Abstract
Objective
We attempted to identify the presence of a so called 'March effect (or phenomenon)' (which had long been known as a 'July effect' in western countries), a transient increase in adverse outcomes during an unskilled period for new interns and residents in a teaching hospital, among a cohort of patients with spontaneous subarachnoid hemorrhage (sSAH).
Methods
A total of 455 consecutive patients with sSAH from our department database from 2008 to 2010 were enrolled retrospectively and the admission month, patient demographics and clinical characteristics, treatment modalities and discharge outcomes were analyzed. Multivariate regression analysis was used to determine whether unfavorable discharge and in-hospital mortality showed a significant increase during the unskilled months for new interns and residents (from March to May) in a pattern suggestive of a "March effect".
Results
Among 455 patients with sSAH, 113 patients were treated during the unskilled period (from March to May) and the remaining 342 patients were treated during the skilled period (from June until February of the next year). No statistically significant difference in demographics and clinical characteristics was observed between patients treated during these periods. In addition, the mortality and unfavorable discharge rates of the un-skilled period were 16.8% and 29.7% and those of the skilled period were 15.5% and 27.2%, respectively. However, no statistically significant difference was observed between them.
Spontaneous subarachnoid hemorrhage (sSAH) is still a challenging neurosurgical disease entity. Emergency and elective care of sSAH is critical given that cerebral vasospasm, rebleeding, increased intracranial pressure due to acute brain swelling, related intra-parenchymal hemorrhage, or acute hydrocephalus, hemodynamic instability, cerebral infarction, seizure, electrolytes imbalances and cardiac rhythm abnormalities due to myocardial injury are all possible life-threatening complications.5)10)17)
Surprisingly, the unnoticed sSAH remains as high as 12%, resulting in four-fold higher rates of morbidity and mortality.16) A common comment from a variety of studies suggests that early identification and treatment of sSAH and related complications are critical components to achievement of desirable outcomes.5)
Meanwhile, thorough reappraisal of educational programs for training of interns and residents in western countries has increased due to results suggesting an increment in unacceptable outcomes in the late summer (that falls during the spring in Korea), which is the unskilled season for beginner interns and residents.23) This tendency, termed a "July effect" in western countries has come from the July inrush of inexperienced interns and residents of the first year. Because the training hospital workforce is highly dependent on intern and resident doctors for duty, especially for night time and emergency room, they stand for the first line of care at these hospitals and may frequently be urged to make acute management decisions and provide care with limited guidance. Because reliable clinical evidence indicates that favorable outcomes in sSAH may be associated with early identification of the disease, rigid compliance to clinical management guidelines and experience and knowledge of corresponding physicians could play a considerable role in such outcomes.5) In Korea, a similar phenomenon might have occurred in March because of the difference in the period of educational systems between western countries and Korea. Some clinical studies on the "July effect" have been reported; on the contrary, no available study on the 'March effect' has been conducted in Korea, especially in the neurosurgical field. The authors attempted to identify a 'March effect', defined as a temporary increase in the frequency of adverse outcomes (mortality rate and unfavorable discharge rate), among a cohort of patients admitted to our hospital under the diagnosis of sSAH.
From January 2008 to December 2010, 455 consecutive patients with an acute form of spontaneous subarachnoid hemorrhage were admitted to the author's hospital. Traumatic SAH was excluded. All patients underwent routine clinical and radiographic evaluations and the authors made decisions on how to treat the patients according to their clinical and radiological information and neurological status and then obtained informed consent from the patient's family; surgical clipping, endovascular coiling and conservative therapy (including external ventricular drainage and medical treatment). The authors prefer early surgical clipping or early endovascular intervention to delayed ones.
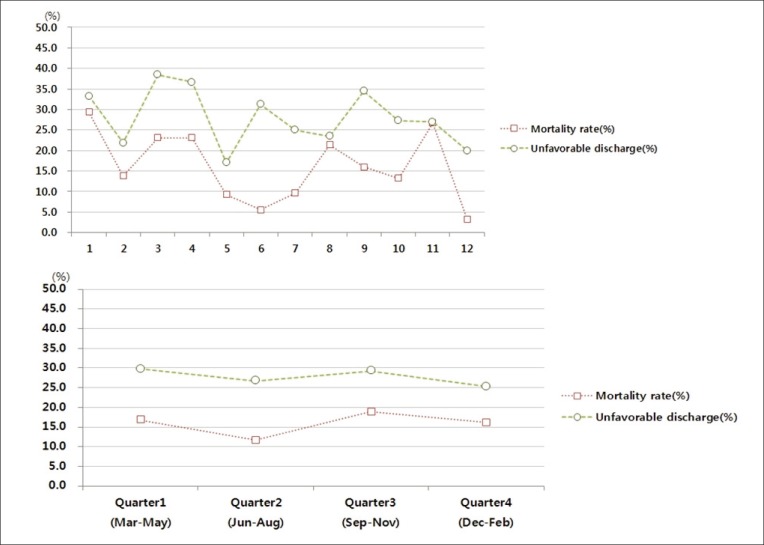
The enrolled patients were divided into four groups according to their admission month; Quarter 1 (March-May), Quarter 2 (June-August), Quarter 3 (September-November) and Quarter 4 (December-next year February). We hypothesized that new interns and new first year residents became more experienced and more skilled with passage of time. Therefore, Quarter 1 was the most unskilled period, whereas Quarter 4 was the most skilled period.
Admission month, demographic and clinical characteristics (age, sex and number of chronic conditions, such as diabetes, hypertension and chronic obstructive lung disease), treatment (length of stay, type of procedures performed) and outcome (in-hospital mortality and unfavorable discharge rates; which means worse discharge Glasgow coma scale (GCS) score than first admission GCS score) variables were obtained from the clinical records and radiographic studies of involved patients.
All retrieved data were converted into categorical or binominal variables. The statistical relationships were assessed using one-way analysis of variance (ANOVA), logistic regression analysis, multiple regression analysis and Cox regression analysis; and additional survival analysis was performed in order to examine the effect of admission quarter on unfavorable discharge and mortality rate of sSAH patients. Statistical significance was accepted for a p value of < 0.05.
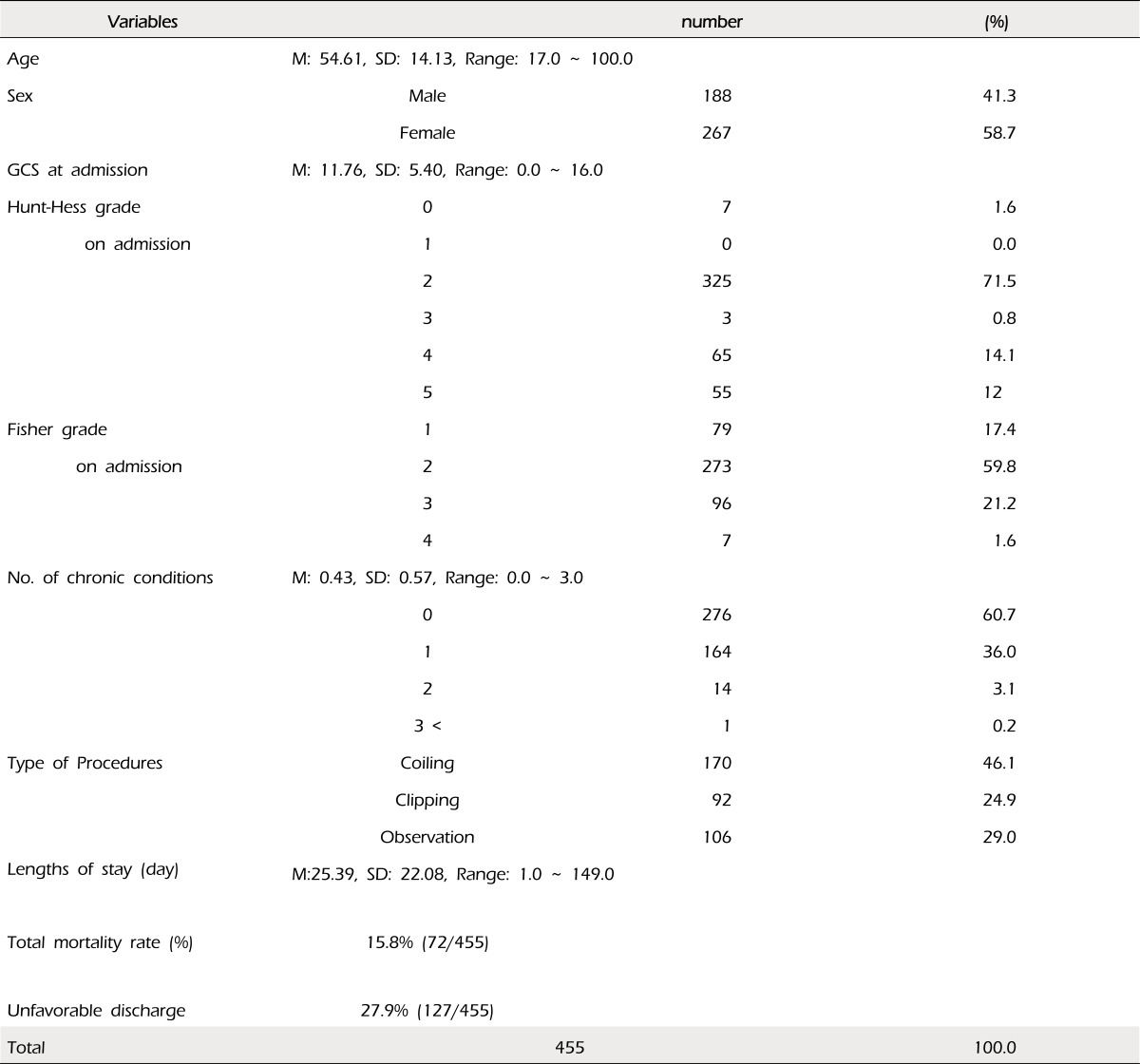
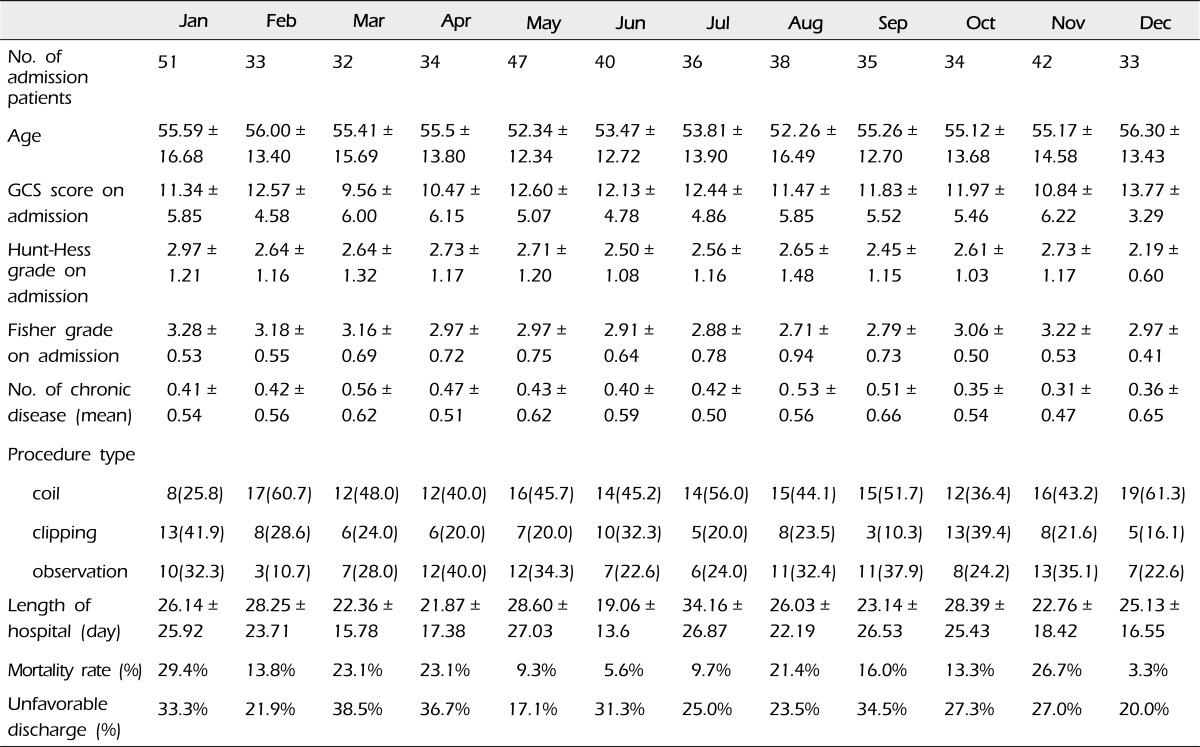
A total of 455 consecutive patients with sSAH between January 2008 and December 2010 were retrospectively enrolled in the present study. Their mean age was approximately 54 years (54.61) and sex ratio was approximately 4:6 (Male: Female = 41.3%: 58.7%). A summary of patients' clinical information is shown in Table 1 and more detailed information according to the admission month is shown in Table 2.
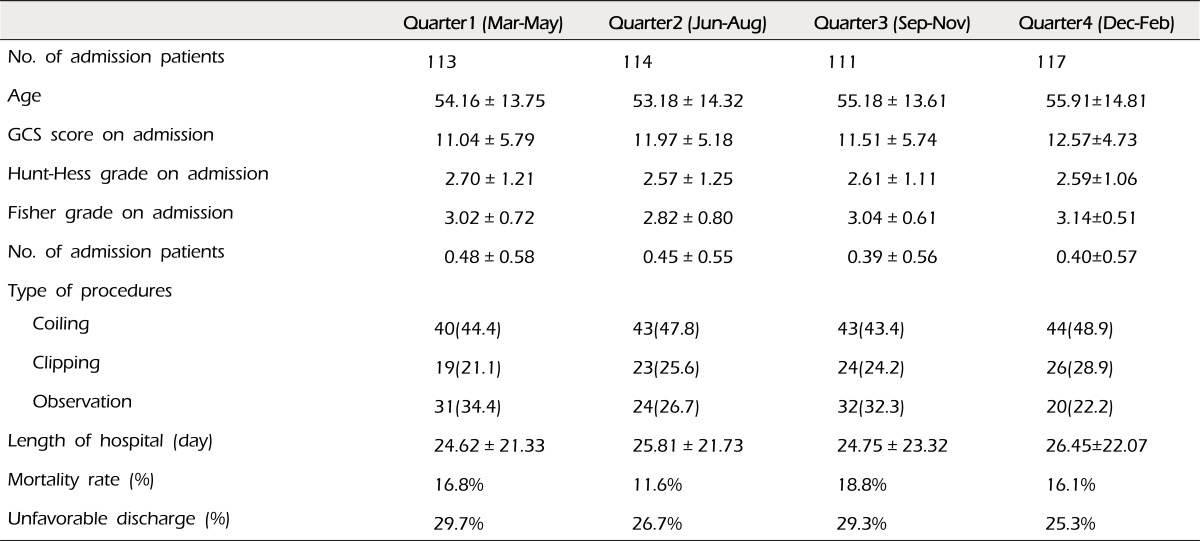
Four groups (quarter 1 to 4), divided according to their admission month, did not show statistically significant difference in their clinical characteristics, including age, Hunt-Hess and Fisher grades at admission and type of treatment procedures (Table 3).
Mortality rates of each quarter were 16.8% in quarter 1, 11.6% in quarter 2, 18.8% in quarter 3 and 16.1% in quarter 4 (Table 3, Fig. 1).
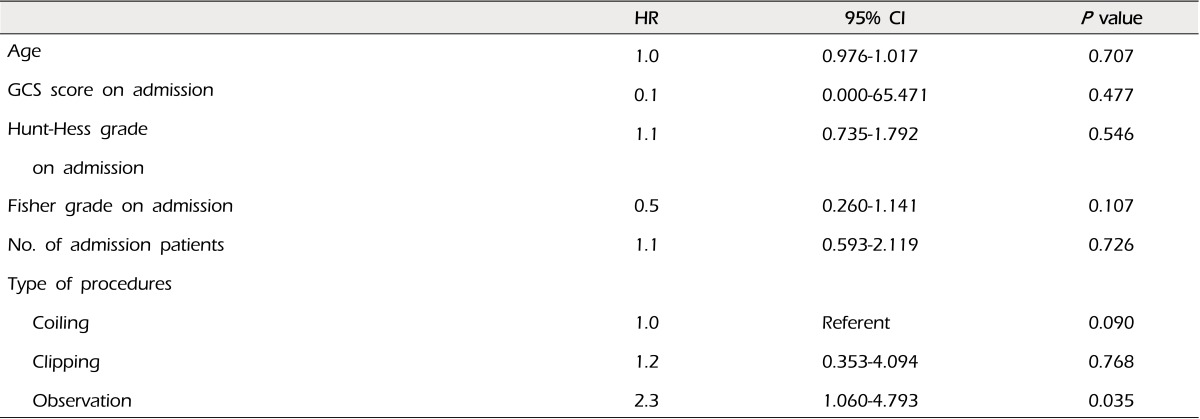
Through logistic regression analysis for identification of factors having an influence on patients' mortality rate, conservative therapy (Hazard Ratio [HR] = 2.3, p = 0.035) was the only statistically significant factor associated with mortality rate regardless of admission quarter. All other investigated clinical variables, including age (HR = 1.0, p = 0.707), admission GCS score (HR = 0.1, p = 0.477), Hunt-Hess grade at admission (HR = 1.1, p = 0.546), Fisher grade at admission (HR = 0.5, p = 0.107), mean number of chronic diseases (HR = 1.1, p = 0.726) and coiling procedure (HR = 1.0, p = 0.090) /surgical clipping (HR = 1.2, p = 0.768) did not show a statistically significantly association with mortality rate of the patients (Table 4).
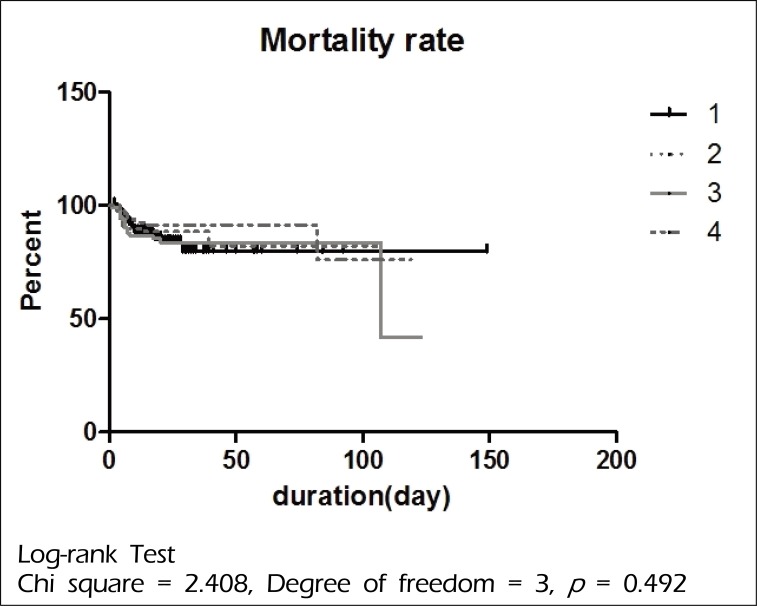
In additional log-rank analysis, no statistically significant difference in mortality rate was observed with respect to the admission quarter (Chi square = 2.408, degree of freedom [Df] = 3, p = 0.492) (Fig. 2).
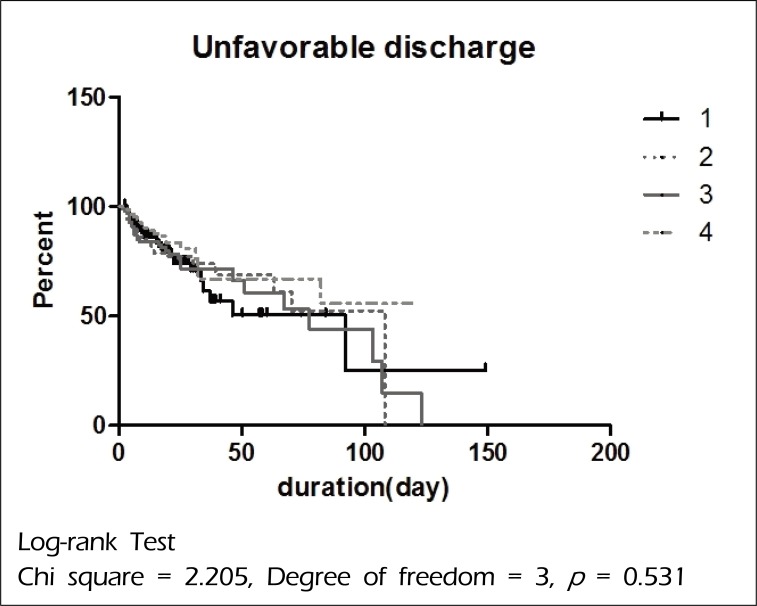
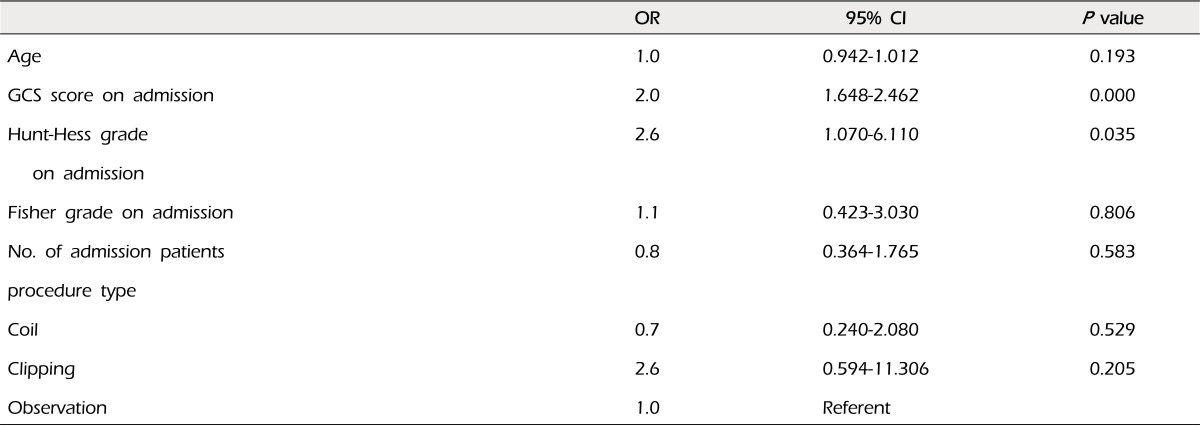
With the logistic regression analysis, admission GCS score (HR = 2.0, p = 0.000) and Hunt-Hess grade at admission (HR = 2.6, p = 0.035) showed a statistically significantly association with unfavorable discharge of patients (Table 5). In additional log-rank analysis, no statistically significant difference in the unfavorable discharge rate was observed with respect to the admission quarter (Chi square = 2.205, Df = 3, p = 0.531) (Fig. 3).
The 'July phenomenon or effect' in western countries (called a 'March effect' in our study) has been studied across different medical specialties, including general surgery, obstetrics and gynecology and internal medicine.2)4)5)8)10)14)18)20)21)27) Evidence of or against the presence of a 'July effect' has been inconsistent. The principal causes for discordance among published studies are likely a function of several phenomena. First, many of these studies derived their data from single-center populations and thus may more accurately reflect the clinical and educational practice patterns of a particular hospital. Second, smaller studies may have failed to normalize data on changes in seasonal practice patterns, which may falsely manifest as relative changes in outcomes. Third, as in our study, complete information regarding long-term outcomes and prognosis were not available in the database and thus could not be used as outcome metrics. Fourth, differing end points and adverse outcome metrics were used among the different studies, including ours, making inter-study comparisons difficult.
The majority of studies on the 'July effect' have found no meaningful difference in patient outcomes in July compared to other months. Buchwald et al.,7) who evaluated neck and back problems, found no increase in the length of hospital stay for July admissions, compared with May. Banco et al.,2) who focused on the incidence of perioperative spinal infection rates at different times during the academic year. They found no association between infection rates in the month of July or other times of the year when residents or fellows were new on the service.
On the other hand, some studies have demonstrated a 'July effect'. In a recent study, after examining all available US death certificates from 1979 to 2006, Phillips and Barker23) reported a 10% increase in fatal medical errors in the inpatient, outpatient and emergency room setting. Englesbe et al.11) reported an increase in postoperative mortality of 41% among patients treated by interns within the American College of Surgeons National Surgical Quality Improvement Program. One study reported a slight increase in overall surgical mortality during the years 1991 to 1997 at teaching hospitals.4) Walling and Veremakis28) reported that first-year residents made more prescribing errors during early months of their training compared with later in the year. In addition, Inaba et al.14) demonstrated an increased risk of errors resulting in preventable or potentially preventable complications at the beginning of the academic year (July and August) compared with the end of the academic year (May and June) at an academic trauma center.
To the best of the author's knowledge, no neurosurgical studies on the 'July effect (March effect)' have been conducted in Korea. In this retrospective, cohort study of 455 consecutive sSAH admissions, we found no statistically significant increase in the mortality or unfavorable discharge rate for the month of March in our hospital compared with all other months.
In the present study, there are several limitations. First, this study is a retrospective study, which has the potential for analytic limitations in some clinical variables and situations, such as medical errors and adverse events. Second, possible limitation is the risks inherent to emergency cases. Given the circumstances of the tertiary emergency room, there are a few potentials for misdiagnosis at admission, which may result in inaccurate mortality and/or unfavorable discharge rates. Third, there is another limitation of the retrospective study. We were not able to analyze the rates of complications and near misses that were not associated with mortality or unfavorable discharges, committed by neurosurgery interns and residents, especially during management in the intensive care unit, which may be a more sensitive tool for evaluation of a 'March effect'. Fourth, one of the limitations to this study is that our data are limited to in-hospital observations. Therefore, mortality occurring after discharge would not be assessed. However, because complications and medical errors, which resulted in death of the patients, committed by neurosurgery interns and residents are most likely going to be in-hospital and not after discharge, we believe that this should not have a significant effect on the result of our study. Fifth, the temporal resolution is limited to monthly intervals and fluctuations in adverse outcomes over time periods shorter than one month would not be detected in the current study, especially if the rotation schedules of interns are shorter than one month. And, finally, we did not consider the clinical experience of the surgeons performing surgical clipping and/or endovascular interventions in our hospital, which might be the most important factor influencing the patients' outcome. However, cases of each surgeon were evenly allocated over one year, which might not have an effect on the monthly variation of patients' outcome.
Generally speaking, it is reasonable to assume that at the start of an academic year, a number of errors made by interns and residents would be higher compared with later months. Alternatively, the absence of a "March effect (July effect)" may be attributable to the increased supervision by more senior residents and faculties during the start of the academic year.
Findings of our study suggest that the 'March effect' was not found for neurosurgical mortality or unfavorable discharge rates in patients with sSAH in the author's hospital. Even with some limitations, our study adds to the limited knowledge on the 'March effect' in the field of neurosurgery. In order to establish a 'March effect' in the neurosurgical field, including sSAH, a meta-analysis from multi-institutional prospective study is anticipated.
References
1. Aylin P, Majeed FA. The killing season-fact or fiction. BMJ. 1994; 12. 309(6970):1690. PMID: 7819988.

2. Banco SP, Vaccaro AR, Blam O, Eck JC, Cotler JM, Hilibrand AS, et al. Spine infections: variations in incidence during the academic year. Spine (Phila Pa 1976). 2002; 5. 27(9):962–965. PMID: 11979171.
3. Barger LK, Cade BE, Ayas NT, Cronin JW, Rosner B, Speizer FE, et al. Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med. 2005; 1. 352(2):125–134. PMID: 15647575.

4. Barry WA, Rosenthal GE. Is there a July phenomenon? The effect of July admissions on intensive care morality and length of stay in teaching hospitals. J Gen Intern Med. 2003; 8. 18(8):639–645. PMID: 12911646.
5. Bederson JB, Connolly ES Jr, Batjer HH, Dacey RG, Dion JE, Diringer MN, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke. 2009; 3. 40(3):994–1025. PMID: 19164800.

6. Blumberg MS. Measuring surgical quality in Maryland: a model. Health Aff (Millwood). 1988; 2. 7(1):62–78. PMID: 3360395.

7. Buchwald D, Komaroff AL, Cook EF, Epstein AM. Indirect costs for medical education. Is there a July phenomenon? Arch Intern Med. 1989; 4. 149(4):765–768. PMID: 2495778.

8. Claridge JA, Schulman AM, Sawyer RG, Ghezel-Ayagh A, Young JS. The 'July phenomenon' and the care of the severely injured patient: fact or fiction? Surgery. 2001; 8. 130(2):346–353. PMID: 11490370.

9. Davydov L, Caliendo G, Mehl B, Smith LG. Investigation of correlation between house-staff work hours and prescribing errors. Am J Health Syst Pharm. 2004; 6. 61(11):1130–1134. PMID: 15237565.

10. Diringer MN. Management of aneurysmal subarachnoid hemorrhage. Crit Care Med. 2009; 2. 37(2):432–440. PMID: 19114880.

11. Englesbe MJ, Pelletier SJ, Magee JC, Gauger P, Schifftner T, Henderson WG, et al. Seasonal variation in surgical outcomes as measured by the American College of Surgeons-National Surgical Quality Improvement Program (ACS-NSQIP). Ann Surg. 2007; 9. 246(3):456–462. discussion 463-5. PMID: 17717449.

12. Finkielman JD, Moreles J, Peters SG, Keegan MT, Ensminger SA, Lymp JF, et al. Mortality rate and length of stay of patients admitted to the intensive care unit in July. Crit Care Med. 2004; 5. 32(5):1161–1165. PMID: 15190967.

13. Friedman WA. Resident duty hours in American neurosurgery. Neurosurgery. 2004; 4. 54(4):925–931. discussion 931-3. PMID: 15046659.

14. Inaba K, Recinos G, Teixeira PG, Barmparas G, Talving P, Salim A, et al. Complications and death at the start of the new academic year: is there a July phenomenon? J Trauma. 2010; 1. 68(1):19–22. PMID: 20065752.

15. Kestle JR, Cochrane DD, Drake JM. Shunt insertion in the summer: is it safe? J Neurosurg. 2006; 9. 105(3 Suppl):165–168. PMID: 16970227.

16. Kowalski RG, Claassen J, Kreiter KT, Bates JE, Ostapkovich ND, Connolly ES, et al. Initial misdiagnosis and outcome after subarachnoid hemorrhage. JAMA. 2004; 2. 291(7):866–869. PMID: 14970066.

17. Kraus JJ, Metzler MD, Coplin WM. Critical care issues in stroke and subarachnoid hemorrhage. Neurol Res. 2002; 24(Suppl 1):S47–S57. PMID: 12074437.

18. Landrigan CP, Rothschild JM, Cronin JW, Kaushal R, Burdick E, Katz JT, et al. Effect of reducing interns' work hours on serious medical errors in intensive care units. N Engl J Med. 2004; 10. 351(18):1838–1848. PMID: 15509817.

19. Lockley SW, Cronin JW, Evans EE, Cade BE, Lee CJ, Landrigan CP, et al. Effect of reducing interns' weekly work hours on sleep and attentional failures. N Engl J Med. 2004; 10. 351(18):1829–1837. PMID: 15509816.

20. McDonald RJ, Cloft HJ, Kallmes DF. Impact of admission month and hospital teaching status on outcomes in subarachnoid hemorrhage: evidence against the July effect. J neurosurg. 2012; 1. 116(1):157–163. PMID: 21942725.

21. Myles TD. Is there an obstetric July phenomenon? Obstet Gynecol. 2003; 11. 102(5 pt 1):1080–1084. PMID: 14672490.

22. Pape HC, Pfeifer R. Restricted duty hours for surgeons and impact on residents quality of life, education and patient care: a literature review. Patient Saf Surg. 2009; 2. 3(1):3. PMID: 19232105.

23. Phillips DP, Barker GE. A July spike in fatal medication errors - a possible effect of new medical residents. J Gen Intern Med. 2010; 8. 25(8):774–779. PMID: 20512532.
24. Rich EC, Gifford G, Luxenberg M, Dowd B. The relationship of house staff experience to the cost and quality of inpatient care. JAMA. 1990; 2. 263(7):953–957. PMID: 2299762.

25. Rich ED, Hillson SD, Dowd B, Morris N. Specialty differences in the "July Phenomenon" for Twin Cities teaching hospitals. Med Care. 1993; 1. 31(1):73–83. PMID: 8417272.

26. Shulkin DJ. The July phenomenon revisited : are hospital complications associated with new house staff? Am J Med Qual. 1995; Spring. 10(1):14–17. PMID: 7727983.
27. Smith ER, Bulter WE, Barker FG 2nd. Is there a "July phenomenon" in pediatric neurosurgery at teaching hospitals? J Neurosurg. 2006; 9. 105(3 Suppl):169–176. PMID: 16970228.

28. Walling HW, Veremakis C. Ordering errors by first-year residents: evidence of learning from mistakes. Mo Med. 2004; Mar-Apr. 101(2):128–131. PMID: 15119112.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download