Abstract
A 35-year-old man presented with simultaneous multiple intracranial hematomas in the right cerebellar dentate nucleus and left basal ganglia. The hematomas were visible by computed tomography performed within two hours of the patient's arrival. The initial computed tomography showed acute hemorrhage in the left basal ganglia and dentate nucleus in cerebellum. The patient then experienced a change of consciousness due to newly developed hydrocephalus, and emergent extra-ventricular drainage was performed. By discharge, fortunately, the patient was fully recovered.
A hypertensive intracranial hemorrhage (ICH) is generally solitary.15) ICH occurrence accounts for 8 to 14% of all strokes in Europe and the United States,3)5) but 20 to 35% of all strokes in Asia.9)10)18) The occurrence of simultaneous multiple ICHs is a rare clinical entity, with a prevalence rate of 1% to 4.7% of all spontaneous ICH.2)14)15)17) Spontaneous ICH usually presents as right hemiplegia with increased severity in the foot, systemic arterial hypertension, vascular sensory deficits, and right homonymous hemianopsia upon malformation or aneurysmal rupture.8) Simultaneous multiple ICHs (SMICHs) are associated with cerebral aneurysms, vascular malformations, hemorrhagic infarction, coagulation defects, cerebral angiitis, neoplasms, sinus thrombosis, and/or amyloid angiopathy.13) Here we describe a case involving multiple ICHs that occurred simultaneously.
A 35-year-old patient was carried into the emergency room after sudden syncope or loss of consciousness. Several hours before this attack, the patient experienced a severe headache, nausea, and vomiting. His past medical history was unremarkable. He reported drinking 1-2 bottles of alcohol daily and smoking cigarettes for 25 years; he was also very obese. His initial blood pressure was 200/114 mmHg, pulse was 100 and regular and respiration rate was 18, body temperature was 36.6℃. No cardiac murmurs or neck bruits were present. He had no specific findings on the physical examination. The patient presented with drowsy mentality with mild dysarthria. Cerebellar function test abnormalities were observed. Initial Glasgow coma scale (GCS) score was 13. An electrocardiogram showed sinus tachycardia and left ventricular hypertrophy.
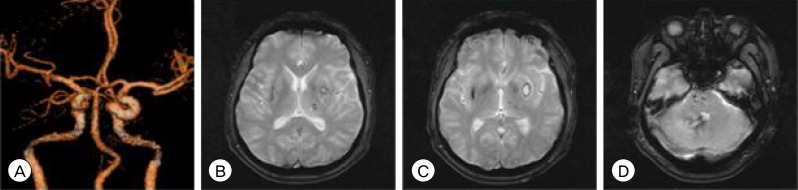
A computed tomography (CT) scan without brain contrast revealed multiple ICHs in the right cerebellar dentate nucleus and left basal ganglia (Fig. 1). He was admitted to the neurosurgical intensive care unit. We treated the patient with strict blood pressure control with intravenous hypertensive medication. After more deterioration of consciousness six hours later, a brain CT showed acute hydrocephalus without new bleeding, but edema around the hemorrhages. We diagnosed him with hydrocephalus and performed an emergency operation for extra-ventricular drainage (EVD) catheter insertion. Three days after the surgery, the patient's consciousness was fully recovered. He was overweight and lab findings showed high triglyceride, hyper-cholesterolemia. Brain CT angiography (Fig. 2A) showed right vertebral artery hypoplasia and diffuse cerebral arteriosclerosis. The magnetic resonance image findings (Fig. 2B, C, D) revealed old infarctions in the pons and left thalamus, a subacute infarction in the left frontal and parietal lobes, and multiple old microbleeds in the pons and the thalamus on both sides. Two days later, the patient was moved from the intensive care unit to the general ward. He was alert, followed commands well, and was able to walk voluntarily; however, his mild dysarthria remained. His modified Rankin scale (mRS) was 0 at discharge.
