Abstract
While Onyx embolization of cerebrospinal arteriovenous shunts is well-established, clinical researchers continue to broaden applications to other vascular lesions of the neuraxis. This report illustrates the application of Onyx (eV3, Plymouth, MN) embolization to vertebral body lesions, specifically, a vertebral hemangioma and renal cell carcinoma vertebral body metastatic lesion.
Hypervascular bone metastases and vascular spinal tumors can cause high volume blood loss during open surgery.2)3)6) Presurgical embolization of these lesions decreases intraoperative blood loss and facilitates subsequent surgical resection.7)15)19) Agents used for embolization of tumors include polyvinyl alcohol (PVA), gelfoam powder, fibrin glue, gelatin microspheres, liquid adhesives, alcohol and coils.4)11) Until recently, PVA particle embolization has served as the mainstay of embolization.4)11) Onyx (eV3, Plymouth, MN, USA) is a nonpolymerizing liquid agent composed of ethylene-vinyl alcohol copolymer dissolved in dimethyl sulfoxide. When injected, Onyx precipitates within vessels forming a spongy cast. We report the use of Onyx in the embolization of vertebral body lesions, including a renal cell carcinoma vertebral body metastatic lesion and a vertebral hemangioma.
A 74-year-old male patient with ongoing persistent lower lumbar spine pain, shortness of breath, and cough was initially treated symptomatically for his pain and for presumed pneumonia. Computed tomography (CT) demonstrated an 11 mm right middle lobe lesion and an indeterminate 13 mm right adrenal lesion, prompting further evaluation with positron emission tomography (PET)-CT. A PET-CT demonstrated a fluorodeoxyglucose (FDG)-avid left renal mass suggestive of malignancy with an associated L2 vertebral body and left humeral head destructive lesion. He underwent total spine magnetic resonance imaging (MRI) and lumbar spine CT imaging, revealing a large destructive L2 vertebral body lesion with a pathologic fracture and 4-mm soft tissue extension into the ventral spinal canal, resulting in moderate left-sided spinal canal narrowing (Fig. 1). Significant L2-L3 left subarticular zone, neural foraminal narrowing, and compression on the left traversing L3 and exiting L2 nerve roots were also identified. There was no cord compression or signal abnormality. The patient was referred for embolization prior to planned surgical resection.
The patient was placed under general anesthesia and standard access with a 5 French sheath in the common femoral artery was achieved. A 5 French Mickelson catheter (Cook Medical Inc., Bloomington, IN, USA) was employed to selectively catheterize the left L2 segmental artery and an angiographic run demonstrated an obvious pathologic blush in the region of the L2 vertebral body (Fig. 2A). Opacification of a spinal pial artery (artery of Adamkiewicz) was not seen. An Echelon microcatheter (eV3, Plymouth, MN, USA) was advanced through the Mickelson catheter (Cook Medical Inc., Bloomington, IN, USA) into the distal left L2 segmental artery and Onyx-18 (eV3, Plymouth, MN, USA) was injected, creating a cast within the segmental artery. The injected Onyx-18 was allowed to reflux into the vertebral body until the metastatic lesion was completely embolized (Fig. 2B-C). A total volume of 0.64 milliliters (mL) of Onyx was used. Subsequent selective injection of the right L2 segmental artery demonstrated minimal pathologic blush. The total fluoroscopy time for the procedure was 33 minutes, and the procedural duration was 2.5 hours. Post-procedure plain X-ray films confirmed Onyx distribution in the left half of the vertebral body, within the tumor (Fig. 3). The patient subsequently underwent an uneventful corpectomy and fusion with minimal blood loss (less than 100 cc) and recovered without complications.
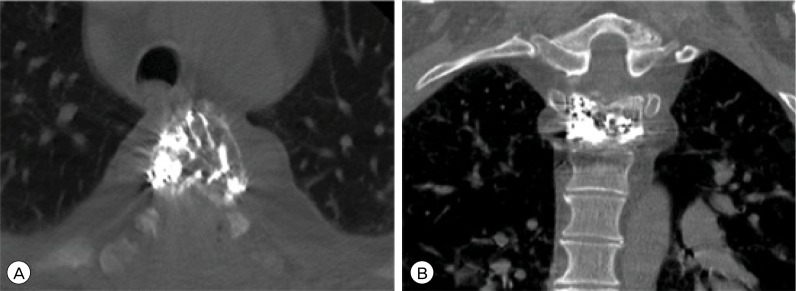
A 52-year-old male patient presented with six months of progressive bilateral lower extremity weakness and worsening sensory function, leading to multiple falls. There were also spasms and spasticity of the lower extremities bilaterally, and several episodes of fecal and urinary incontinence. A CT and total spine MRI revealed multiple lesions with coarse trabeculae in the thoracic (T1, T3 and T11) and lumbar spine (L1), most severe within the T3 vertebral body. These lesions extended to the posterior elements and soft tissues in the surrounding paravertebral and epidural space, causing significant anterior cord compression (Fig. 4).
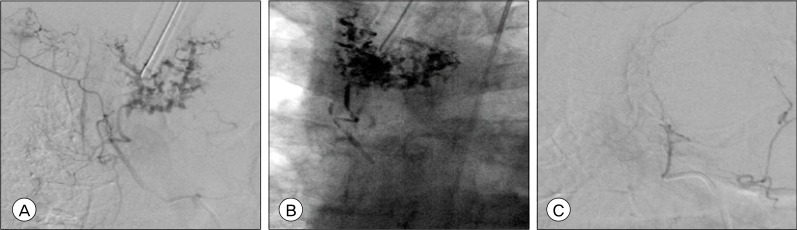
