Abstract
Objective
Keyhole craniotomy is a modification of pterional craniotomy that allows for use of a minimally invasive approach toward cerebral aneurysms. Currently, mini-pterional (MPKC) and supraorbital keyhole craniotomies (SOKC) are commonly used. In this study, we measured and compared the geometric configurations of surgical exposure provided by MPKC and SOKC.
Methods
Nine patients underwent MPKC and four underwent SOKC. Their postoperative contrast-enhanced brain computed tomographic scans were evaluated. The transverse and longitudinal diameters and areas of exposure were measured. The locations of the anterior communicating artery, bifurcation of the middle cerebral artery (MCAB), and the internal carotid artery (ICA) terminal were identified, and the working angles and depths for these targets were measured.
Results
No significant differences in the transverse diameters of exposure were observed between MPKC and SOKC. However, the longitudinal diameters and the areas were significantly larger, by 1.5 times in MPKC. MPKC provided larger operable working angles for the targets. The angles by MPKC, particularly for the MCAB, reached up to 1.9-fold of those by SOKC. Greater working depths were required in order to reach the targets by SOKC, and the differences were the greatest in the MCAB by 1.6-fold.
Conclusion
MPKC provides larger exposure than SOKC with a similar length of skin incision. MPKC allows for use of a direct transsylvian approach, and exposes the target in a wide working angle within a short distance. Despite some limitations in exposure, SOKC is suitable for a direct subfrontal approach, and provides a more anteromedial and basal view. MCAB and posteriorly directing ICA terminal aneurysms can be good candidates for MPKC.
Since the introduction of frontotemporal craniotomy by Yaşargil et al, so-called "pterional craniotomy" (PC) has traditionally been regarded as a standard approach for clipping of cerebral aneurysms in the anterior circulation.17-19) Because the PC provides an optimal microscopic exposure and a wide open working space for manipulation of intracranial structures, it had ultimately been regarded as a gold standard method for treatment of cerebral aneurysms until the introduction of endovascular coiling. There is no doubt that surgical clipping of a cerebral aneurysm is the best treatment option in the aspect of complete obliteration with the least chance of recurrence. However, as endovascular coiling has gained popularity because of its less invasiveness and shorter operation time, even with its incomplete outcome, the role of surgical clipping has gradually diminished over the past 15 years.10)
With advancement in microscopic techniques and instrumentation, many surgical modifications have been added to the traditional PC in order to simplify the process.1)5-8)10)14)15) The keyhole craniotomy is a novel modification of the PC that allows for use of a minimally invasive approach toward cerebral aneurysms, dramatically minimizes iatrogenic trauma to normal tissues, and still enables complete obliteration of the aneurysm.3)5-8)10)11)14)15) Currently, the mini-pterional keyhole craniotomy (MPKC) and the supraorbital keyhole craniotomy (SOKC) are commonly used.1)5)6)10)11)14)15) However, significant controversy exists with regard to the following questions: is it safe?, is it always possible to reach the target?, is the cosmetic result superior to that of the standard PC from the patient's aspect?, can it be used for treatment of all aneurysms?, and so forth.
To the best of our knowledge, there have been some reports comparing one of the previously mentioned keyhole craniotomies and the standard PC, however, none have compared the MPKC and SOKC and described their different indications.3)6)11) In this study, we measured the geometric configurations of surgical exposure provided by the MPKC and SOKC, and compared the results in order to establish the surgical indications of each keyhole craniotomy.
Thirteen patients (four males and nine females) with 15 aneurysms underwent keyhole craniotomies at our institute in 2012. They were assigned to two groups, MPKC (n = 9) and SOKC groups (n = 4). Their surgical decisions were made by preoperative simulation using computed tomographic (CT) angiography or conventional angiography with three-dimensional reconstruction.
