Abstract
Contrast extravasation on computed tomography angiography (CTA) is rare but becoming more common, with increasing use of CTA for various cerebral vascular diseases. We report on two cases of spontaneous subarachnoid hemorrhage (SAH) in which the CTA showed a saccular lesion of the upper basilar trunk suggesting a ruptured aneurysm. However, no vascular lesion was observed on immediate subsequent digital subtraction angiography (DSA).
In one case, repeated follow up DSA was also negative. The patient was treated conservatively and discharged with no neurologic deficit. In the other case, the patient showed sudden mental deterioration on the third hospital day and her brain CT showed rebleeding. The immediate follow up DSA showed contrast stagnation in the vicinity of the upper basilar artery, suggestive of pseudoaneurysm. Double stent deployment at the disease segment was performed.
Due to the frequent use of CTA, contrast extravasation is an increasingly common observation. Physicians should be aware that basilar artery extravasation can mimic the appearance of an aneurysm.
Nontraumatic subarachnoid hemorrhage (SAH) is caused by rupture of a cerebral aneurysm in 80-90% of patients.4) Unfortunately, aneurysmal SAH has a high mortality rate of 45%.1) Therefore, immediate diagnosis and treatment are very important in prevention of catastrophic deterioration.
Digital subtraction angiography (DSA) remains the gold standard as the main technique for diagnosis of intracranial aneurysms.4)5)7) Computed tomography angiography (CTA) is a rapid, less invasive modality for patients with intracranial aneurysm and is useful for evaluation of patients with aneurysmal SAH. Therefore, CTA is more often used in the initial evaluation of SAH.4)7)10)11)14)
However, in some patients with a nontraumatic SAH, no aneurysms are found on the initial DSA.3)9)11) Contrast extravasation of a ruptured intracranial aneurysm during CTA is rare, but is becoming more common, with increasing use of CTA for various cerebral vascular diseases and increasing resolution of CTA. We report on two similar cases, but with different clinical course of contrast extravasation from the distal basilar artery (BA) during CTA but negative findings of DSA.
A 66-year-old man was admitted to our hospital after sudden loss of consciousness. He had suffered from a severe headache for 2 hours before his admission. He had a five-year history of taking medication for angina. On admission, he had a stuporous mental status. A pre-enhanced cranial CT showed acute diffuse SAH in the basal cistern (Fig. 1A). The 3-dimensional CTA showed a saccular lesion arising from the upper basilar artery and projecting anteriorly (Fig. 1B). DSA performed one and a half hours later showed no vascular abnormality (Fig. 1C). A repeat DSA, performed on postbleed day 10, also showed no vascular abnormality. The patient was treated conservatively and discharged after 30 days with no neurologic deficit. On follow-up at three months, the patient had no neurologic deficit, and follow up DSA also confirmed no vascular abnormality.
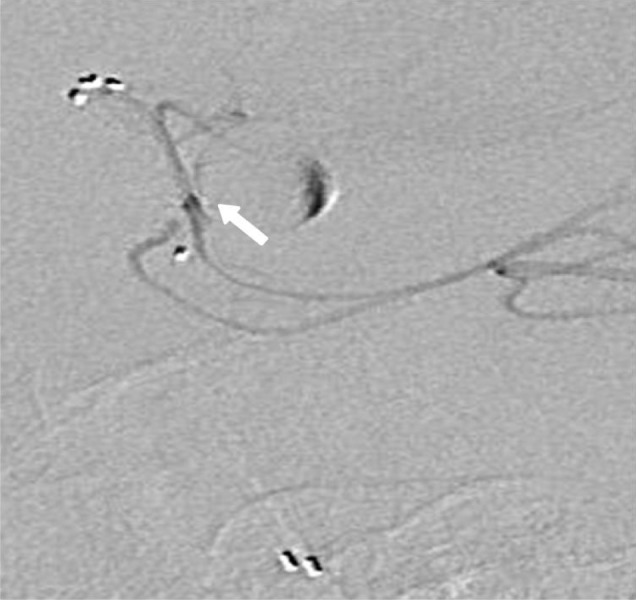
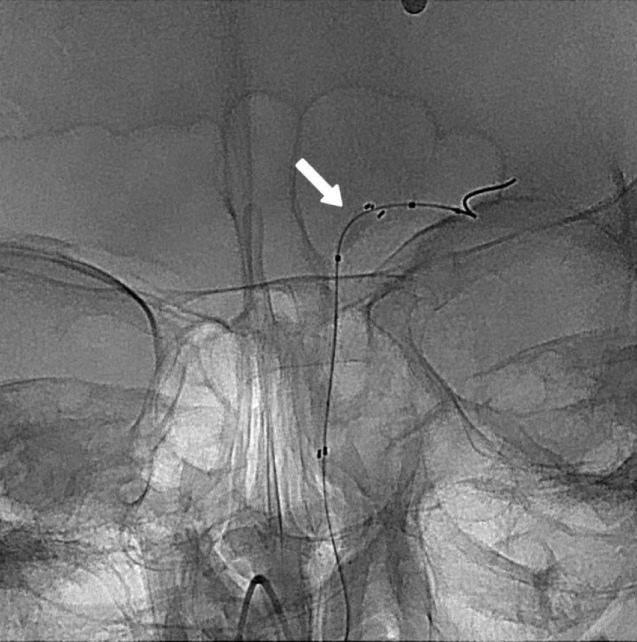