An open biopsy confirmed an intraosseous hemangioma, and the patient was referred for embolization prior to anticipated surgical resection. The patient was placed under general anesthesia and standard access with a 5 French sheath in the common femoral artery was achieved. The right T4 segmental artery was selectively catheterized with a Cobra catheter (Terumo, Somerset, NJ, USA). Angiography demonstrated a large pathologic blush in the region of the T3 vertebral body, corresponding to the known hemangioma (Fig. 5A). Opacification of a spinal pial artery was not seen. An Echelon microcatheter was advanced into the segmental artery and the vascular supply to the hemangioma was embolized with a total of 0.24 mL of Onyx-18 (Fig. 5B). The procedural total fluoroscopy time was 27 minutes, and procedural duration was 2.5 hours. Post-embolization angiography via the Cobra catheter confirmed no further pathologic blush (Fig. 5C, Fig. 6). The patient recovered uneventfully from the embolization and surgical resection, the latter with 300 cc of estimated blood loss.
Metastatic disease occurs in approximately 30% to 50% of patients with renal cell carcinoma at the time of initial diagnosis.9)15)16)18) Approximately 40% of patients develop bone metastases.11) In addition to drug-based therapies such as bisphosphonates and denosumab for the treatment of osseous metastatic lesions, radiation therapy and surgery are important in the treatment of renal cell carcinoma bone metastases.18) These interventions are considered appropriate when there is mechanical instability, intractable pain, radiculopathy and pathologic fractures.11)13)15)18) Surgical decompression and stabilization are the treatments of choice for radiation resistant metastatic spinal tumors.11)13)14) Renal cell metastases to the vertebral bodies are, however, highly vascular and can cause life threatening bleeding.11)14)15)
Vertebral hemangiomas are also highly vascular intraosseous lesions, thought to occur in approximately 10% of all patients, most commonly in the thoracic and lumbar spine.5)6)10)17) These lesions are typically asymptomatic though they may enlarge, causing pain and neurological deficits secondary to spinal cord compression or pathological fractures.1)8)
Multiple studies have demonstrated safe and effective results from preoperative embolization of both spinal metastases of renal origin and vertebral hemangiomas. Sundarasean et al. demonstrated successful results in the treatment of 17 patients who underwent selective spinal angiography and preoperative embolization with absolute ethyl alcohol in the treatment of spinal metastases.15) In 1999, Berkfield et al. verified the effectiveness of particle embolization, PVA, in reducing perioperative hemorrhage prior to corporectomy in hypervascular spinal tumors.2) Smith et al. demonstrated the safety and effectiveness of transarterial embolization of symptomatic vertebral hemangiomas in eight cases using PVA.12) In 2013, Yao et al. described four cases of transpedicular n-butyl cyanoacrylate (NBCA) direct-puncture embolization of spinal hemangiomas as a preoperative adjunct, facilitating resection of these high vascular tumors.19)
Cases reporting the use of Onyx for preoperative embolization of spinal tumors are limited. Hurley et al. were the first to document the use of Onyx, transarterially, in the treatment of two cases of aggressive vertebral hemangiomas.6) Additional studies report use of Onyx via an arterial route and by direct puncture in the treatment of hypervascular head, neck and spinal tumors.4) Advantages of Onyx embolization include a more controlled injection due to gradual precipitation in a centripetal fashion, allowing for slower and more accurate injections as well as penetration of very small caliber vessels.4) In addition, it can be easily visualized during surgery via intraoperative X-rays and directly visualized, serving as a roadmap for the surgeon.
As is done during particulate embolization, careful attention must be paid to the initial diagnostic angiographic run prior to embolization to ensure opacification of a spinal pial artery such as the artery of Adamkiewicz is not seen. In both of our illustrative cases, this was not seen and embolization proceeded uneventfully without complication. Notably, as is illustrated in Fig. 3, reflux of Onyx into the epidural venous plexus may occur without resultant morbidity. Our results further the growing body of literature confirming the safety and efficacy of Onyx embolization of vertebral body lesions.
References
1. Acosta FL Jr, Dowd CF, Chin C, Tihan T, Ames CP, Weinstein PR. Current treatment strategies and outcomes in the management of symptomatic vertebral hemangiomas. Neurosurgery. 2006; 2. 58(2):287–295. discussion 287-95. PMID: 16462482.