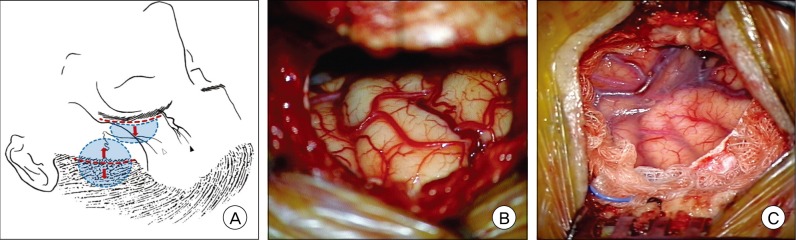
Contrast-enhanced brain CT scans with three-dimensional reconstruction were obtained one week after the operation, and were evaluated retrospectively. The transverse and longitudinal diameters of surgical exposure by the craniotomies were measured, and the areas of exposure were calculated automatically by drawing the outlines of the craniotomies using the picture archiving and communication system program (PACS pia, Information & Communication Management Inc., Seoul, Korea). The locations of the anterior communicating artery (ACoA), bifurcation of the middle cerebral artery (MCAB), and the internal carotid artery (ICA) terminal were identified in each patient; these points were regarded as the targets. Then, a cross section involving one of these three targets and the transverse line of the craniotomy was made using Rapidia (Rapidia 2.8, Infinitt Healthcare, Seoul, Korea), thereby acquiring three different planes for each patient. On each plane, two lines were drawn from both edges of the craniotomy to the target. The angle between the two lines was measured and it was defined as a microscopically operable working angle. The median line from the target to the outer table of the craniotomy was drawn, and it was named a trajectory line. The length of this line was measured, and it was named a working depth (Fig. 1A, 1B, and 1C).
All acquired data were recorded, and statistical analyses were performed using SPSS version 20.0 (SPSS Inc., Chicago, IL). For comparison of the MPKC and SOKC groups, a student t-test was performed for these parametric variables such as the transverse and longitudinal diameter and the area of exposure, and the operable working angle and depth for the ACoA, MCAB, and ICA terminal. In all cases, p values of less than 0.05 were considered statistically significant.
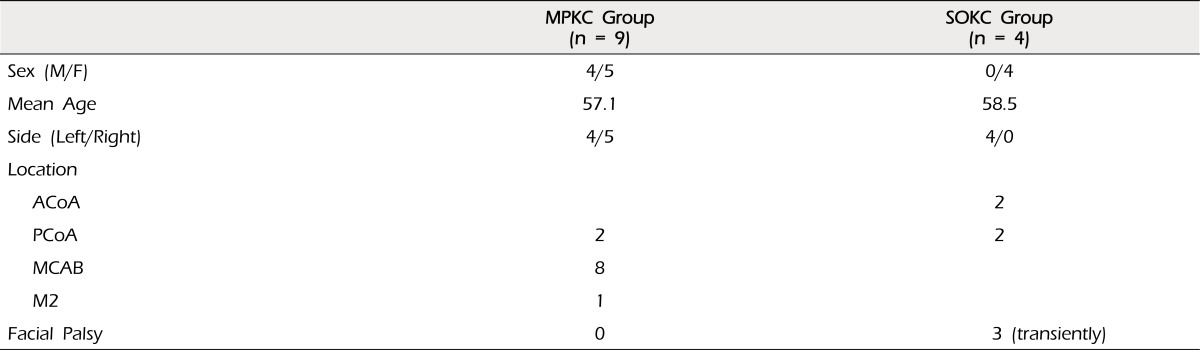
In the MPKC group, nine patients (four males and five females, mean age of 57.1 years) with 11 aneurysms were enrolled. Of these, two aneurysms were located in the posterior communicating artery; eight in the MCAB; and one in the M2 segment of the middle cerebral artery (MCA). In the SOKC group, four patients (all females, mean age of 58.5 years) with four aneurysms were enrolled. Two aneurysms were located in the ACoA, and two in the posterior communicating artery. All of the aneurysms were unruptured, and were treated successfully without occurrence of major complications, although there were three cases of transient mild facial palsy in the SOKC group, which were resolved within two months (Table 1).
