This article has been
cited by other articles in ScienceCentral.
Abstract
Distal embolization resulting from carotid angioplasty and stenting (CAS) occurs mainly in the cerebral hemisphere. We report a case of ophthalmic artery occlusion after carotid revascularization. A 75-year old man received emergency CAS for cervical internal carotid artery occlusion. Two months later, the patient was readmitted for decreased visual acuity. We found ophthalmic artery occlusion that was not noticed soon after CAS. Although ophthalmic artery occlusion after CAS is rare, endovascular neurosurgeons should be aware of this potential complication.
Go to :

Keywords: Carotid angioplasty and stenting, Embolization, Ophthalmic artery occlusion
INTRODUCTION
Carotid angioplasty and stenting (CAS) has become an alternative option to carotid endarterectomy (CEA) for treatment of carotid artery stenosis. The Carotid Revascularization Endarterectomy versus Stenting Trial (CREST) supported this alternative treatment option although the periprocedural stroke rate was higher in the stenting group.
3) Distal embolization of plaque fragments raises concerns regarding the safety of CAS. Whereas distal embolization resulting from CAS usually occurs in the cerebral hemisphere, it sometimes develops as central or branch retinal artery occlusion (CRAO or BRAO).
8)11-
13) However, there have been no reports of ophthalmic artery occlusion. We describe a rare case of ophthalmic artery occlusion resulting from carotid revascularization.
Go to :

CASE REPORT
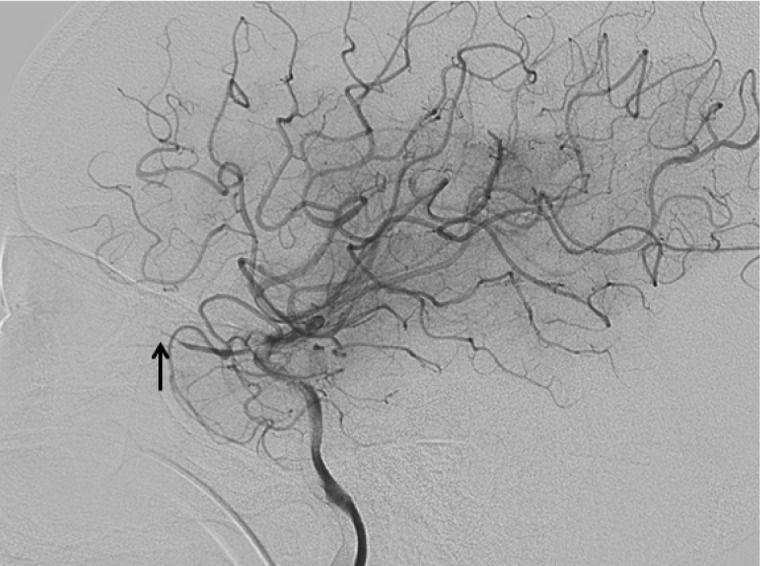
A 75-year old man with right hemiparesis and motor aphasia visited our emergency department. Symptom duration was three hours. He had hypertension for which he had been under treatment for ten years. No hemorrhagic lesions or low density areas were revealed by brain computerized tomography. A right internal carotid artery (ICA) angiogram showed collateral circulation to the anterior cerebral artery (ACA) and the middle cerebral artery (MCA) via anterior communicating artery and leptomeningeal anastomoses (
Fig. 1). The left ICA bifurcation was filled with thrombus (
Fig. 1). A left common carotid artery (CCA) angiogram revealed left proximal cervical ICA occlusion (
Fig. 2). The patient underwent CAS. After insertion of an 8 Fr sheath, an 8 Fr guiding catheter (FAS; Boston Scientific, Natick, MA, USA) was introduced into the left CCA. A 4×20 mm balloon (Ultra-soft SV; Boston Scientific, Natick, MA, USA) was used for pre-dilatation followed by stent implantation using an 8×40 mm carotid stent (Acculink; Abbott Vascular, Abbott Park, IL, USA) (
Fig. 3). After CAS, the thrombus in distal ICA was removed using the Penumbra aspiration system (Penumbra, Inc., Alameda, CA, USA). Final angiography showed flow restoration in the occluded segment (
Fig. 4). After the procedure, the right hemiparesis and motor aphasia improved. The patient was transferred to a hospital near his home.
 | Fig. 1Right internal carotid artery (ICA) angiogram showing collateral circulation to left anterior cerebral artery (ACA) via anterior communicating artery and to middle cerebral artery territory via leptomenigeal anastomosis from ACA. The arrow indicates thrombus at left ICA bifurcation. 
|
 | Fig. 2Left common carotid artery (CCA) angiogram reveals left proximal cervical ICA occlusion. 
|
 | Fig. 3Left CCA angiogram shows good dilatation of the left proximal cervical ICA after carotid angioplasty and stenting (CAS). 
|
 | Fig. 4Cerebral angiogram shows flow restoration in the left middle cerebral artery after thrombus aspiration. 
|
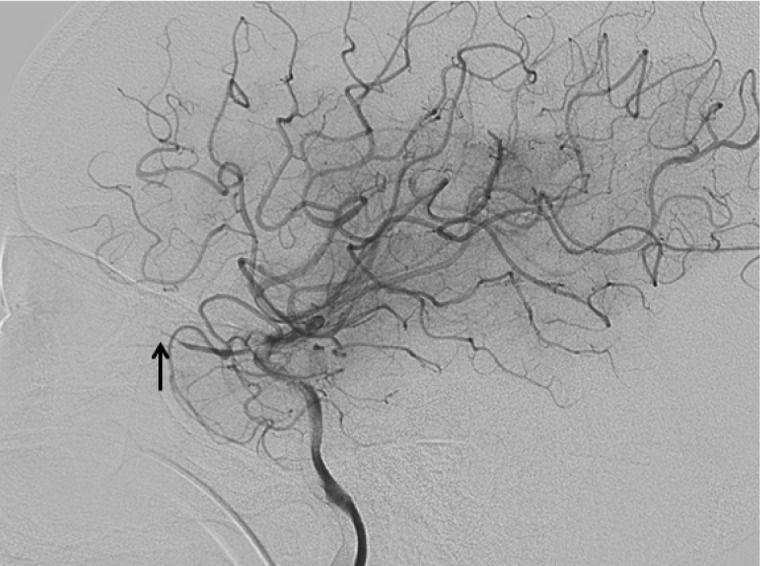
Two months later, the patient visited our ophthalmology department for decreased visual acuity. A careful interview revealed that his visual acuity decreased soon after CAS. Upon examination, the patient's visual acuity in the left eye was finger counting at a distance of 50 cm. Fundus examination revealed a pale optic disc and macular edema. Fluorescein angiography revealed no abnormal finding except a mild delay (18 sec.) in the arm to retina time. We checked the previous cerebral angiogram after CAS and found ophthalmic artery occlusion (
Fig. 5). Follow-up of the cerebral angiogram showed no occlusion in the left ophthalmic artery (
Fig. 6).
 | Fig. 5Cerebral angiogram after CAS demonstrates ophthalmic artery occlusion (arrow). 
|
 | Fig. 6Left cerebral angiogram two months after CAS shows no occlusion of the ophthalmic artery and normal blood flow. 
|
Go to :

DISCUSSION
CAS is an effective alternative treatment for patients who are not good candidates for CEA. However, it has several complications such as major or minor stroke, vasospasm, arterial dissection, residual stenosis and subarachnoid hemorrhage.
1)2) Distal arterial embolization is the most common complication, reported as high as 29-39.5%.
4)6) Most often, embolization occurs in the cerebral hemisphere. Jaeger et al.
4) reported that most embolic lesions were smaller than 5 mm and occurred in the distribution of the cortical branches of the MCA and ACA, in the parietal and frontal lobes, and in the upper and middle areas of the brain. These authors explained these embolic properties by the particles released during the procedure traveling in a straight path with the blood flow to the cortical branches of the MCA and ACA.
CRAO is an ophthalmologic emergency, characterized by a sudden onset of devastating visual loss. CRAO is a rare event, encountered in less than 0.1% of the cases.
7) Its causes include carotid bifurcation disease, cardiac disease, retinal artery thrombosis, vascular spasm, and vasculitis. Among these, embolism from the carotid bifurcation is the most common cause of CRAO and BRAO.
7)
Unlike CRAO, which can be thromboembolic or embolic, the causes of BRAO are almost always embolic.
8) Several studies reported CRAO or BRAO after CAS.
8)11-
13) Samardzic et al.
10) reported retinal circulation embolism after cardiac procedures. There are not many reports of the incidence of retinal artery embolization during or after CAS. Wilentz et al.
12) reported that the incidence of retinal artery embolization during CAS was 5% (six out of 118 patients). Two of these cases were symptomatic (1.7%).
CRAO caused by CAS can be explained by several mechanisms. One is an embolus obstructing the retinal artery. A study using transcranial Doppler measurements found a considerable number of embolic episodes during CAS, with an average of 74 emboli per procedure.
5) Atherosclerosis of the ophthalmic artery can be another cause of CRAO.
11) The third mechanism involves anastomosis between the ophthalmic artery and the external carotid artery.
12)13) The ophthalmic artery has numerous extra-orbital branches, which can have extensive anastomoses with the ICA. These anastomoses may cause retinal embolization when some types of embolic protection devices are used.
Several reports address risk factors of CRAO in patients with carotid stenosis. Muller et al.
9) reported that the patients with ulcerated, heterogeneous plaques have a higher risk of CRAO or BRAO. Kimura et al.
7) suspected that severe carotid stenosis, in addition to heterogenous plaques, is an important risk factor for retinal artery occlusion.
We present a case of ophthalmic artery occlusion during emergency revascularization of an acutely occluded ICA. During this procedure, interventionists cannot detect CRAO if the patient does not complain about visual symptoms. Unlike CRAO, ophthalmic artery occlusion can be easily detected and is treated simultaneously if the interventionists are aware of this condition. In our case, the ophthalmic artery occlusion was caused by a thrombus that filled the ICA due to ICA occlusion. After CAS, restoration of ICA flow pushed the thrombus to the ophthalmic artery. Therefore, we suggest that acute ICA occlusion carries a higher risk of ophthalmic artery occlusion or CRAO than ICA stenosis.
Go to :

CONCLUSION
Ophthalmic artery occlusion or CRAO during CAS are rare complications, but when they occur they are disastrous. Endovascular neurosurgeons should closely observe ophthalmic arterial blood flow during CAS, especially in the treatment of acute ICA occlusion.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download