2. Berkefeld J, Scale D, Kirchner J, Heinrich T, Kollath J. Hypervascular spinal tumors: Influence of the embolization technique on perioperative hemorrhage. AJNR Am J Neuroradiol. 1999; 5. 20(5):757–763. PMID: 10369341.
3. Clarençon F, Di Maria F, Cormier E, Sourour NA, Enkaoua E, Sailhan F, et al. Onyx injection by direct puncture for the treatment of hypervascular spinal metastases close to the anterior spinal artery: Initial experience. J Neurosurg Spine. 2013; 6. 18(6):606–610. PMID: 23600580.

4. Elhammady MS, Wolfe SQ, Ashour R, Farhat H, Moftakhar R, Lieber BB, et al. Safety and efficacy of vascular tumor embolization using Onyx: Is angiographic devascularization sufficient? J Neurosurg. 2010; 5. 112(5):1039–1045. PMID: 19698039.

5. Fox MW, Onofrio BM. The natural history and management of symptomatic and asymptomatic vertebral hemangiomas. J Neurosurg. 1993; 1. 78(1):36–45. PMID: 8416240.

6. Hurley MC, Gross BA, Surdell D, Shaibani A, Muro K, Mitchell CM, et al. Preoperative Onyx Embolization of Aggressive Vertebral Hemangiomas. AJNR Am J Neuroradiol. 2008; 6. 29(6):1095–1097. PMID: 18372419.

7. Kim LJ, Albuquerque FC, Aziz-Sultan A, Spetzler RF, McDougall CG. Low morbidity associated with the use of NBCA liquid adhesive for preoperative transarterial emoblization of central nervous system tumors. Neurosurgery. 2006; 7. 59(1):98–104. discussion 98-104. PMID: 16823305.
8. Krueger EG, Sobel GL, Weinstein C. Vertebral hemangioma with compression of spinal cord. J Neurosurg. 1961; 5. 18:331–338. PMID: 13754556.

9. Lang EK, Sullivan J. Management of primary and metastatic renal cell carcinoma by transcatheter embolization with iodine 125. Cancer. 1988; 7. 62(2):274–282. PMID: 3383128.

10. Laredo JD, Reizine D, Bard M, Merland JJ. Vertebral hemangiomas: Radiologic evaluation. Radiology. 1986; 10. 161(1):183–189. PMID: 3763864.

