Abstract
Objective
The purpose of this study was to report the authors' preliminary experience using the Amplatzer Vascular Plug (AVP) (St. Jude Medical, Plymouth, MN, USA) for parent artery occlusion of the internal carotid artery (ICA) or vertebral artery (VA).
Materials and Methods
Between September 2008 and December 2015, we performed 52 therapeutic parent artery occlusions (PAOs) by an endovascular technique. Among them, 10 patients underwent PAO of the carotid or vertebral arteries using AVPs. Clinical and radiographic data of these patients were retrospectively reviewed.
Results
The devices were used for VA dissection that presented with subarachnoid hemorrhage (SAH) in five patients, traumatic arteriovenous fistula (AVF) in two patients, spontaneous AVF in one patient, recurrence of carotid-cavernous fistula (CCF) in one patient, and symptomatic unruptured giant ICA aneurysm in one patient. The devices were used in conjunction with detachable and/or pushable coils and in the extracranial segments of the ICA or VA. Complete occlusion of the parent artery was achieved in all patients. There was one intra-procedural rupture of the VA dissection during coiling prior to using the device.
Although reconstruction techniques using stents, such as flow-diverters, have come to the forefront in neuroendovascular fields, therapeutic parent artery occlusion (PAO) is still necessary in the treatment of fusiform giant cerebral aneurysms, arterial dissection, direct carotid-cavernous fistula (CCF), or high-flow head and neck arteriovenous fistula (AVF). Historically, detachable balloons were used for these purposes; however, after the balloon occlusion device was withdrawn from the market, coil embolization became the most common method for PAO.
The Amplatzer Vascular Plug (AVP) (St. Jude Medical, Plymouth, MN, USA) is a self-expanding nitinol mesh cage that was approved by the United States Food and Drug Administration for clinical use in 2004, for peripheral vascular embolizations. This device can serve as an excellent alternative to coils or detachable balloons in the embolization of medium to large vessels with high flow. The AVP family has developed and evolved from a single device to a group of 4 models (types 1 to 4) that can be used for various types of anatomy, hemodynamics, and lesion entities. All models contain two basic components: a vascular plug and a delivery wire. The plugs have radiopaque marker bands at both ends and a stainless-steel screw on one of the marker bands attaches to a delivery cable. Once the position of a deployed device is satisfactory, the device can easily be released by rotating the cable counterclockwise to complete implantation. These days, the device has been successfully and extensively used in a wide range of therapeutic applications, even in neurovascular diseases.14)
This retrospective study was approved by the institutional review board and the requirement for informed consent was waived. Between September 2008 and December 2015, we performed 52 therapeutic PAO surgeries by an endovascular technique. Among these, 10 patients underwent PAO of the ICA or VA using vascular plugs. The AVP has been used in the medium to large arteries (proximal ICA and VA) where simple coil occlusion wan not enough to occlude the artery due to high flow. Clinical and radiographic data of the patients, such as age, sex, initial presentation signs, laterality (right or left), location of the device deployed, number of devices used, type of the device, size of the device, number of detachable coils used, number of pushable coils used, procedure-related complications, angiographic results, and clinical outcomes, were retrospectively reviewed and described.
All operations were performed under general anesthesia. A 6-Fr guiding catheter was positioned in the ICA and a 5-Fr or 6-Fr guiding catheter in the VA. Coil embolization was performed via a microcatheter with an inner diameter (ID) of 0.021 inches in cases using pushable coils. Similar to an intracranial self-expanding stent, deployment of the AVP was performed by unsheathing the guiding catheter gently when it was correctly positioned. If the positioning of the device was suboptimal, it was re-sheathed and redeployed. The device was detached through counterclockwise rotation of the pusher wire using a torque device. Heparin was not injected intravenously or subcutaneously, but was instead mixed into the saline slushes during the procedure. Therefore, the activated clotting time (ACT) was not checked during the procedure. In addition, antiplatelet agents were not used.
The final angiographic results were evaluated by two independent investigators and categorized as complete occlusion or incomplete occlusion of the parent arteries. There was no follow-up angiography at the time of analysis because we planned to perform follow-up angiography when clinical symptoms or signs developed. There was no recurrence of clinical symptoms and signs. Clinical outcomes were assessed based on the modified Rankin Scale (mRS) in which a mRS score of 0 was completely independent and a mRS score of 6 was indicative of death.
Table 1 shows clinical and radiographic characteristics of the patients. The device was used in addition to detachable and/or pushable coils in all 10 cases: five cases with intracranial VA dissection presented with subarachnoid hemorrhage (SAH); two cases with traumatic AVF; one case with spontaneous AVF; one case with recurrence of CCF; and one case with symptomatic unruptured giant ICA aneurysm. Mean age of the 10 patients was 55.6 years. A type 1 device was used only in the first case, type 2 devices were used in the next 6 cases, and type 4 devices were used most recently in 3 cases. Technical success rate was 100% and there were no cases of suboptimal device positioning in this study. There was one intraprocedural rupture of the VA dissection during coiling prior to using the device (case 4). Otherwise, there were no procedure-related complications related to use of the device. At discharge, mRS was 0 in six patients, 1 in two patients, 5 in one patient, and 6 (death due to an initial insert of SAH) in one patient.