A 55-year-old woman with a medical history of chronic viral hepatitis presented to our clinic after sudden onset of headache with vomiting. We found no neurologic deficit and her mentality was drowsy. Her CT scan showed a diffuse SAH and mild hydrocephalus (Fig. 2A). CTA confirmed an upper basilar abnormality (Fig. 2B, C and D). Cerebral angiography obtained two hours later showed no vascular abnormality (Fig. 2E). The patient received an external ventricular drain (EVD) for symptomatic hydrocephalus on posthemorrhage day 2. The patient's clinical condition improved and her level of consciousness improved to alert immediately after EVD. On the second day after EVD, her mentality suddenly deteriorated to semicoma. Immediate CT scan showed an increased amount of SAH, suggestive of rebleeding. A repeat CTA after rebleeding showed no abnormal vascular lesion. However, cerebral angiography at the same time confirmed a small cylinder like contrast stagnation from the upper basilar artery at late arterial phase, indicating pseudoaneurysm formation (Fig. 3). We inserted two Solitaire stents (4 × 20 mm, ev3, Irvine, CA, USA) for flow diversion and anticipating thrombus formation of the pseudoaneurysm. The patient's clinical course was uneventful, however, one-month follow up CTA still showed a saccular lesion from the upper basilar artery. Therefore, we decided to perform DSA and intervention. DSA still showed contrast stagnation at late arterial phase on the upper basilar artery and superselective microcatheter angiography confirmed a pseudoaneurysm arising from a small perforating artery of the superior cerebellar artery (SCA) (Fig. 4). Due to concern about cerebellar infarction, we could not sacrifice the SCA. To facilitate thrombus formation of the pseudoaneurysm, we performed repeated temporary balloon occlusion using a Sceptor XC balloon (4 × 10 mm, Microvention, Tustin, CA, USA) and achieved decreased contrast inflow to the pseudoaneurysm (Fig. 5). On follow-up at 11 months, the patient had no neurologic deficit, and she was able to live independently. Follow up DSA performed 11 months after hemorrhage confirmed no contrast stagnation no abnormal vascular legion (Fig. 6).
In the current cases, we report on two patients with contrast extravasation from the basilar artery observed on CTA, but negative findings with immediate subsequent cerebral angiography. Reported incidence of patients with SAH of unknown etiology was approximately 10 to 30%.3)5)9)12) The precise cause of angiogram-negative SAH is unclear. However, patients with angiogram-negative SAH have a more favorable prognosis and lower rebleeding rate than those with other distributions of aneurysmal SAH.3)9)11)12)
DSA has been the gold standard method for detection and diagnosis of intracranial aneurysms.
However, DSA has a weakness of being very invasive and takes time to perform. The risk of complications has been reported as 0.9% to 2.3% with permanent deficit in 0.3%4) and 0.6% of cases occurring in the non-severe neurologic complications, including formation of hematoma, peripheral thromboembolic events, transient hypotension, arteriovenous fistulas, or infection.2)4)
Recently, because it is less invasive and the procedure is easier to perform than DSA, CTA is useful for detection of intracranial aneurysms. Because contrast media for CTA is injected intravenously, it is less invasive than arterial injections required for DSA.7) Therefore, CTA is now used as the diagnostic method of first choice for detection of aneurismal SAH, vascular malformations, stenotic vessel disease, vasospasm, traumatic vessel disease, and for development of an occupational treatment plan.4)10)14) Sensitivity of CTA for detection of intracranial aneurysms between 