Recurrent hemorrhages are not an unusual finding in patients with previous hypertensive ICH,1)3)4) but the simultaneous occurrence of multiple intraparenchymal bleeding sites is rare and comprises only a small percentage of strokes.8)18) SMICH have been observed in only 2 to 3% of hemorrhagic stroke patients.11) Kabuto et al. reported that the most common location of multiple ICHs was the bilateral putamen, while only two of 17 multiple ICH patients in his case series had putaminal and cerebellar hemorrhages.7)13) Some studies suggest that the mean age and sex distributions of groups of patients with multiple ICHs are similar to those with solitary ICH,18) but that these patients exhibited a longer duration of chronic hypertension and more often a history of a previous stroke.13)18) Several risk factors, including blood pressure, blood sugar, cigarette smoking, alcohol drinking, and hypercholesterolemia have been examined as precipitating factors for hypertensive ICH. Other factors are not significantly associated with multiple ICHs. However, the blood pressure measurements that are taken after a stroke will most likely not reflect the patients' blood pressure before the stroke, as high blood pressure could be a result of increased intracranial pressure. Additionally, the prevalence of hypercholesterolemia was significantly higher in the group with multiple ICHs.13)
SMICH is a rare clinical entity, and the mechanisms are not clear and only occasionally associated with cerebral aneurysms, vascular malformations, hemorrhagic infarctions, coagulation defects, cerebral angiitis, neoplasms, sinus thrombosis, or amyloid angiopathy.11)15) The simultaneous development of intracranial hemorrhages in two different arterial territories may occur in hypertensive patients and create SMICH.8) The current theory is that the initial hemorrhage causes resulting structural or hemodynamic changes that tend to result in a second hemorrhage.16)18) The rupture of bilateral intracerebral microaneurysms may occur simultaneously by chance. The initial hemorrhage that results from a ruptured microaneurysm may cause the necessary conditions, such as hemodynamic changes and structural distortion, that rupture other microaneurysms, capillaries, and/or venules on the contralateral side, which are at risk, in a relatively short time,7) but our multivariate studies did not revealed these findings. In this patient, SMICH were found in the basal ganglia and cerebellum. One hematoma was supratentorial, while the other was infratentorial. These two hematomas had different vascular territories and flow dynamics. This type of SMICH is very rare.7) Some studies suggest that simultaneous supraand infratentorial hemorrhages occur commonly,7)12) but that their mechanism and pathophysiology are not clear. In any case, the high mortality and morbidity rates in these patients make the treatment of this devastating condition difficult. Thus, preventive measures must be taken.13) The management of ICH remains heterogeneous across institutions due to the lack of information regarding medical and surgical effectiveness of these methods of management.18) The indications of surgery for multiple simultaneous hypertensive ICHs are ambivalent.15) For patients with multiple ICHs, surgery seems of minor use.18) Treatment may be either medical or surgical, and the decision for treatment should be based on the GCS score of the patient, the locations and sizes of the hematomas, and the presence of additional medical problems. Patients with GCS scores over 5 or those with additional problems, as in our case, should be treated medically.6) Adequate blood pressure control is an important part of management of SMICH. The majority of patients with SMICH have poor outcomes because of their severely impaired consciousness.13) The mortality rate for patients with SMICH is much higher than that of patients with a single ICH, even if the hematomas were small.7)8)16)18) In our case, the patient had hydrocephalus, and we performed an EVD operation. Because he had a cerebellar hematoma, the EVD operation had the potential to expand the hematoma and aggravate his neurological symptoms. However, it was a small hematoma, and, thus we were able to drain the cerebrospinal fluid very slowly with a catheter.
Simultaneous multiple ICH is rare, and the mechanism is not clear. With the increased availability of the use of CT scans for the diagnosis of ICH, the overall diagnostic rate of multiple ICHs is likely to rise. Medical professionals should be alert and initiate treatment for excessive reflex hypertension to properly treat this dangerous condition.
References
1. Bae H, Jeong D, Doh J, Lee K, Yun I, Byun B. Recurrence of bleeding in patients with hypertensive intracerebral hemorrhage. Cerebrovasc Dis. 1999; Mar-Apr. 9(2):102–108. PMID: 9973653.