A 62-year-old female suffered from right-side CCF with complete steal (Fig. 1A) and was treated by ICA occlusion with coil embolization. Immediate postoperative right ICA angiography showed that complete obliteration of the right ICA was achieved. In addition, the collaterals from the anterior and posterior communicating artery supplied the right hemisphere (Fig. 1B; white circles indicate coils packed in the cavernous sinus and the right ICA). However, recanalization of the right ICA and the CCF caused her to return to the institution (Fig. 1C). Retreatment by right ICA occlusion was performed with several additional coils and a type 2 AVP (Fig. 1D). Finally, complete occlusion of the right ICA was achieved.
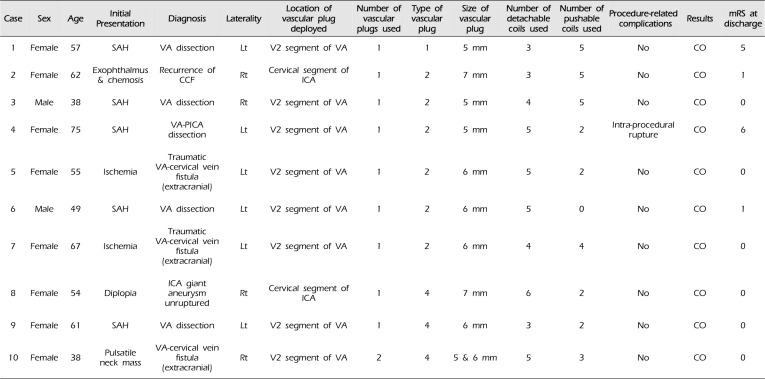
A 38-year-old female with neurofibromatosis type I suffered from a large pulsatile mass on the left side of her neck. Her neck CT and digital subtraction cerebral angiography (DSA) revealed a very high-flow AVF from the V2 segment of the left VA to the cervical venous plexus with a large pseudoaneurysm or venous pouch just distal to the fistula (Fig. 2A). Because of the high-flow shunt via either antegrade or retrograde flow, it seemed impossible to achieve parent artery occlusion with coiling only. Thus, short-segment trapping of the left VA was planned and two AVPs (type 4) were deployed distal and proximal to the fistula with coiling between the AVPs (Fig. 2B). As the diameter of the left VA was approximately 3.6 mm, we deployed a 5-mm AVP distally and a 6-mm AVP proximally. Finally, the AVF was occluded completely (Fig. 2C, D).
In the present study, we experienced positive outcomes with AVPs indicating that these devices could be used for therapeutic PAO in the extracranial segments of the ICA or VA. These devices have a low risk of distal migration because they are anchored to the vessel wall by radial force. It was recommended that oversizing the device by 30-50% with respect to the diameter of the parent artery would make the device more stable. Previously, detachable balloons were available to provide a fast method of PAO; however, this technique carried the risk of unintentional detachment or early balloon deflation, and distal migration of the balloon could lead to recurrence of the disease and/or distal thromboembolic complications. In addition, the AVP device has multiple layers of cross-sectional nitinol mesh to occlude flow and showed a rapid occlusion time, which would prevent the potential complications of thrombus formation within the parent artery and/or distal embolization into the intracranial circulation. With the evolution of endovascular techniques and an innovative endovascular approach, the management of high-flow vascular lesions in the head and neck might be achieved rapidly and safely. Moreover, there was a low recurrence rate after successful PAO with the AVP.
As mentioned above, the AVP is a self-expanding nitinol mesh cage and has been successfully used in a wide range of therapeutic applications.14) However, relatively few reports about the use of these devices in neuroendovascular fields have been published to date.6)8)9)10)11) The AVP family has evolved from a single device to a group of 4 models (types 1 to 4). Type 1 is a large cylindrical mesh cage and is generally referred to as the initial model of the AVP family. This type is appropriate for short landing zones and has high radial force that secures the device within the parent vessel. Type 2 is preferred if rapid vessel occlusion is required and is better for minimizing migration and recanalization compared to type 1. Almost all previous reports about the use of AVP in neuroendovascular fields involved type 1 and type 2 AVPs. Type 3 offers a rapid occlusion capability and fits elliptical-shaped vascular structures. It is better at enhancing stability in high-flow vessels than the previous types. However, type 3 is not appropriate for use in neuroendovascular fields because of its shape and radial force. Type 4 is the most effective type if the target vessels are small and access to the target segments is difficult as it can be delivered using a 0.038-inch diagnostic catheter without a delivery catheter. Type 4 seems to be the most appropriate type of AVP for use in neuroendovascular fields. In the present series, the AVP type 4 did not move and effectively occluded the parent artery proximally as well as distally while treating a very high-flow AVF (case 10) that migrated coils to a distal venous pouch or a pseudoaneurysm. As mentioned above, migration is a rare complication of AVP because it is self-expanding and has sufficient radial force on the vessel wall to minimize movement.13)
There are some limitations of our study. One limitation is its retrospective design with a very small number of included patients. Furthermore, there are no control groups for comparison of the effects of the AVP with other currently used methods of PAO. Another limitation is that there are no follow-up angiographic results to show the long-term efficacy of the device. However, spontaneous recanalization of the AVP after successful PAO is very rare, with only 5 reports of recurrence among more than 1,200 AVP placements described in the literature.1) Regarding pulmonary AVMs, 20 published papers have described a total of 340 PAOs using AVPs, with recurrence occurring in approximately 1%.2)3)4)12) In comparison, coil embolization is associated with a recurrence rate of 8-15%.5)7) In addition, the AVP procedure should be considered a technical failure unless complete PAO has been demonstrated. If necessary, additional embolic material, such as coils or additional AVPs, can be used as adjuncts to ensure complete occlusion.
References
1. Dorenberg EJ, Hafsahl G, Andersen R, Krohg-Sørensen K. Recurrent rupture of a hypogastric aneurysm caused by spontaneous recanalization of an Amplatzer vascular plug. J Vasc Interv Radiol. 2006; 6. 17(6):1037–1041. PMID: 16778239.