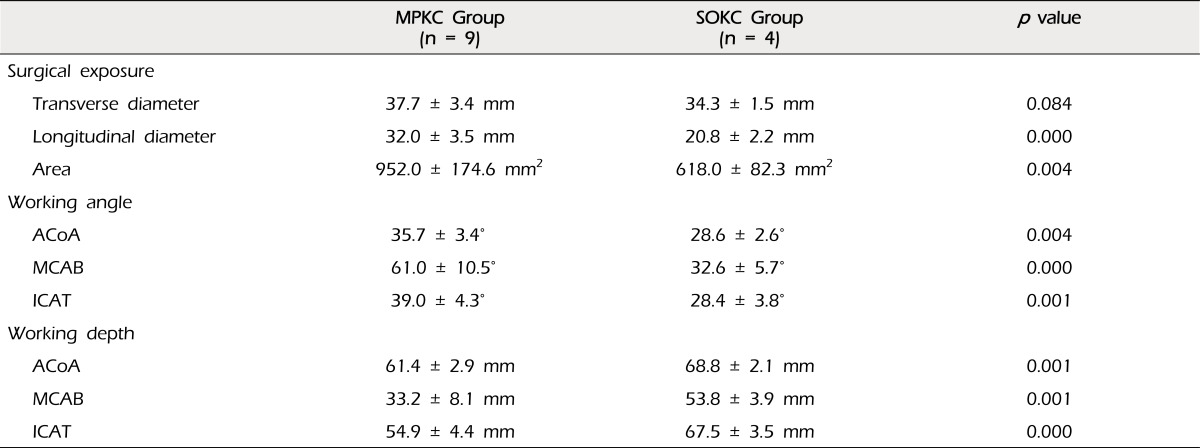
The mean transverse diameter of the surgical exposure by the craniotomies was 37.7 ± 3.4 mm for the MPKC group and 34.3 ± 1.5 mm for the SOKC group, which was not statistically different (p = 0.084). However, significant differences (p = 0.000) were observed in the longitudinal diameters (MPKC: 32.0 ± 3.5 mm, SOKC: 20.8 ± 2.2 mm), where the MPKC provided longitudinal diameters of craniotomy that were 1.5 times larger than those for the SOKC. Likewise, the mean areas of exposure by the MPKC (952.0 ± 174.6 mm2) were 1.5 times larger than those by the SOKC (618.0 ± 82.3 mm2) (p = 0.004). The MPKC also provided a significantly larger range of microscopically operable working angles for the ACoA, MCAB, and ICA terminal than the SOKC, and the difference was statistically significant (p = 0.004, p = 0.000, p = 0.001). In particular, the greatest differences in working angles were observed in the MCAB, where the angles by the MPKC reached up to 1.9-fold of those by the SOKC. The least differences were seen in the ACoA, where the angles by the MPKC were still 1.2 times larger than those by the SOKC. In addition, significantly greater working depths were required in order to reach these targets by the SOKC, compared with the MPKC (p = 0.001, p = 0.001, p = 0.000), and the differences were the greatest in the MCAB by 1.6-fold, and the least in the ACoA by 1.1-fold (Table 2).
Since introduction of the PC, it has been widely used in the field of neurosurgery for treatment of lesions in the anterior and posterior circulations.14-17) Even with development of endovascular coiling, due to its versatility, the PC is still the most important primary surgical option for treatment of aneurysms. The wide surgical corridor for the target lesion, which utilizes a variety of ranges of microscopic angles, is the main advantage of the PC.3) However, it requires a large scalp incision and temporalis dissection, which can cause facial nerve injury. Creation of a large bone flap may result in poor cosmetic outcomes, such as keyhole site depressions and the hollows of multiple burr hole sites.2)4)8)9)11)17)
Recently, the idea of minimizing unnecessary exposure and utilizing only the core surgical corridor has brought the minimally invasive surgical concept into practice in the neurosurgical field.15) The keyhole surgery has gained popularity with the belief that it would reduce the invasive nature of the PC but still ensure the complete obliteration of the aneurysm and the durability by clipping, which is regarded as a weak point of endovascular coiling. Perneczky et al. advocated the keyhole concept in neurosurgery using the SOKC in treatment of a variety of brain lesions.3)11)15) Nathal et al. described the sphenoid ridge keyhole approach, namely the MPKC, which is centered over the sylvian fissure.10) These two techniques are currently the most commonly used keyhole surgeries.
However, as the keyhole surgery gains remarkable popularity and notable attention, one may have a misbelief that the keyhole surgery is a simple and convenient operation. In fact, it is stressful for a surgeon to create a craniotomy with an appropriate size in a small skin incision, to work in a narrow surgical field, and to repair the skin without leaving a significant scar. Another misbelief is that a single method of the keyhole surgery is sufficient for treatment of nearly all aneurysms at different locations, replacing the role of the traditional PC or endovascular coiling. However, a keyhole surgery cannot be adopted as a primary standard approach, and one technique is not always the best option for reaching different targets.6)10)11) Different types of keyhole surgery offer different surgical fields and working angles. In order to determine the most suitable approach that provides the best surgical window for each different target, it is important to be aware of the limitations of each type of keyhole surgery.
