Abstract
Objective
Preoperative endovascular embolization of intracranial tumors is performed to mitigate anticipated intraoperative blood loss. Although the usage of a wide array of embolic agents, particularly polyvinyl alcohol (PVA), has been described for a variety of tumors, literature detailing the efficacy, safety and complication rates for the usage of Onyx is relatively sparse.
Materials and Methods
We reviewed our single institutional experience with pre-surgical Onyx embolization of extra-axial tumors to evaluate its efficacy and safety and highlight nuances of individualized cases.
Results
Five patients underwent pre-surgical Onyx embolization of large or giant extra-axial tumors within 24 hours of surgical resection. Four patients harbored falcine or convexity meningiomas (grade I in 2 patients, grade II in 1 patient and grade III in one patient), and one patient had a grade II hemangiopericytoma. Embolization proceeded uneventfully in all cases and there were no complications.
Meningiomas are typically treated through surgical resection if large and with symptoms related to mass effect. However, these tumors are often hypervascular and surgical resection can lead to significant blood loss if en bloc resection is not possible.2) Preoperative embolization has been demonstrated to decrease operative times, surgical blood loss, infection rates, and concomitant risks of anesthesia. Additionally, the surgical resection is often made less arduous technically due to softening of the tumor.9)10)
Various agents have been described in preoperative tumor embolization, with the most common being polyvinyl alcohol (PVA).10) Other described agents include gelatin microspheres, alcohol, gelfoam powder and liquid agents including n-butylcyanoacrylate (NBCA) and Onyx.10) Taki et al. first introduced the use of Onyx as a new liquid non adhesive material in the embolization of three cerebral arteriovenous malformations (AVMs).12) Onyx has now become a well-accepted method for embolizing AVMs.7) Its use in embolization of meningiomas was first reported by Gobin et al.4) in 8 cases with successful preoperative devascularization. Further depictions of Onyx embolization of meningiomas in the literature are relatively sparse.5)8)9)10)11)13) The purpose of this report was to highlight in detail our experience with Onyx embolization of large or giant extra-axial tumors.
We reviewed our institutional endovascular database for patients undergoing preoperative embolization of extra-axial tumors with Onyx from 2008 to 2014. We extracted patient demographic information such as age and sex, presentation modality, tumor size, tumor location, vascular supply, tumor pathology, technical complications, surgical blood loss and long-term results.
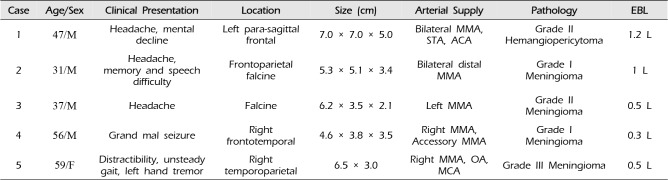
Five patients at our institution underwent preoperative Onyx embolization for extra-axial hypervascular tumors (Table 1). The five cases included four falcine or convexity meningiomas (2 grade I, 1 grade II and 1 grade III) and one hemangiopericytoma (grade II); all tumors were large or giant with middle meningeal artery supply. One case involved Onyx embolization only; the other four tumors were embolized by Onyx along with other agents. Satisfactory devascularization was obtained in all cases as determined by radiographic examination and by both the embolizing and operative physicians. Two patients underwent surgery on the same day of embolization; the remaining three underwent resection on the following day. There were no major complications related to embolization or surgery detected in any of the patients; surgical estimated blood loss ranged from 0.3 to 1.2 liters (median: 0.5 liters).
A 47-year-old right handed man presented with intermittent progressive headaches for 5 weeks and facial numbness. Magnetic resonance imaging (MRI) revealed a 7 cm extra-axial, enhancing mass arising from the left frontal para-sagittal convexity (Fig. 1A). Significant mass effect and edema was present. Invasion of the superior sagittal sinus (SSS) and frontal calvarium was also demonstrated. Angiography revealed significant supply to the tumor from the left external carotid artery (ECA), principally via the superficial temporal artery (STA) and middle meningeal artery (MMA) (Fig. 1B). Preoperative embolization with Onyx allowed significant devascularization of the majority of the tumor (Fig. 1C). The patient was taken immediately to the operating where he underwent total surgical resection of the tumor. The results of pathology confirmed the presumptive diagnosis of WHO grade II hemangiopericytoma. Postoperatively, the patient was neurologically intact. No evidence of tumor recurrence was seen on the 2 year follow up MRI.
A 31-year-old male presented with progressively worsening headaches, intermittent memory problems, and difficulty speaking. Imaging revealed a 5.3 × 5.1 × 3.4 cm extra-axial, falcine lesion over the frontoparietal vertex, with mass effect deforming the subjacent bilateral frontal and parietal lobes (Fig. 2A). The patient underwent cerebral angiography which demonstrated bilateral supply of what was thought to be a large falcine meningioma from distal branches of the middle meningeal artery, showing a classic spoke-wheel pattern filling of the tumor (Fig. 2B). The venous phase showed lack of filling of the middle third of the SSS, though normal filling of the anterior and posterior thirds, suggesting venous sinus occlusion of the middle portion with rerouted venous flow. Onyx embolization via the MMA was undertaken (Fig. 2C). Subsequent control angiography demonstrated occlusion of the tumor and the distal middle meningeal artery. Surgical resection was performed the following day, revealing a grade I meningioma. MRI at 2-year follow up showed no recurrence of the tumor.
A 37-year-old right-handed man presented with headache due to a recurrent falcine meningioma. Magnetic resonance imaging demonstrated a heterogeneously enhancing mass along the anterior falx (Fig. 3A). Cerebral angiography showed multiple arterial feeders to the tumor, primarily from the left MMA (Fig. 3B). Preoperative Onyx embolization resulted in occlusion of the left MMA (Fig. 3C). Bifrontal craniotomy with resection of the mass was performed on post-embolization day 1. Pathology was consistent with a grade II meningioma. No postoperative complications were encountered. MRI showed no recurrence of tumor at 1-year follow up.
A 56-year-old right-handed man presented with a grand mal seizure. Imaging revealed a large contrast enhancing mass compressing the right hemisphere consistent with a meningioma (Fig. 4A). The patient underwent cerebral angiography which demonstrated tumor blood supply from the MMA and accessory MMA (Fig. 4B). Superior and medial displacement of the middle cerebral artery (MCA) vasculature by the tumor was noted. Successful embolization of the tumor from the accessory MMA and MMA was performed using embolic microspheres, Onyx, and detachable pushable coils (Fig. 4C). As in the previous two cases, complete surgical resection of the tumor was performed the following day, and the pathology revealed a grade I meningioma. Postoperatively, the patient did well aside from a transient bout of sialdenitis attributed to inhalation anesthetic.
A 59-year-old female presented with increased distractibility, unsteady gait, and left handed tremor. Imaging demonstrated a right temporoparietal hypervascular extraxial mass (Fig. 5A). At preoperative embolization, the angiogram showed tumor supply from the right MMA, right occipital artery and some pial vessels from the right MCA (Fig. 5B). Post embolization angiography showed that a significant portion of the tumor had been devascularized (Fig. 5C). Surgical resection occurred the same day. The procedure was uneventful with no complications. The histologic analysis of the tumor confirmed grade III anaplastic meningioma.
Onyx is a nonpolymerizing liquid agent composed of ethylene-vinyl alcohol copolymer dissolved in dimethyl sulfoxide. During Onyx injection, the material will precipitate upon contact with aqueous fluid and form a spongy cast that obstructs blood flow. The three principal advantages of Onyx over other glues are its more permanent nature, its better control during release, and lower probability of sticking to the catheter.3)4)5)7) When compared with particles, Onyx is considered to allow for a more controlled injection due to its gradual centripetal precipitation which allows for slower and more accurate injections. The operator may even perform angiographic runs during the Onyx infusion while assessing the progress of the injection.3)4)5)7)
Few published reports of Onyx embolization for meningiomas exist.4)5)8)9)11)13) Some have suggested Onyx should be avoided in tumor embolization because of the high associated cost as well as the large volume required for adequate tumor devascularization.8)9) However, some physicians have reported a preferred use of Onyx especially for the embolization of anterior skull based meningiomas due to collateral tumor supply and the ophthalmic artery. The increased control in Onyx embolization was felt to decrease the chance of embolic material reflux into the central retinal artery.13) One large retrospective study of 100 patients (including 39 meningiomas) with hypervascular head, neck and spinal tumors undergoing Onyx embolization was published recently, demonstrating no major embolization complications.8) Other reports have also demonstrated a lack of significant complications due to Onyx tumor embolization.4)5)9)11)13) Our report reaffirms this low complication rate while providing pictoral evidence of Onyx penetration into the tumor bed (Fig. 1 and Fig. 4). The only major complication linked to Onyx in tumor embolization has been a resultant disseminated intravascular coagulation (DIC) following embolization, although only a hypothesis by the authors.14) Direct tumoral puncture with onyx embolization has also been described as a method.1)3)
While many reasonable embolization agents are available, Onyx was specifically chosen in these hypervascular tumors due to its increased ability to penetrate multiple supplying vessels over repeated injections, thereby increasing the amount of tumor embolized. Particle embolization will only allow penetration of supplying vessels with the highest direct flow. However, slow, controlled, and visualized penetration of the tumor with Onyx will allow occlusion of one territory before recruitment into other vascular territories with increased ease. In addition, the concern that such high flow may allow particle migration to the venous phases during the embolization of the hemangiopericytoma, possibly increasing the risk of venous thrombosis, made us opt for Onyx in that particular case.
Some recent reports have described the delayed resection of embolized tumors without demonstrating increased complication rates.6)8)11) We prefer resection within 24 hours as a means to decrease the likelihood of vascular recruitment around the embolized vessels and also as a cost efficient approach that can even be performed under the same anesthetic for patients undergoing surgery the same day. In addition, potential post-embolization edema is met with swift surgical excision with this more expedient approach, though this was not ostensibly encountered in this series where we demonstrate the success of Onyx embolization of these tumors without associated complications.
Preoperative embolization of extra-axial hypervascular tumors using Onyx is a recent approach in their endovascular adjunctive management. This series augments the expanding literature suggesting the safety and efficacy of Onyx in preoperative tumor embolization, underscoring the value of being able to attain extensive devascularization via only one supplying pedicle.
References
1. Ding D, Kreitel D, Liu KC. Onyx embolization of an intracranial hemangiopericytoma by direct transcranial puncture. Interv Neuroradiol. 2013; 12. 19(4):466–470. PMID: 24355151.

2. Dowd CF, Halbach VV, Higashida RT. Meningiomas: the role of preoperative angiography and embolization. Neurosurg Focus. 2003; 7. 15(1):E10. PMID: 15355012.

3. Elhammady MS, Peterson EC, Johnson JN, Aziz-Sultan MA. Preoperative onyx embolization of vascular head and neck tumors by direct puncture. World Neurosurg. 2012; May-Jun. 77(5-6):725–730. PMID: 22079824.

4. Gobin YP, Murayama Y, Milanese K, Chow K, Gonzalez NR, Duckwiler GR, et al. Head and neck hypervascular lesions: embolization with ethylene vinyl alcohol copolymer--laboratory evaluation in Swine and clinical evaluation in humans. Radiology. 2001; 11. 221(2):309–317. PMID: 11687669.

5. Gore P, Theodore N, Brasiliense L, Kim LJ, Garrett M, Nakaji P, et al. The utility of onyx for preoperative embolization of cranial and spinal tumors. Neurosurgery. 2008; 6. 62(6):1204–1211. PMID: 18824987.

6. Kai Y, Hamada J, Morioka M, Yano S, Todaka T, Ushio Y. Appropriate interval between embolization and surgery in patients with meningioma. AJNR Am J Neuroradiol. 2002; 1. 23(1):139–142. PMID: 11827886.
7. Pierot L, Cognard C, Herbreteau D, Fransen H, van Rooi WJ, Boccardi E, et al. Endovascualr treatment of brain arteriovenous malformations using a liquid emboilc agent: results of a prospective, multicentre study (BRAVO). Eur Radiol. 2013; 10. 23(10):2838–2845. PMID: 23652849.
8. Rangel-Castilla L, Shah AH, Klucznik RP, Diaz OM. Preoperative Onyx embolization of hypervascular head, neck, and spinal tumors: experience with 100 consecutive cases from a single tertiary center. J Neurointerv Surg. 2014; 1. 6(1):51–56. PMID: 23268473.

9. Rossitti S. Preoperative embolization of lower-falx meningiomas with ethylene vinyl alcohol copolymer: technical and anatomical aspects. Acta Radiol. 2007; 4. 48(3):321–326. PMID: 17453504.

10. Shah AH, Patel N, Raper DM, Bregy A, Ashour R, Elhammady MS, et al. The role of preoperative embolization for intracranial meningiomas. J Neurosurg. 2013; 8. 119(2):364–372. PMID: 23581584.

11. Shi ZS, Feng L, Jiang XB, Huang Q, Yang Z, Huang ZS. Therapeutic embolization of meningiomas with Onyx for delayed surgical resection. Surg Neurol. 2008; 11. 70(5):478–481. PMID: 18261767.

12. Taki W, Yonekawa Y, Iwata H, Uno A, Yamashita K, Amemiya H. A new liquid material for embolization of arteriovenous malformations. AJNR AM J Neuroradiol. 1990; Jan-Feb. 11(1):163–168. PMID: 2105599.
13. Trivelatto F, Nakiri GS, Manisor M, Riva R, Al-Khawaldeh M, Kessler I, et al. Preoperative onyx embolization of meningiomas fed by the ophthalmic artery: a case series. AJNR Am J Neuroradiol. 2011; 10. 32(9):1762–1766. PMID: 21835949.

14. Velez AM, Friedman WA. Disseminated intravascular coagulation during resection of a meningioma: case report. Neurosurgery. 2011; 4. 68(4):E1165–E1169. PMID: 21242833.

Fig. 1
Case 1. Preoperative T1-weighted post contrast coronal magnetic resonance imaging showing an extra-axial mass with significant mass effect and edema on the adjacent brain parenchyma (A). Anteroposterior view of left external carotid artery arteriogram demonstrating filling of the tumor through branches of the left superficial temporal artery and the left middle meningeal artery draining into a venous fistula and also supplying the tumor through multiple collaterals (B). Anteroposterior skull film demonstrating Onyx cast (C).

Fig. 2
Case 2. Preoperative T1-weighted post contrast coronal magnetic resonance imaging demonstrates an extra-axial, falcine lesion over the frontoparietal vertex with mass effect and an associated inferolateral peritumoral cyst (A). Anteroposterior view of a distal left external carotid artery arteriogram illustrates the classic "spoke wheel" filling of the falcine meningioma supplied by distal branch of the middle meningeal artery (C). Lateral view of post-embolization angiogram of left external carotid artery shows occlusion of the distal middle meningeal artery.

Fig. 3
Case 3. Preoperative T1-weighted post contrast sagittal magnetic resonance imaging shows an extra-axial enhancing mass centered in the falx cerebri (A). This lesion extended bilaterally with invasion of the anterior and mid superior sagittal sinus. Anteroposterior view of left external carotid artery arteriogram showing multiple arterial feeders to the tumor, mainly from the left middle meningeal artery (B). Anteroposterior view of post-embolization left common carotid artery arteriogram (C).
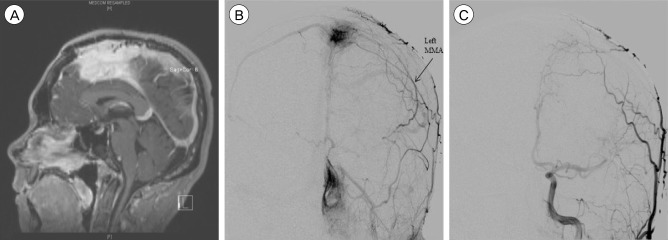
Fig. 4
Case 4. Preoperative T1-weighted post contrast axial magnetic resonance imaging shows a right frontal extra-axial mass with intraosseous extension and adjacent dural thickening (A). Lateral view of right external carotid artery angiogram shows a hypervascular tumor blush, supplied by the middle meningeal artery and accessory middle meningeal artery (B). Anteroposterior, unsubtracted view of post-embolization of right external carotid artery angiogram demonstrates Onyx casting within the distal middle meningeal artery, with markedly diminished supply to the tumor but little flow from the accessory middle meningeal artery (C).
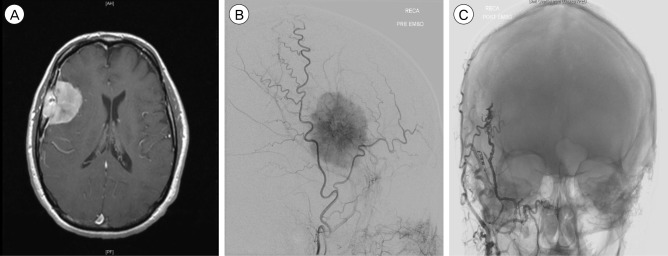
Fig. 5
Case 5. Preoperative T1-weighted post contrast coronal magnetic resonance imaging shows a right temporal occipital extra-axial mass, with midline shift and mass effect noted on the right lateral ventricle and extensive edema (A). Anteroposterior view of right external carotid artery angiogram shows arterial supply to the tumor from branches of right occipital artery and the middle meningeal artery (B). Lateral view of post-embolization of right common carotid artery angiogram demonstrates little residual supply to the tumor (C).

Table 1
Summary of 5 patients with extra-axial hypervascular tumors treated with Onyx




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download