11. Manke C, Bretschneider T, Lenhart M, Strotzer M, Neumann C, Gmeinwieser J, et al. Spinal metastases from renal cell carcinoma: Effect of preoperative particle embolization on intraoperative blood loss. AJNR Am J Neuroradiol. 2001; 5. 22(5):997–1003. PMID: 11337348.
12. Smith TP, Koci T, Mehringer CM, Tsai FY, Fraser KW, Dowd CF, et al. Transarterial embolization of vertebral hemangioma. J Vasc Interv Radiol. 1993; Sep-Oct. 4(5):681–685. PMID: 8219564.

13. Sundaresan N, Galicich JH, Lane JM, Bains MS, McCormack P. Treatment of neoplastic epidural cord compression by vertebral body resection and stabilization. J Neurosurg. 1985; 11. 63(5):676–684. PMID: 4056870.

14. Sundaresan N, Scher H, DiGiacinto GV, Yagoda A, Whitmore W, Choi IS. Surgical treatment of spinal cord compression in kidney cancer. J Clin Oncol. 1986; 12. 4(12):1851–1856. PMID: 2431111.

15. Sundaresan N, Choi IS, Hughes JE, Sachdev VP, Berenstein A. Treatment of spinal metastases from kidney cancer by presurgical embolization and resection. J Neurosurg. 1990; 10. 73(4):548–554. PMID: 2398386.

16. Swanson DA, Orovan WL, Johnson DE, Giacco G. Osseous metastases secondary to renal cell carcinoma. Urology. 1981; 12. 18(6):556–561. PMID: 7314355.

17. Thakur NA, Daniels AH, Schiller J, Valdes MA, Czerwein JK, Schiller A, et al. Benign tumors of the spine. J Am Acad Orthop Surg. 2012; 11. 20(11):715–724. PMID: 23118137.

18. Wood SL, Brown JE. Skeletal metastasis in renal cell carcinoma: Current and future management options. Cancer Treat Rev. 2012; 6. 38(4):284–291. PMID: 21802857.

19. Yao KC, Malek AM. Transpedicular N-butyl cyanoacrylate-mediated percutaneous embolization of symptomatic vertebral hemangiomas. J Neurosurg Spine. 2013; 5. 18(5):450–455. PMID: 23452246.

Fig. 1
Axial noncontrast lumbar spine computed tomography (A) and sagittal reformat (B) show a destructive L2 lesion with extension into the left pedicle and large epidural soft tissue component causing moderate spinal canal stenosis. There is pathologic compression with at least 50% loss of height centrally. Axial (C) and sagittal (D) T2 magnetic resonance images demonstrate a large destructive L2 lesion with pathologic fracture and 4 mm soft tissue extension into the ventral spinal canal, resulting in moderate left sided spinal canal narrowing.
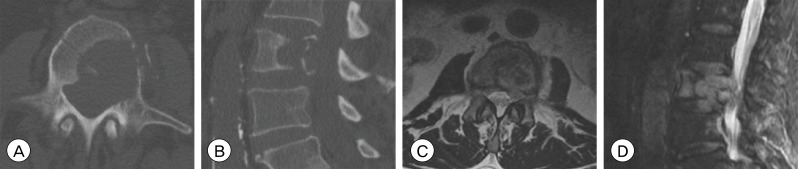
Fig. 2
Selective angiography of the left L2 segmental artery demonstrates a significant pathologic vascular blush at the level of the L2 vertebral body (A). Post-embolization unsubtracted radiograph shows Onyx distributed diffusely through the lateral vertebral body (B). Post-embolization selective left L2 segmental artery injection demonstrates grossly total angiographic devascularization of the L2 vertebral body tumor (C).

Fig. 3
Postembolization frontal (A) and lateral (B) lumbar spine radiographs show penetration of Onyx through tumor vessels within the L2 vertebral body. Reflux into the epidural venous plexus is seen.
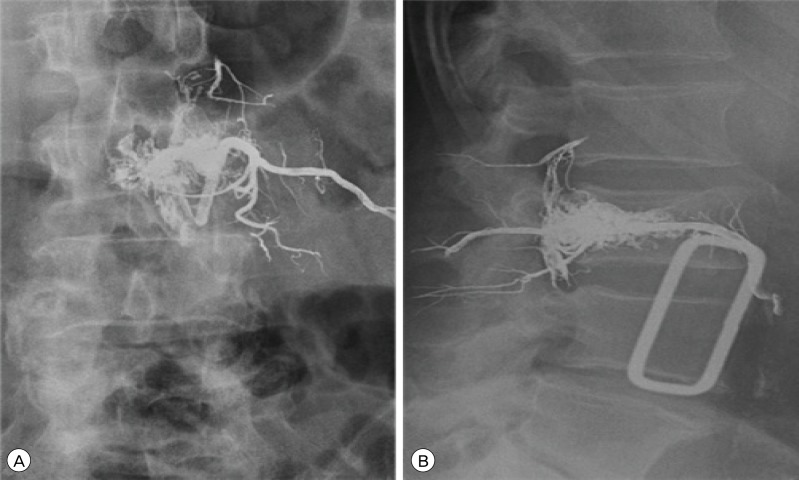
Fig. 4
Axial computed tomography demonstrates a hypodense lesion with coarse trabeculae within the T3 vertebral body with extensive soft tissue in the surrounding paravertebral and epidural space causing significant anterior cord compression (A). Sagittal T2-weighted (B) and Short T1 Inversion Recovery (STIR) (C) magnetic resonance images of thoracic spine demonstrate a heterogeneous lesion at the T3 vertebral body extending laterally and posteriorly through the vertebral body and causing severe central canal compression.
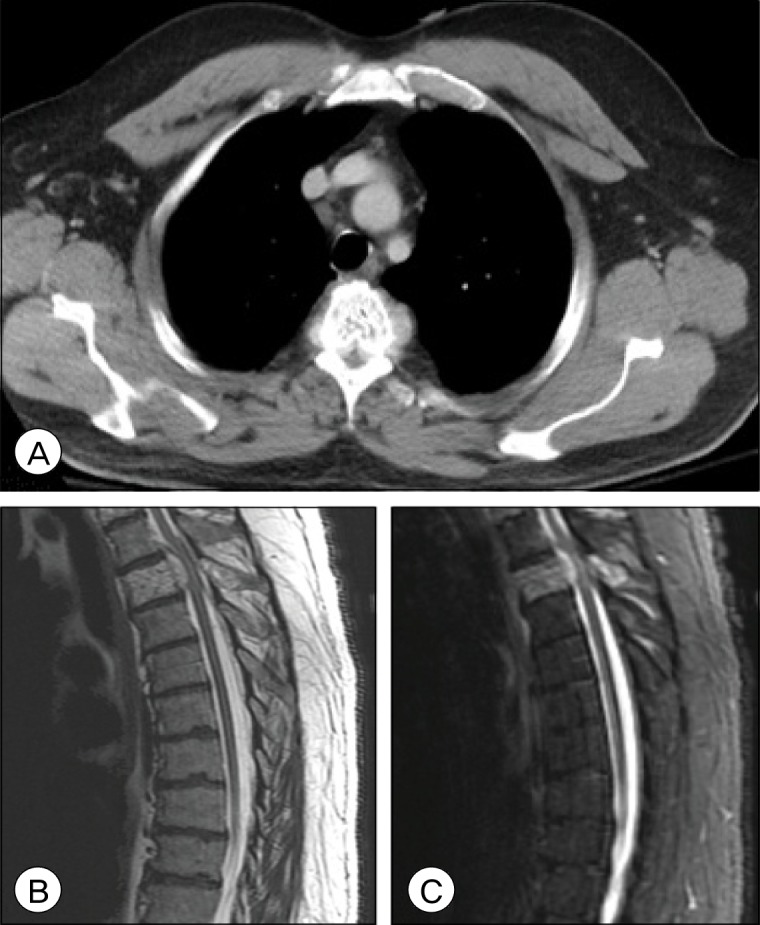
Fig. 5
Selective angiography of the right T4 segmental artery demonstrates a pathologic blush in the region of the T3 vertebral body (A). Intraprocedural unsubtracted antero-posterior radiograph demonstrates Onyx distributed through the known T3 hemangioma (B). Post-embolization selective injection of the right T4 segmental artery demonstrates no residual opacification of the pathologic vascular blush (C).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download