The SOKC is basically a subfrontal approach. The range of the craniotomy size is limited by several anatomical structures.15) The medial extension is limited by the supraorbital artery and nerve, the frontal sinus, and the olfactory nerve. The lateral extension is enabled by drilling of the sphenoid ridge along with dissection of the temporalis muscle, but is still limited due to inevitable scarring. Even a tiny scar in the forehead may cause stress to a patient, whereas a larger scar behind the hairline is often neglected because it is rarely seen. The inferior extension is enabled in a small range by drilling the orbital convolutions. According to our study, the SOKC provides a limited longitudinal exposure, because downward skin retraction is limited by the orbit and only the upward retraction is used to expose the skull, thereby creating a semilunar craniotomy. However, the upward skin retraction is still limited by the risk of injury to the frontal branch of the facial nerve.12) In the current study, three patients in the SOKC group suffered from transient facial nerve palsies, and this may be related to an excessive upward skin retraction. The limited area of exposure is related primarily to the narrow longitudinal exposure, whereas the transverse exposure is nearly the same as that of the MPKC. Therefore, the SOKC allows for a similar length of the transverse exposure by a similar length of the skin incision, as in the MPKC, but a smaller area of exposure with the limited longitudinal exposure mainly from the limitation of the skin retraction (Fig. 2A and 2B). The MPKC allows for direct visualization of the sylvian fissure.8)10) There are no significant anatomical barriers that limit the size of the craniotomy.6) The skin incision is always behind the temporal hairline, which may relieve the fear from scarring. The risk of injury to the facial nerve is very low, as in the current study. Bilateral upward and downward skin retractions enable significantly larger longitudinal exposure with the same size of skin incision, as in the SOKC (Fig. 2A and 2C).
Because the SOKC is fundamentally a subfrontal approach, it offers a more anteromedial and basal view than the classical PC or the MPKC.10) The approach toward the ACoA is straightforward and the trajectory line toward the target is a right angle to the craniotomy. These conditions make the ACoA aneurysm a good candidate for the SOKC. Even though our study confirmed that the working angles and the depths for the ACoA supplied by the SOKC were slightly inferior to those by the MPKC (80.1% and 112% of MPKC respectively), the differences were the least when compared with the results for other targets. On the other hand, access to the ACoA using the MPKC appears to be less favorable than that of the SOKC because the MPKC was basically developed for a transsylvian approach. More longitudinal exposure toward the skull base is required in order to allow for use of a direct subfrontal approach, and this can be feasible with an anterior extension of the skin incision along the forehead wrinkle, however, we prefer to use this technique only when the ACoA aneurysm is accompanied by an MCAB aneurysm.
The approach toward the terminal of the ICA is not always favorable by the SOKC. Because the SOKC offers an anteromedial subfrontal corridor, the laterally directing ICA terminal aneurysm can be a good candidate for the SOKC. However, in cases of posteriorly directing ICA terminal aneurysms, visualization of the aneurysmal neck and the origin of the incorporated branch is not optimal. This problem has already been emphasized by many authors.8)10)11)15) Neither mobilization of the parent artery nor modification of the microscopic working angle is possible in the narrow and deep surgical corridor obtained by the SOKC. Utilizing endoscopy can be a solution in some cases, however, the instrument is bulky and the process is time-consuming, which may minimize the advantage of the keyhole surgery over the standard PC.10)11)15) In addition, blind clipping of the aneurysmal neck is still often required and, in many cases, endoscopy can only confirm the result of clipping. In performance of the blind procedure, there may be a risk of leaving a remnant at any time, and it may undermine the superiority of clipping over endovascular coiling in terms of complete obliteration. The MPKC is a good surgical alternative to the SOKC when treating posteriorly directing ICA terminal aneurysms.10) It enables direct visualization of the aneurysm and the adjacent branches, and the surgical field can be additionally extended by the proximal sylvian dissection. The current study also demonstrated superior working angles and depths by the MPKC to those by the SOKC.
The main limitations of the SOKC are found when treating the MCA aneurysm. Several previous reports have described these limitations.8)10)11) Our study confirmed that the working angles and the depths for the MCAB obtained by the SOKC were remarkably inferior to those by the MPKC (53.3% and 162% of MPKC respectively) with the greatest differences when compared with the results for other targets. The trajectory line from the craniotomy window toward the MCAB is far laterally deviated, and it becomes even worse if the M1 segment is too long. This distorted surgical view is responsible for the narrow working angle (Fig. 1B). The sylvian dissection may sometimes be difficult even with the standard PC when tight adhesion between the frontal and temporal lobe is encountered or the sylvian fissure is too much posteriorly deviated, and the dissection with the suboptimal visualization of the sylvian fissure by the SOKC may be more difficult. Therefore, technical limitations may exist, and it may carry a potential risk. In contrast, the MCAB aneurysm is the best candidate for the MPKC. The MPKC provides a wide surgical window and the shortest distance to reach the target. The corridor is straightforward from the craniotomy (Fig. 1A). It exposes both the frontal and temporal lobes, and there exists sufficient space for utilization of brain retractors in cases of difficult sylvian dissection. Because the surgical field is wide and the working view is similar to those by the standard PC, this approach has fewer technical limitations than the SOKC.10)
One of the most important goals of keyhole surgery is minimizing unnecessary brain exposure by creating a more specific and tailored craniotomy, and shortening the operation time is secondary. Aneurysm clipping by keyhole craniotomy is still one of the open surgeries, and the advantages of open surgery over endovascular surgery are the superior obliteration rate and durability of the treatment. Therefore, neurosurgeons should make every effort to occlude the aneurysm completely rather than to speed up in haste and leave remnants. The indications for keyhole surgery when treating a cerebral aneurysm are not determined just by the size of aneurysm, but the configuration of the aneurysmal neck. An aneurysm with a simple neck is a good indication for keyhole surgery. An aneurysm with a broad neck can also be a feasible candidate if the neck is not too complex and can be easily visualized in a narrow operable working angle. To determine whether the neck can be visualized at a good surgical angle, preoperative simulation is necessary using CT angiography or conventional angiography with three-dimensional reconstruction, and it is certainly helpful in determination of the feasibility of keyhole surgery.15) With development of different types of keyhole surgeries, we should not rely only on one type of technique. Neurosurgeons must be aware of the advantages and disadvantages of each keyhole surgery, and the most appropriate approach should be chosen according to the location and the direction of the aneurysm. The success of the keyhole surgery truly relies on proper patient selection.
The MPKC offers a larger surgical exposure than the SOKC even with the similar length of the skin incision. The MPKC provides a direct sylvian approach, and exposes the target in a wide operable working angle within a short distance. The SOKC is suitable for a direct subfrontal approach, and provides a more anteromedial and basal view despite some limitations of the working angle and depth. MCAB aneurysms and posteriorly directing ICA terminal aneurysms are good candidates for the MPKC, and ACoA aneurysms and laterally directing ICA terminal aneurysms are good candidates for the SOKC. Keyhole surgery can be a safe and effective treatment modality for treatment of a cerebral aneurysm when the most suitable approach is selected based on the location and the direction of the aneurysm. Further detailed comparative analyses with a large series of patients may be helpful in determination of more specific indications of each keyhole surgery.
References
1. Andaluz N, Romano A, Reddy LV, Zuccarello M. Eyelid approach to the anterior cranial base. J Neurosurg. 2008; 8. 109(2):341–346. PMID: 18671651.

2. Badie B. Cosmetic reconstruction of temporal defect following pterional [corrected] craniotomy. Surg Neurol. 1996; 4. 45(4):383–384. PMID: 8607091.
3. Chalouhi N, Jabbour P, Ibrahim I, Starke RM, Younes P, El Hage G, et al. Surgical treatment of ruptured anterior circulation aneurysms: comparison of pterional and supraorbital keyhole approaches. Neurosurgery. 2013; 3. 72(3):437–442. PMID: 23208062.
4. Coscarella E, Vishteh AG, Spetzler RF, Seoane E, Zabramski JM. Subfascial and submuscular methods of temporal muscle dissection and their relationship to the frontal branch of the facial nerve. Technical note. J Neurosurg. 2000; 5. 92(5):877–880. PMID: 10794306.
5. Dare AO, Landi MK, Lopes DK, Grand W. Eyebrow incision for combined orbital osteotomy and supraorbital minicraniotomy: application to aneurysms of the anterior circulation. Technical note. J Neurosurg. 2001; 10. 95(4):714–718. PMID: 11596969.
6. Figueiredo EG, Deshmukh P, Nakaji P, Crusius MU, Crawford N, Spetzler RF, et al. The minipterional craniotomy: technical description and anatomic assessment. Neurosurgery. 2007; 11. 61(5 Suppl 2):256–264. discussion 264-5. PMID: 18091240.

7. Jallo GI, Suk I, Bognár L. A superciliary approach for anterior cranial fossa lesions in children. Technical note. J Neurosurg. 2005; 7. 103(1 Suppl):88–93. PMID: 16122012.
8. Kil JS, Kim DW, Kang SD. Navigation-guided keyhole approach for unruptured intracranial aneurysms. Korean J Cerebrovasc Surg. 2011; 9. 13(3):244–248.
9. Lee MS, Lee YS, Lee JH, Ryu KY, Kang DG. The efficacy of temporal mesh plate floating technique for keyhole site depression after frontotemporal craniotomy. J Korean Neurotraumatol Soc. 2011; 7:78–82.

10. Nathal E, Gomez-Amador JL. Anatomic and surgical basis of the sphenoid ridge keyhole approach for cerebral aneurysms. Neurosurgery. 2005; 1. 56(1 Suppl):178–185. discussion 178-85. PMID: 15799808.

11. Park HS, Park SK, Han YM. Microsurgical experience with supraorbital keyhole operations on anterior circulation aneurysms. J Korean Neurosurg Soc. 2009; 8. 46(2):103–108. PMID: 19763211.

12. Reisch R, Perneczky A. Ten-year experience with the supraorbital subfrontal approach through an eyebrow skin incision. Neurosurgery. 2005; 10. 57(4 Suppl):242–255. discussion 242-55. PMID: 16234671.

13. Renowden SA, Benes V, Bradley M, Molyneux AJ. Detachable coil embolisation of ruptured intracranial aneurysms: a single center study, a decade experience. Clin Neurol Neurosurg. 2009; 2. 111(2):179–188. PMID: 19013012.

14. Sánchez-Vázquez MA, Barrera-Calatayud P, Mejia-Villela M, Palma-Silva JF, Juan-Carachure I, Gomez-Aguilar JM, et al. Transciliary subfrontal craniotomy for anterior skull base lesions. Technical note. J Neurosurg. 1999; 11. 91(5):892–896. PMID: 10541254.
15. van Lindert E, Perneczky A, Fries G, Pierangeli E. The supraorbital keyhole approach to supratentorial aneurysms: concept and technique. Surg Neurol. 1998; 5. 49(5):481–489. discussion 489-90. PMID: 9586924.

16. Yaşargil MG, Antic J, Laciga R, Jain KK, Hodosh RM, Smith RD. Microsurgical pterional approach to aneurysms of the basilar bifurcation. Surg Neurol. 1976; 8. 6(2):83–91. PMID: 951657.
17. Yaşargil MG, Boehm WB, Ho RE. Microsurgical treatment of cerebral aneurysms at the bifurcation of the internal carotid artery. Acta Neurochir (Wien). 1978; 41(1-3):61–72. PMID: 665339.

18. Yaşargil MG, Fox JL. The microsurgical approach to intracranial aneurysms. Surg Neurol. 1975; 1. 3(1):7–14. PMID: 1111150.
19. Yaşargil MG, Reichman MV, Kubik S. Preservation of the frontotemporal branch of the facial nerve using the interfascial temporalis flap for pterional craniotomy. Technical article. J Neurosurg. 1987; 9. 67(3):463–466. PMID: 3612281.
Fig. 1
The illustration depicts the microscopically operable working angles for the anterior communicating artery, the terminal of the internal carotid artery, and the bifurcation of the middle cerebral artery when approached by the mini-pterional keyhole craniotomy (A) and the supraorbital keyhole craniotomy (B). The simplified diagram (C) describes the working angle (black arrow) and the trajectory line (asterisk). The working depth refers to the length of the trajectory line. The black arrow head indicates a half angle of the working angle.

Fig. 2
The illustration (A) shows the different locations of the skin incision (red dotted line), size and shape of the bone flap (blue dotted line and area), and direction of skin retraction (red arrows) for the supraorbital keyhole craniotomy (SOKC) and the mini-pterional keyhole craniotomy (MPKC). The courses of the supraorbital nerve and artery (black arrow head) and the frontal branches of the facial nerve (white arrow head) are shown. Intraoperative photographs show the area of surgical exposure created by the SOKC (B) and MPKC (C). Note that the basal frontal lobe is exposed by the semilunar SOKC using only upward skin retraction, whereas the sylvian fissure is directly exposed by the MPKC using bilateral skin retraction.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download