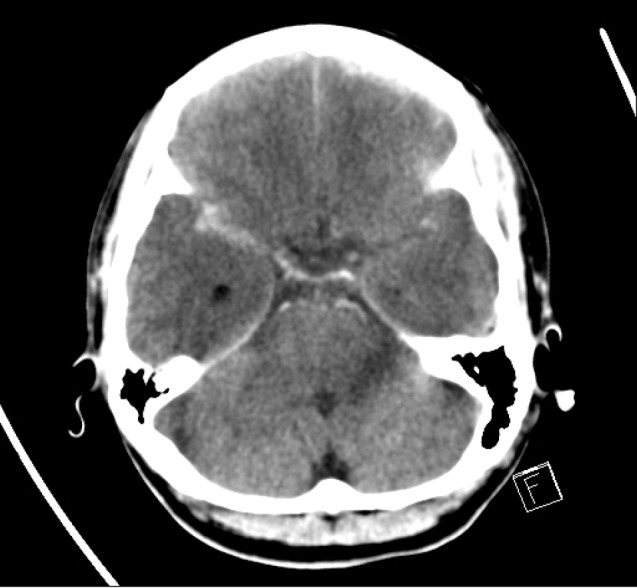
Fig. 4
Brain CT on readmission demonstrates SAH which dominant in the right Sylvian fissure. CT = computed tomography; SAH = subarachnoid hemorrhage.
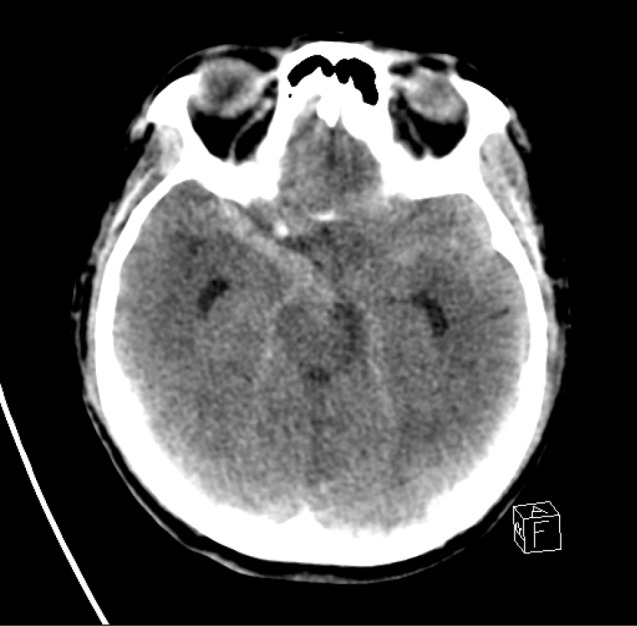
Fig. 5
CT angiogram on readmission shows a 4 × 4 mm right MCA bifurcation aneurysm (white arrow). CT = computed tomography; MCA = middle cerebral artery.
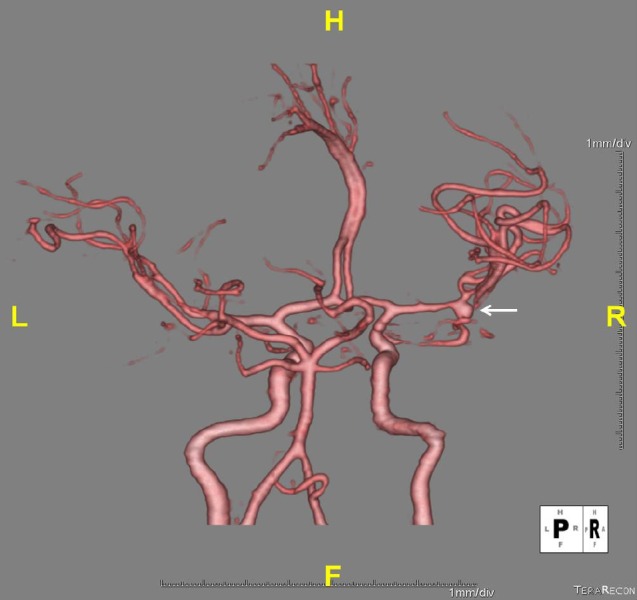
Fig. 6
Intraoperative photographs. (A) Aneurysm with narrow neck (star) located at right MCA bifurcation. Arrow: frontal branch of MCA, Open arrow: temporal branch of MCA. (B) After aneurysmal clipping, transcranial Doppler reflected violation of the MCA by the clip. (C) Another clip was applied above the first clip. (D) Frontal and temporal branch of MCA are patent after removal of the first clip. MCA = middle cerebral artery.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download