83.6% and 92.7%, and specificity between 77.2% and 98.9% has been reported.4) Due to the increased usefulness, sensitivity, and specificity for detection of intracranial aneurysms, use of CTA has recently become more frequent. However, CTA has still not replaced DSA as the standard method for detection of intracranial aneurysms. The disadvantages of CTA were difficulty in distinguishing small perforating arteries with a diameter less than 1 mm, difficulty in discriminating an infundibular dilatation of the arterial origin from an aneurysm, artifact of the adjacent vessel, display of venous systems imitating aneurysms, and extravasated blood such as hemorrhage surrounding the aneurysm imitating vascular structures.
Almost all extravasation occurs from ruptured aneurysms, however, it has also been reported in association with other rare situations such as microangioma, infarction with SAH due to obliteration of a perforating artery or increase in arterial pressure after injection of contrast media.8)10) Another potentiality of extravasation is a very small sized true aneurysmal SAH that is not large enough to be recognized. Extravasation on CTA has been reported previously, such as the "cap sign", "corkscrew sign", "puddling", and the "spot sign". The "cap sign" and the "corkscrew sign" are patterns of extravasation. The "puddling" indicates multiple areas of contrast media on CTA and the "spot sign" is enhancing foci within a hematoma mass associated with hematoma growth and poor prognosis.7)13)14) Nevertheless, sometimes a lesion that was initially detected on the CTA was not detected using DSA. Failure to detect an aneurysmal rupture by DSA that was detected on the initial CTA has been ascribed to a result of vasospasm, dissecting aneurysm, spontaneous thrombosis of the aneurysm, microaneurysm, or error of interpretation.5)11) Aneurysms detected on CTA that do not present on initial DSA can become visible on repeat DSA. Some authors have previously reported discovery rates of repeat DSA of occult aneurysms overlooked on the initial DSA of 2 and 36%.5)6)11)
In the second case, we found a small cylinder like vascular abnormality, which was confirmed by repeated DSA after rebleeding. The proposed mechanism of this case could be as follows. First bleeding was due to rupture of a small perforating vessel arising from the superior cerebellar artery and then spontaneous thrombosis occurred. Therefore, despite detection of a saccular lesion on initial CTA, we could not detect vascular abnormality on DSA. Subsequent rebleeding into the hematoma could cause pseudoaneurysm formation. Therefore we were able to detect contrast stagnation on repeated DSA. Flow diversion through double stents and temporary balloon occlusion could facilitate thrombosis within the pseudoaneurym. Finally, we achieved complete occlusion of the pseudoaneurysm arising from the SCA.
We reported on two extremely rare cases involving patients who showed nonaneurysmal, angiogram-negative SAH in which supposed contrast extravasation on initial CTA mimicked a basilar artery trunk aneurysm. Based on our experience, repeated DSA is mandatory when encountering a patient with extravasation on CTA with negative DSA findings and superselective microangiography could reduce false-negative finding and improve understanding of pathophysiology.
References
1. Brisman JL, Song JK, Newell DW. Cerebral aneurysms. N Engl J Med. 2006; 8. 355(9):928–939. PMID: 16943405.

2. Cloft HJ, Joseph GJ, Dion JE. Risk of cerebral angiography in patients with subarachnoid hemorrhage, cerebral aneurysm, and arteriovenous malformation: a meta-analysis. Stroke. 1999; 2. 30(2):317–320. PMID: 9933266.
3. Eskesen V, Sørensen EB, Rosenørn J, Schmidt K. The prognosis in subarachnoid hemorrhage of unknown etiology. J Neurosurg. 1984; 12. 61(6):1029–1031. PMID: 6502230.

4. Goddard AJ, Tan G, Becker J. Computed tomography angiography for the detection and characterization of intra-cranial aneurysms: current status. Clin Radiol. 2005; 12. 60(12):1221–1236. PMID: 16291304.

5. Inamasu J, Nakamura Y, Saito R, Horiguchi T, Kuroshima Y, Mayanagi K, et al. "Occult" ruptured cerebral aneurysms revealed by repeat angiography: result from a large retrospective study. Clin Neurol Neurosurg. 2003; 12. 106(1):33–37. PMID: 14643914.

6. Juul R, Fredriksen TA, Ringkjøb R. Prognosis in subarachnoid hemorrhage of unknown etiology. J Neurosurg. 1986; 3. 64(3):359–362. PMID: 3950713.

7. Nakatsuka M, Mizuno S, Uchida A. Extravasation on three-dimensional CT angiography in patients with acute subarachnoid hemorrhage and ruptured aneurysm. Neuroradiology. 2002; 1. 44(1):25–30. PMID: 11942496.

8. Ney JP. Midbrain stroke with angiogram-negative subarachnoid hemorrhage mimicking a perimesencephalic bleed. J Stroke Cerebrovasc Dis. 2005; May-Jun. 14(3):136–137. PMID: 17904013.

9. Ronkainen A, Hernesniemi J. Subarachnoid haemorrhage of unknown aetiology. Acta Neurochir (Wien). 1992; 119(1-4):29–34. PMID: 1481749.

10. Ryu CW, Kim SJ, Lee DH, Suh DC, Kwun BD. Extravasation of intracranial aneurysm during computed tomography angiography: mimicking a blood vessel. J Comput Assist Tomogr. 2005; Sep-Oct. 29(5):677–679. PMID: 16163041.
11. Stetson ND, Pile-Spellman J, Brisman JL. Contrast extravasation on computed tomographic angiography mimicking a basilar artery aneurysm in angiogram-negative subarachnoid hemorrhage: report of 2 cases. Neurosurgery. 2012; 11. 71(5):E1047–E1052. PMID: 22806079.
12. Tatter SB, Buonanno FS, Ogilvy CS. Acute lacunar stroke in association with angiogram-negative subarachnoid hemorrhage. Mechanistic implications of two cases. Stroke. 1995; 5. 26(5):891–895. PMID: 7740585.
13. Wada R, Aviv RI, Fox AJ, Sahlas DJ, Gladstone DJ, Tomlinson G, et al. CT angiography "spot sign" predicts hematoma expansion in acute intracerebral hemorrhage. Stroke. 2007; 4. 38(4):1257–1262. PMID: 17322083.

14. Walker MT, Wattamwar A, Mellman D, Mo J. Active hemorrhage into a postresection cavity detected by neuro-CT angiography. AJNR Am J Neuroradiol. 2005; 5. 26(5):1163–1165. PMID: 15891177.
Fig. 1
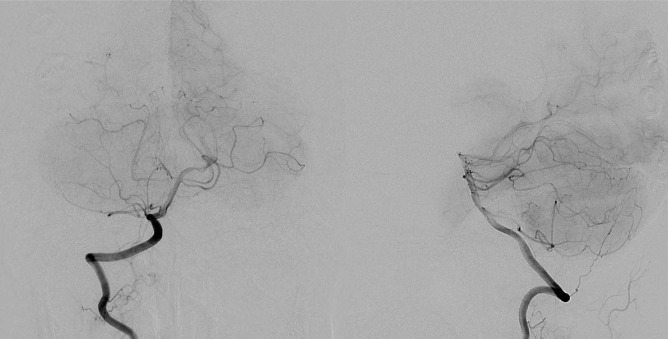
(A) Noncontrast computed tomography (CT) scan on admission shows diffuse subarachnoid hemorrhage in the prepontine cistern and both sylvian fissures. (B) 3-dimensional computed tomography angiography image demonstrates an enhancing abnormal vascularity (arrow). (C) Digital subtraction angiography of the basilar artery acquired in the anteroposterior (left) and lateral (right) views failed to detect the previously seen basilar abnormal structure.
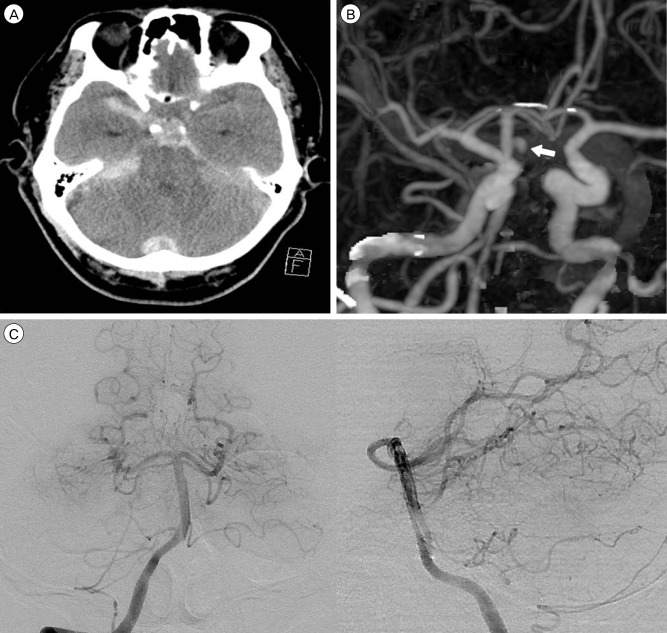
Fig. 2
(A) Initial noncontrast computed tomography (CT) scan reveals diffuse subarachnoid hemorrhage in the basal, prepontine, perimesencephalic cistern and both sylvian fissures. (B) Computed tomography angiography axial and (C) sagittal reformatted images showing an enhanced saccular structure with surrounding blood clot on the posterior surface of the basilar artery (arrow). (D) 3-D computed tomography angiography image demonstrating a cylinder-shape, enhancing abnormal structure (arrow). (E) Digital subtraction angiography of the basilar artery acquired 2 hours after the initial CT scan in the anteroposterior (left) and lateral (right) views failed to detect the previously seen basilar abnormal structure.
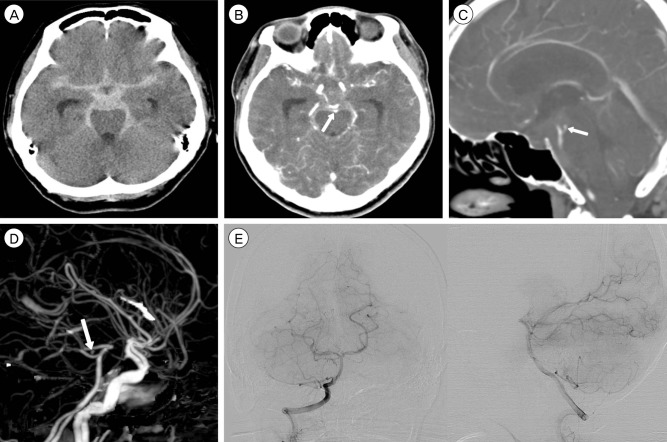
Fig. 3
Digital subtraction angiography of the basilar artery acquired 3 days after a bleeding event, in the oblique view demonstrates the cylinder-shape contrast stagnation in the upper basilar trunk at late arterial phase (arrow).

Fig. 4
Follow up digital subtraction angiography acquired 28 days after double stenting. Superselective microcatheter angiography of the left superior cerebellar artery confirms a pseudoaneurysm arising from the small superior cerebellar artery perforating artery (arrow).




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download