2. Fidelman N, Gordon RL, Bloom AI, LaBerge JM, Kerlan RK Jr. Reperfusion of pulmonary arteriovenous malformations after successful embolotherapy with vascular plugs. J Vasc Interv Radiol. 2008; 8. 19(8):1246–1250. PMID: 18656022.

3. Hart JL, Aldin Z, Braude P, Shovlin CL, Jackson J. Embolization of pulmonary arteriovenous malformations using the Amplatzer vascular plug: successful treatment of 69 consecutive patients. Eur Radiol. 2010; 11. 20(11):2663–2670. PMID: 20574633.

4. Letourneau-Guillon L, Faughnan ME, Soulez G, Giroux MF, Oliva VL, Boucher LM, et al. Therasse E. Embolization of pulmonary arteriovenous malformations with Amplatzer vascular plugs: safety and midterm effectiveness. J Vasc Interv Radiol. 2010; 5. 21(5):649–656. PMID: 20346701.
5. Mager JJ, Overtoom TT, Blauw H, Lammers JW, Westermann CJ. Embolotherapy of pulmonary arteriovenous malformations: long-term results in 112 patients. J Vasc Interv Radiol. 2004; 5. 15(5):451–456. PMID: 15126654.

6. Mihlon F, Agrawal A, Nimjee SM, Ferrell A, Zomorodi AR, Smith TP, et al. Enhanced, rapid occlusion of carotid and vertebral arteries using the AMPLATZER Vascular Plug II device: the Duke Cerebrovascular Center experience in 8 patients with 22 AMPLATZER Vascular Plug II devices. World Neurosurg. 2015; 1. 83(1):62–68. PMID: 23920294.

