Abstract
Endovascular coil embolization using a balloon- or stent-assisted technique for the treatment of wide-necked posterior communicating artery (PcomA) aneurysms is well established. However, complete aneurysm occlusion with preservation of the PcomA can be difficult in case of wide-neck aneurysms with a PcomA incorporation. We present two cases of stent-assisted coil embolization using a retrograde approach through the posterior circulation for wide-neck or branch-incorporated PcomA aneurysms. Retrograde stenting was successful without periprocedural complications. These aneurysms were completely occluded. The patency of the PcomA was maintained in all cases.
Endovascular coil embolization of posterior communicating artery (PcomA) aneurysm is relatively easier than other anterior circulation intracranial artery aneurysms in an aspect of simple microcatheter access. However, coiling of wide-neck or branch-incorporated PcomA aneurysm is challenging to prevent coil protrusion and preserve blood flow of parent or PcomA vessel. Moreover, in case of acute-angled PcomA from internal carotid artery (ICA), it requires a novel technical method for stent-assisted coil embolization. We present two cases of wide-neck or branch-incorporated PcomA aneurysms, which were treated by retrograde stent-assisted coil embolization through ipsilateral posterior cerebral artery (PCA).
A 33-year-old man was admitted to our hospital following severe headache that lasted 8 hours. His mental status was alert, and the neurologic examination was unremarkable. Brain computed tomography (CT) demonstrated a Fisher grade 2 and Hunt-Hess grade 2 subarachnoid hemorrhage. A cerebral angiography was obtained immediately and showed bilobed 1.6 × 3.5 mm sized wide-neck aneurysm at left PcomA (Fig. 1A). Stent-assisted coil embolization for ruptured aneurysm at acute period is not recommended because of thromboembolic or hemorrhagic complications due to antiplatelet agents. Nevertheless, this patient was treated by stent-assisted coil embolization by request of patient fearing surgical invasiveness. The procedure was performed under-general anesthesia. Loading dose of clopidogrel (300 mg) was took via Levin tube and a bolus of 1,000 IU of heparin was administered after femoral arterial puncture and was added by each hour. Procedural steps were as followings : (1) Two guiding systems with 6 French Envoy MPD guiding catheters (Codman & Shurtleff Inc, Raynham, MA, USA) were placed at the level of the V2 segment of left vertebral artery (VA) and ascending cervical segment of left ICA by bilateral femoral puncture; (2) Placement of a stent delivery microcatheter (Prowler Select Plus, Codman Neurovascular, Miami Lakes, FL, USA) into left M1 of middle cerebral artery (MCA) via ipsilateral P1 by retrograde approach (Fig. 1B); (3) Access of another microcatheter (Prowler Select Plus, Codman Neurovascular, Miami Lakes, FL, USA) for coil delivery to aneurysmal sac via ipsilateral ICA; (4) Deployment of self-expandable stent (Enterprise, 4.5 × 28 mm, Codman Neurovascular, Miami Lakes, FL, USA) from M1 to P1; (5) Coil packing was performed with four detachable coils with stent-jail technique. There was no contrast filling in aneurysmal sac or decrease of blood flow from parent artery after coiling (Fig. 1C). On follow-up at 18 months, aneurysmal sac was occluded totally in the cerebral angiography (Fig. 1D).
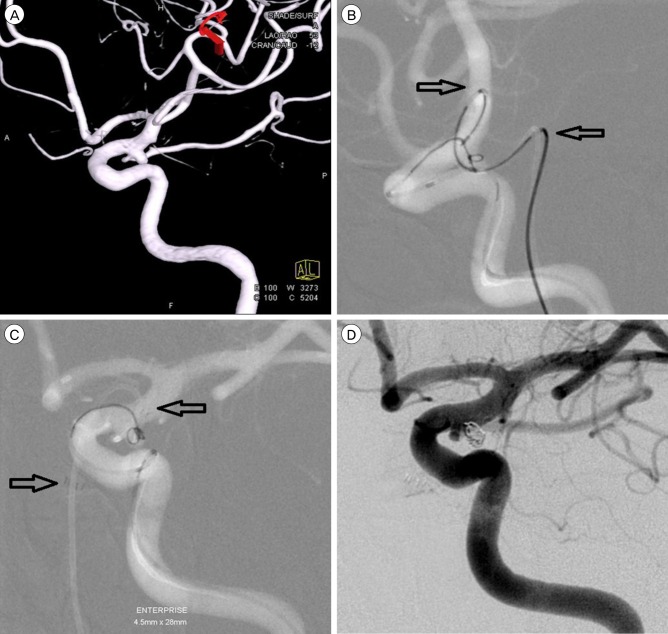
A 51-year-old female presented mild dizziness for several months. She has no underlying disease. A cerebral angiography showed wide-neck unruptured aneurysm at left PcomA. The aneurysm was posteriorly directed and its size was 2.6 × 2.3 mm. The PcomA was incorporated at the aneurysmal neck broadly (Fig. 2A). The patient had been received 75mg of clopidogrel and 100mg aspirin for 7 days before the endovascular procedure. The endovascular procedure was performed under-general anesthesia. Procedural steps were similar as above : (1) Placement of two guiding systems (a 6 French 90 cm Envoy MPD guiding catheter at left ICA and a 5 French 100 cm Envoy MPD at left VA [Codman & Shurtleff Inc., Raynham, MA, USA]); (2) Access of microcatheter (Prowler Select Plus, Codman Neurovascular, Miami Lakes, FL, USA) into aneurysmal sac; (3) Placement of microcatheter (Prowler Select Plus, Codman Neurovascular, Miami Lakes, FL, USA) via left P1 and PcomA (Fig. 2B); (4) Before the deployment of stent, one coil loop was inserted into the aneurysmal sac; (5) Self-expandable stent (Enterprise, 4.5 × 28 mm, Codman Neurovascular, Miami Lakes, FL, USA) was deployed anchoring coil mass (Fig. 2C); (6) Aneurysmal sac was completely packed with five detachable coils; (7) There was no contrast filling in aneurysmal sac and the blood flow of PcomA was intact (Fig. 2D).