2. Balasubramaniam S, Nadkarni TD, Goel A. Simultaneous thalamic and cerebellar hypertensive haemorrhages. Neurol India. 2007; Apr-Jun. 55(2):183–184. PMID: 17558137.

3. Bamford J, Sandercock P, Dennis M, Warlow C, Jones L, McPherson K, et al. A prospective study of acute cerebrovascular disease in the community: The Oxfordshire Community Stroke Project 1981-86. 1. Methodology, demography and incident cases of first-ever stroke. J Neurol Neurosurg Psychiatry. 1988; 11. 51(11):1373–1380. PMID: 3266234.

4. Bayramoğlu M, Karatas M, Leblebici B, Cetin N, Sozay S, Turhan N. Hemorrhagic transformation in stroke patients. Am J Phys Med Rehabil. 2003; 1. 82(1):48–52. PMID: 12510185.

5. Becker C, Howard G, McLeroy KR, Yatsu FM, Toole JF, Coull B, et al. Community hospital-based stroke programs: North Carolina, Oregon, and New York. II: Description of study population. Stroke. 1986; Mar-Apr. 17(2):285–293. PMID: 3083536.

6. Butcher K, Laidlaw J. Current intracerebral haemorrhage management. J Clin Neurosci. 2003; 3. 10(2):158–167. PMID: 12637041.

7. Kabuto M, Kubota T, Kobayashi H, Nakagawa T, Arai Y, Kitai R. Simultaneous bilateral hypertensive intracerebral hemorrhages-Two case reports. Neurol Med Chir (Tokyo). 1995; 8. 35(8):584–586. PMID: 7566389.
8. Kohshi K, Abe H, Tsuru E. Simultaneous hypertensive intracerebral hematomas: Two case reports. J Neurol Sci. 2000; 12. 181(1-2):137–139. PMID: 11099724.

9. Kojima S, Omura T, Wakamatsu W, Kishi M, Yamazaki T, Iida M, et al. Prognosis and disability of stroke patients after 5 years in Akita, Japan. Stroke. 1990; 1. 21(1):72–77. PMID: 2300993.

10. Lin YT, Lo YK, Kuo HC, Chang YT, Chang MH, Li JY. Stroke registry in Kaohsiung Veterans General Hospital. Zhonghua Yi Xue Za Zhi (Taipei). 2002; 7. 65(7):307–313. PMID: 12365647.
11. Mauriño J, Saposnik G, Lepera S, Rey RC, Sica RE. Multiple simultaneous intracerebral hemorrhages: Clinical features and outcome. Arch Neurol. 2001; 4. 58(4):629–632. PMID: 11295994.
12. Ozdemir O, Calisaneller T, Yildirim E, Altinors N. Simultaneous supra and infratentorial hypertensive intracerebral haemorrhage. J Clin Neurosci. 2007; 8. 14(8):775–777. PMID: 17493816.

13. Silliman S, McGill J, Booth R. Simultaneous bilateral hypertensive putaminal hemorrhages. J Stroke Cerebrovasc Dis. 2003; 1. 12(1):44–46. PMID: 17903903.

14. Sorimachi T, Ito Y, Morita K, Fujii Y. Microbleeds on gradient-echo T2(*)-weighted MR images from patients with multiple simultaneous intracerebral haemorrhages. Acta Neurochir (Wien). 2007; 2. 149(2):171–176. discussion 176-7. PMID: 17211554.
15. Takeuchi S, Takasato Y, Masaoka H, Hayakawa T, Yatsushige H, Sugawara T. Simultaneous multiple hypertensive intracranial hemorrhages. J Clin Neurosci. 2011; 9. 18(9):1215–1218. PMID: 21752649.

16. Tanno H, Ono J, Suda S, Karasudani H, Yamakami I, Isobe K, et al. [Simultaneous, multiple hypertensive intracerebral hematomas: Report of 5 cases and review of literature]. No shinkei Geka. 1989; 3. 17(3):223–228. Japanese. PMID: 2671770.
17. Weisberg L. Multiple spontaneous intracerebral hematomas: clinical and computed tomographic correlations. Neurology. 1981; 7. 31(7):897–900. PMID: 7195516.

18. Yen CP, