Abstract
Coronary-subclavian steal (CSS) can occur after coronary artery bypass grafting (CABG) using the internal thoracic artery (ITA). Subclavian artery (SA) stenosis proximal to the ITA graft causes CSS. We describe a technique for cardiac and cerebral protection during endovascular stenting for CSS due to right SA origin stenosis after CABG. A 64-year-old man with a history of CABG using the right ITA presented with exertional right arm claudication. Angiogram showed a CSS and retrograde blood flow in the right vertebral artery (VA) due to severe stenosis of the right SA origin. Endovascular treatment of the right SA stenosis was planned. For cardiac and cerebral protection, distal balloon protection by inflating a 5.2-F occlusion balloon catheter in the SA proximal to the origin of the right VA and ITA through the right brachial artery approach and distal filter protection of the right internal carotid artery (ICA) through the left femoral artery (FA) approach were performed. Endovascular stenting for SA stenosis from the right FA approach was performed under cardiac and cerebral protection by filter-protection of the ICA and balloon-protection of the VA and ITA. Successful treatment of SA severe stenosis was achieved with no complications.
Coronary-subclavian steal (CSS) can occur after coronary artery bypass grafting (CABG) using the internal thoracic artery (ITA). Subclavian artery (SA) stenosis proximal to the ITA graft may cause CSS.2)4)6) Endovascular treatment for SA stenosis has been reported with high technical and clinical success rates and with low complication rates.8) Although the use of cerebral protection devices in endovascular stenting for extracranial internal carotid artery (ICA) stenosis is established, the use of cerebral protection devices in an endovascular stenting for SA stenosis is less well established.7)8)15) We performed endovascular stenting for SA stenosis under filter-protection of the ICA and balloon-protection at the right SA proximal to the VA and ITA origin during SA stenting for right SA stenosis with CSS. We describe a technique for simultaneous cardiac and cerebral protection during endovascular stenting for right SA origin stenosis in a patient with CSS after CABG.
A 64-year-old man who had undergone CABG using the bilateral ITAs and the right gastroepiploic artery presented with exertional right arm claudication. In comparison of the arms, he had a difference in systolic blood pressure of approximately 30 mmHg (right, 96/64 mmHg; left, 125/69 mmHg). He had no neurological deficits or cardiac symptoms. Computed tomography (CT) angiography showed severe stenosis with calcification in the right SA origin and poor visualization of the right ITA (Fig. 1A). Left vertebral angiography showed retrograde blood flow in the right VA (Fig. 1B). Angiography showed 90% stenosis in the right SA origin and no antegrade blood flow in the vertebral artery (VA) or right ITA graft secondary to severe stenosis of the right SA origin (Fig. 2A). Right subclavian angiography showed to-and fro blood flow in the right ITA. The patient preferred endovascular treatment rather than surgery; therefore, we planned to perform endovascular stenting for SA stenosis. The patient was already receiving clopidogrel (75 mg daily) and aspirin (100 mg daily) orally due to a past history of percutaneous coronary intervention with drug-eluting stents and bare metal stents.
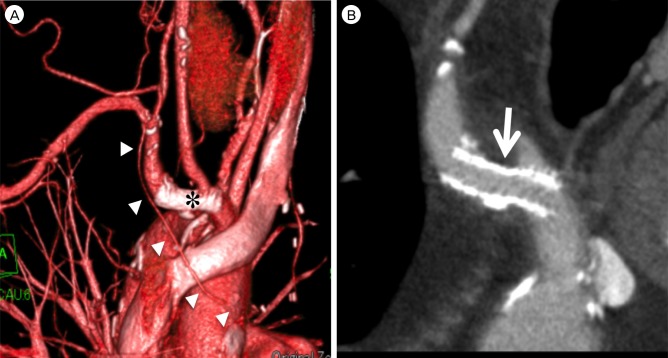
The endovascular procedure was performed under local anesthesia. An activated clotting time of more than 300 seconds was maintained by intravenous administration of heparin. A 4-Fr 90 cm sheath (FUBUKI sheath: Asahi Intecc, Aichi, Japan) was navigated into the right common carotid artery through the left femoral artery (FA) approach. For protection of the right ICA, a filter-wire (FilterWire EZ: Boston Scientific, Natick, MA, USA) was deployed into the right ICA through the 4-Fr femoral sheath (Fig. 2B). A 5-Fr 11 cm sheath was inserted into the right brachial artery (BA). To perform protection of the right VA and ITA, a 5.2-Fr occlusion balloon catheter (Selecon MP Catheter II: Terumo Clinical Supply, Gifu, Japan) was navigated into the SA proximal to the origin of the right VA and ITA through the right brachial sheath. A 6-Fr 90 cm sheath (FUBUKI sheath: Asahi Intecc, Aichi, Japan) was positioned at the innominate artery (IA) through the right FA approach, and a 0.035-inch stiff type 300-cm guidewire was navigated into the BA. A 5.2-Fr occlusion balloon catheter at the SA proximal to the origin of the right VA and ITA was inflated (Fig. 2B). Under filter-protection of the ICA and balloon-protection of the VA and ITA for simultaneous cardiac and cerebral protection, predilation was performed using a 6 × 20 mm PTA balloon. Next, a 7 × 27 mm balloon-expandable stent (Express Vascular LD: Boston Scientific) was deployed to the SA stenosis (Fig. 2C). After stent deployment, 30 mL of blood was aspirated through the 5.2-Fr occlusion balloon catheter using a 50 mL syringe. After no debris was confirmed in the aspirated blood, the 5.2-Fr occlusion balloon catheter was deflated. The occlusion catheter and filter-wire were retrieved. Debris was not observed in the filter-wire. Angiography showed excellent dilatation after stenting and antegrade blood flow in the right VA and through the right ITA graft (Fig. 2D). After the procedure, intravenous administration of heparin was terminated, and argatroban was administered for 12 hr. Postoperative diffusion-weighted images showed no hyper-intensity lesions. The patient was discharged with no new neurological deficits or chest symptoms. Follow-up CT angiography at 3 months showed good patency of the SA stent and good visualization of the right ITA graft (Fig. 3).
Protection against distal embolic complications is important during endovascular treatment. Although cerebral protection during extracranial ICA stenting is established, cerebral protection during SA stenting has not yet been established. The reported neurological complication rate of SA angioplasty ranges from 0.4 to 4.7%.7) Ringelstein and Zeumer9) used continuous ultrasound monitoring to observe VA blood flow of the SA stenosis or occlusion with subclavian steal syndrome before, during, and after PTA. The flow direction within the VA did not immediately change to antegrade but rather did so gradually within 20 s to several minutes. Therefore, they concluded that this delay of flow-reversal served as a protective mechanism against cerebral embolism during PTA only. If PTA or direct stenting for SA stenosis with subclavian steal was performed, embolic protection may not be necessary. However, SA stenting after predilation required distal embolic protection because VA blood flow changed to the antegrade direction after predilation.
CSS, which was first described in 1974, can be caused by retrograde or insufficient blood flow through an ITA graft. Proximal stenosis of the SA was the most frequent cause.2)4)6) Incidence up to 3.4% after CABG was reported.2)5) The treatment for CSS was thoracotomy with aortosubclavian bypass, carotid subclavian bypass graft, and, more recently, angioplasty and stenting.10)13) Endovascular treatment in CSS due to SA stenosis after CABG has already been reported, and endovascular therapy with PTA and stenting appeared to be an effective treatment for CSS due to SA stenosis.2)6)10)13)14) On the other hand, cardiac and cerebral protection during SA stenting in CSS was not performed.2)6)10)13)14) Although native coronary stent angioplasty is performed with no distal embolic protection, the cardiac complication rate during SA angioplasty in CSS is unknown. On the other hand, the cerebral protection methods during stenting for stenosis of the right SA origin or IA proximal to the right SA origin have been reported. The anterior circulation was protected by placing a filter-wire or balloon protection device in the ICA, and the posterior circulation was protected by inflating the balloon of the catheter at the SA or by placing a filter-wire or balloon protection device in the VA.1)3)11)12) Therefore, we think that cardiac and cerebral protection should be performed simultaneously during SA stenting for CSS as well as the right SA origin or IA.
In the current case, we performed protection of the right ICA, VA, and ITA for cerebral and cardiac protection. ICA protection was performed to protect against distal embolization by plaque shift from the SA origin. We used a filter-wire for ICA protection to maintain antegrade flow. Stenting after predilation may result in distal embolization when retrograde flow in right VA and ITA changes into antegrade flow after predilation, therefore, right VA and ITA protection was performed. We used a balloon catheter for VA and ITA protection to induce retrograde flow in VA and ITA and to aspirate blood through the lumen of the balloon catheter.
References
1. Albuquerque FC, Ahmed A, Mitha A, Stiefel M, McDougall CG. Endovascular recanalization of the chronically occluded brachiocephalic and subclavian arteries: technical considerations and an argument for embolic protection. World Neurosurg. 2013; 12. 80(6):e327–e336. PMID: 23043999.

2. Bicknell CD, Subramanian A, Wolfe JH. Coronary subclavian steal syndrome. Eur J Vasc Endovasc Surg. 2004; 2. 27(2):220–221. PMID: 14718907.

3. Guimaraes M, Muhlert MK, Enterkin J, Schonholz C. Can we provide complete cerebral protection during innominate artery stenting? J Endovasc Ther. 2010; 10. 17(5):657–659. PMID: 20939726.
4. Harjola PT, Valle M. The importance of aortic arch or subclavian angiography before coronary reconstruction. Chest. 1974; 10. 66(4):436–438. PMID: 4416304.

5. Lobato EB, Kern KB, Bauder-Heit J, Hughes L, Sulek CA. Incidence of coronary-subclavian steal syndrome in patients undergoing noncardiac surgery. J Cardiothorac Vasc Anesth. 2001; 12. 15(6):689–692. PMID: 11748514.

6. Machado C, Raposo L, Leal S, Goncalves PA, Mesquita Gabriel H, Teles RC, et al. Coronary-subclavian steal syndrome: percutaneous approach. Case Rep Cardiol. 2013; 2013:757423. PMID: 24829810.

7. Michael TT, Banerjee S, Brilakis E. Subclavian artery intervention with vertebral embolic protection. Catheter Cardiovasc Interv. 2009; 7. 74(1):22–25. PMID: 19530179.

8. Miyakoshi A, Hatano T, Tsukahara T, Murakami M, Arai D, Yamaguchi S. Percutaneous transluminal angioplasty for atherosclerotic stenosis of the subclavian or innominate artery: angiographic and clinical outcomes in 36 patients. Neurosurg Rev. 2012; 1. 35(1):121–125. discussion 125-6. PMID: 21643683.

9. Ringelstein EB, Zeumer H. Delayed reversal of vertebral artery blood flow following percutaneous transluminal angioplasty for subclavian steal syndrome. Neuroradiology. 1984; 26(3):189–198. PMID: 6234477.

10. Sadek MM, Ravindran A, Marcuzzi DW, Chisholm RJ. Complete occlusion of the proximal subclavian artery post-CABG: presentation and treatment. Can J Cardiol. 2008; 7. 24(7):591–592. PMID: 18612504.

11. Sakamoto S, Kiura Y, Kajihara Y, Mukada K, Kurisu K. Endovascular stenting of symptomatic innominate artery stenosis under distal balloon protection of the internal carotid and vertebral artery for cerebral protection: a technical case report. Acta Neurochir (Wien). 013; 2. 155(2):277–280. PMID: 23263481.

12. Shah N, Nee LM, Raval AN. Percutaneous revascularization of subclavian artery chronic occlusion with dual cerebral artery protection. Catheter Cardiovasc Interv. 2008; 6. 71(7):992–994. PMID: 18383148.

13. Tortoledo F, Sánchez A, Izaguirre L, Guerrero J, Trujillo MH. Endovascular repair of symptomatic coronary-subclavian steal syndrome due to stenosis of the proximal left subclavian artery. Cardiol Rev. 2005; May-Jun. 13(3):128–129. PMID: 15831145.

14. Westerband A, Rodriguez JA, Ramaiah VG, Diethrich EB. Endovascular therapy in prevention and management of coronary-subclavian steal. J Vasc Surg. 2003; 10. 38(4):699–703. discussion 704. PMID: 14560215.

15. Yadav JS, Wholey MH, Kuntz RE, Fayad P, Katzen BT, Mishkel GJ, et al. Protected carotid-artery stenting versus endarterectomy in high-risk patients. N Engl J Med. 2004; 10. 351(15):1493–1501. PMID: 15470212.

Fig. 1
(A) Computed tomography angiography shows severe stenosis with calcification in the right subclavian artery origin (arrow) and poor visualization of the right internal thoracic artery graft (arrowheads). (B) Left vertebral angiography shows retrograde blood flow in the right vertebral artery.
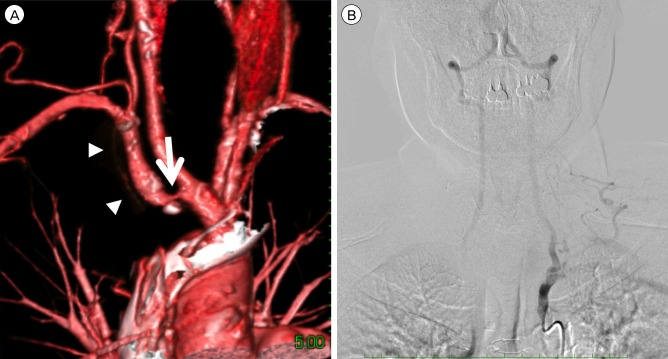
Fig. 2
(A) Preoperative angiography shows 90% stenosis in the right subclavian artery origin (arrow). (B) The filter-wire (arrow) is deployed into the right internal carotid artery through the 4-Fr femoral sheath. A 5.2-Fr occlusion balloon catheter is navigated into the subclavian artery proximal to the origin of the right vertebral artery and internal thoracic artery through the right brachial sheath, and is then inflated (double arrows). (C) The 7 × 27 mm balloon-expandable stent is deployed to the subclavian artery origin stenosis (asterisk). (D) Postoperative angiogram shows excellent dilatation.
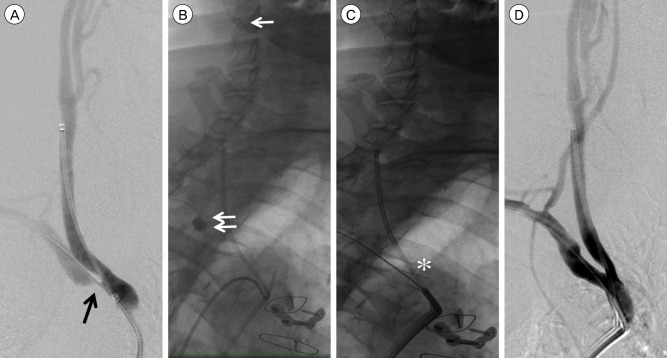
Fig. 3
(A) Follow-up computed tomography (CT) angiography at 3 months shows stent deployment in the right subclavian artery origin (asterisk) and good visualization of the right internal thoracic artery graft (arrowheads). (B) Follow-up CT angiography at 3 months shows a good patency of the stent in the subclavian artery (arrow).




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download