PcomA aneurysms are common intracranial aneurysms representing 50% of all ICA aneurysms and 25% of all intracranial aneurysms.5) Though PcomA aneurysms have several anatomic variations in the extent of involvement of the PcomA, most common type is the PcomA partially-incorporation at the neck of aneurysm. However, if incorporating aneurysm has a wide neck or PcomA was acutely angled from ICA, the endovascular treatment using balloon- or stent-assisted technique through usual anterograde approach would be difficult. Sometimes, stent placement from the ICA to acute-angled PcomA can cause kinking or narrowing of the stent.2) Thus, retrograde approach through dominant VA can be considered as an alternative route to aneurysmal sac.
Retrograde stenting has several advantages: (1) protection of coil protrusion (2) horizontal stent placement prevents kinking or narrowing (ovalization) in case of acute-angled PcomA not to make the risk of stent-induced flow disturbance.1)
To our knowledge, retrograde technique was introduced by Gurian and his colleagues in 1995 for the first time.4) In their case report, retrograde approach was used to occlude residual lumen of right distal VA aneurysm, which was previously treated by endovascular proximal balloon occlusion. In their first attempt, microcatheter navigation through the left VA and over the vertebrobasilar junction was not possible because of the acute angle of VA-VA. Finally, retrograde approach via right ICA-PcomA-P1-BA and coil embolization was successfully performed using a hydrophilic coating microcatheter (FasTracker-10; Target Therapeutics). Moret et al.8) reported 12 cases of retrograde approach using balloon remodeling technique for endovascular treatment of cerebral aneurysms. In their study, the locations of aneurysms were basilar bifurcation in five cases, PcomA in two, ICA bifurcation in two, superior cerebellar artery in two and posterior inferior cerebellar artery in one. In two patients, the retrograde catheterization was failed. Despite small number of cases, this study suggested an efficacy of retrograde approach.
For successful endovascular treatment by this technique, there were some considerable points. First, the diameter of arteries should be considered. In general, stent-assisted coil embolization in small vessels can cause peri-procedural thrombus or dissection of vessel. However, several previous series have reported that Enterprise stent can be feasible in parent arteries below a 2.0-mm diameter.3)7)10) In our cases, we were able to pass the microcatheter with stent system through ipsilateral PCA easily. And none of the deployed stent developed occlusion of the parent artery or other thromboembolic complication. Second, Enterprise stent is a closed-cell type stent and its conformability was lower comparing with other type of intracranial stents. However, this stent system have been recorded good results in several studies.6)9)11)12) In our case 1, a follow up angiography at 18 months presented straightening of stent due to its low conformability (Fig. 1D). But, horizontal straightening of stent especially on wide-necked aneurysm is not always pitiful in that it makes full coverage of the aneurysm neck.
This retrograde approach is not applicable in all PcomA aneurysm with a difficult configuration. Anatomic conditions of the vessels should be sufficient for microcatheter to pass through. So, this approach is not a first line treatment of a wide-neck or branch-incorporated PcomA aneurysm. But, if usual anterograde approach is not possible to deploy stent or pack with coil, this approach could be a good alternative method. But, further studies with a large population are needed to establish its efficacy and safety.
References
1. Cho YD, Kang HS, Lee WJ, Kim KM, Kim JE, Han MH. Stent-assisted coil embolization of wide-necked posterior inferior cerebellar artery aneurysms. Neuroradiology. 2013; 7. 55(7):877–882. PMID: 23568700.