7. Milic A, Chan RP, Cohen JH, Faughnan ME. Reperfusion of pulmonary arteriovenous malformations after embolotherapy. J Vasc Interv Radiol. 2005; 12. 16(12):1675–1683. PMID: 16371535.

8. Ong CK, Lam DV, Ong MT, Power MA, Parkinson RJ, Wenderoth JD. Neuroapplication of Amplatzer vascular plug for therapeutic sacrifice of major craniocerebral arteries: an initial clinical experience. Ann Acad Med Singapore. 2009; 9. 38(9):763–768. PMID: 19816634.
9. Ross IB, Bucius R. The vascular plug: a new device for parent artery occusion. AJNR Am J Neuroradiol. 2007; 2. 28(2):385–386. PMID: 17297018.
10. Scott DA, Keston P, White P, Sellar R. Vascular plug for ICA occlusion in cavernous carotid aneurysms: technical note. Neuroradiology. 2008; 9. 50(9):795–798. PMID: 18542939.

11. Shankar JJ, Maloney WJ, Vandorpe R. Amplatzer vascular plug for occlusion of parent artery in carotid blowout with active extravasation. Interv Neuroradiol. 2011; 6. 17(2):224–227. PMID: 21696663.

12. Tapping CR, Ettles DF, Robinson GJ. Long-term follow-up of treatment of pulmonary arteriovenous malformations with Amplatzer vascular plug and Amplatzer vascular plug II devices. J Vasc Interv Radiol. 2011; 12. 22(12):1740–1746. PMID: 22115581.

13. Tuite DJ, Kessel DO, Nicholson AA, Patel JV, McPherson SJ, Shaw DR. Initial clinical experience using the Amplatzer vascular plug. Cardiovasc Intervent Radiol. 2007; Jul-Aug. 30(4):650–654. PMID: 17497066.

14. Wang W, Li H, Tam MD, Zhou D, Wang DX, Spain J. The Amplatzer vascular plug: a review of the device and its clinical applications. Cardiovasc Intervent Radiol. 2012; 8. 35(4):725–740. PMID: 22526108.

Fig. 1
(A) A 62-year-old female suffered from right side carotid-cavernous fistula (CCF) with complete steal and was treated by internal carotid artery (ICA) occlusion with coil embolization. (B) After right ICA occlusion, the collaterals from the anterior and posterior communicating artery supplied the right hemisphere. White circles indicate coils packed in the cavernous sinus and the right ICA. (C) Recanalization of the right ICA and the CCF occurred. (D) Retreatment by right ICA occlusion was performed with several additional coils and an Amplatzer Vascular Plug type 2.
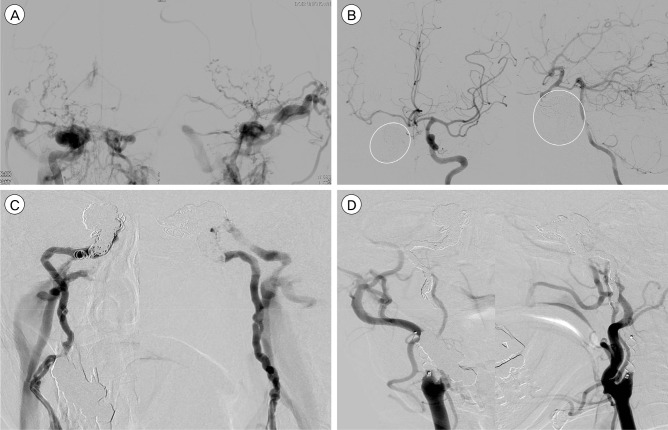
Fig. 2
A 38-year-old female with neurofibromatosis type I suffered from a large pulsatile mass on the left side of her neck. (A) Digital subtraction cerebral angiography revealed a very high-flow AVF from the V2 segment of the left VA to the cervical venous plexus with a large pseudoaneurysm or venous pouch just distal to the fistula. (B) Short-segment trapping of the left VA was performed. Two AVPs (type 4; white circles) were deployed distal and proximal to the fistula with coiling between the AVPs. (C, D) Final left VA angiography (C) and right VA angiography (D) revealed complete occlusion of the fistula (white circles indicate the AVPs and white arrow indicates the occlusion of retrograde flow). AVF = arteriovenous fistula; VA = vertebral artery.

Table 1
Clinical and radiographic characteristics of the patients




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download