2. Cho YD, Lee WJ, Kim KM, Kang HS, Kim JE, Han MH. Stent-assisted coil embolization of posterior communicating artery aneurysms. AJNR Am J Neuroradiol. 2013; Nov-Dec. 34(11):2171–2176. PMID: 23660292.

3. Chung J, Kim B, Lee D, Kim TH, Shin YS. Vertebral artery occlusion with vertebral artery-to-posterior inferior cerebellar artery stenting for preservation of the PICA in treating ruptured vertebral artery dissection. Acta Neurochir (Wien). 2010; 9. 152(9):1489–1492. PMID: 20593207.

4. Gurian JH, Viñuela F, Gobin YP, Waston VE, Duckwiler GR, Gulielmi G. Aneurysm rupture after parent vessel sacrifice: treatment with Guglielmi detachable coil embolization via retrograde catheterization: case report. Neurosurgery. 1995; 12. 37(6):1216–1220. discussion 1220-1. PMID: 8584166.
5. He W, Gandhi CD, Quinn J, Karimi R, Prestigiacomo CJ. True aneurysms of the posterior communicating artery: a systematic review and meta-analysis of individual patient data. World Neurosurg. 2011; 1. 75(1):64–72. discussion 49. PMID: 21492665.

6. Higashida RT, Halbach VV, Dowd CF, Juravsky L, Meagher S. Initial clinical experience with a new self-expanding nitinol stent for the treatment of intracranial cerebral aneurysms: the Cordis Enterprise stent. AJNR Am J Neuroradiol. 2005; 8. 26(7):1751–1756. PMID: 16091525.
7. Kim MJ, Chung J, Kim SL, Roh HG, Kwon BJ, Kim BS, et al. Stenting from the vertebral artery to the posterior inferior cerebellar artery. AJNR Am J Neuroradiol. 2012; 2. 33(2):348–352. PMID: 22051805.

8. Moret J, Ross IB, Weill A, Piotin M. The retrograde approach: a consideration for the endovascular treatment of aneurysms. AJNR Am J Neuroradiol. 2000; 2. 21(2):262–268. PMID: 10696006.
9. Peluso JP, van Rooij WJ, Sluzewski M, Beute GN. A new self-expandable nitinol stent for the treatment of wide-neck aneurysms: initial clinical experience. AJNR Am J Neuroradiol. 2008; 8. 29(7):1405–1408. PMID: 18436611.

10. Roh HG, Chun YI, Choi JW, Cho J, Moon WJ, Solander S. Retrograde stent placement for coil embolization of a wide-necked posterior inferior cerebellar artery aneurysm. Korean J Radiol. 2012; Jul-Aug. 13(4):510–514. PMID: 22778576.

11. Siddiqui MA, J Bhattacharya J, Lindsay KW, Jenkins S. Horizontal stent-assisted coil embolisation of wide-necked intracranial aneurysms with the Enterprise stent--a case series with early angiographic follow-up. Neuroradiology. 2009; 6. 51(6):411–418. PMID: 19277620.

12. Weber W, Bendszus M, Kis B, Boulanger T, Solymosi L, Kühne D. A new self-expanding nitinol stent (Enterprise) for the treatment of wide-necked intracranial aneurysms: initial clinical and angiographic results in 31 aneurysms. Neuroradiology. 2007; 7. 49(7):555–561. PMID: 17476494.

Fig. 1
(A) A cerebral angiography revealed a wide-neck aneurysm at left posterior communicating artery. (circle) (B) Microcatheter for stenting was positioned to left M1 via PcomA. (C) Final angiography showed a complete occlusion of aneurysmal sac with four detachable coils and retrograde stenting. (Asterisk : ICA, Yellow arrow : Posterior communicating artery, White arrow : P1 of posterior cerebral artery, Two arrowheads : Both ends of stent) (D) A follow-up angiography at 18 months showed no evidence of recurrent of aneurysmal sac. Straight of stenting was observed. (two arrowheads are the both ends of stent). ICA = internal carotid artery.
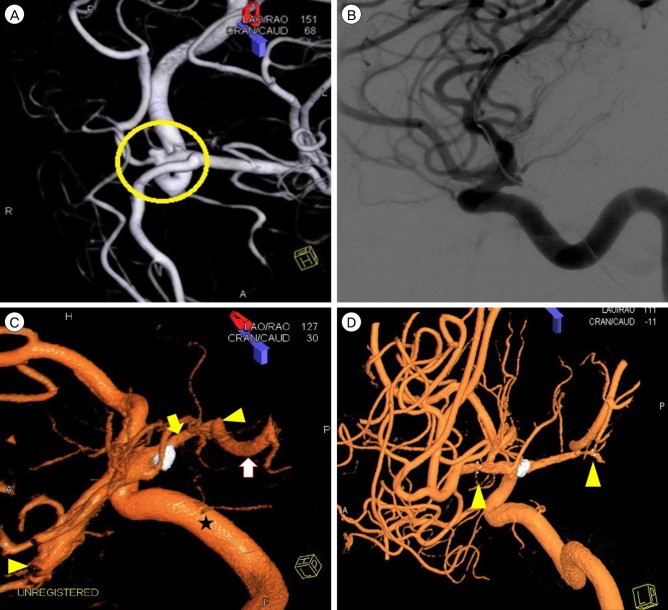
Fig. 2
(A) Cerebral angiography demonstrated a branch-incorporated aneurysm at left posterior communicating artery. (B) The stent delivery microcatheter was placed acrossing the aneurysmal neck via P1-PcomA. (arrows) (C) Retrograde stenting was performed from terminal ICA to PcomA. (two arrows are the both ends of stent) (D) Final angiography showed a complete occlusion of the aneurysm maintaining the patency of PcomA flow. PcomA = posterior communicating artery; ICA = internal carotid artery.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download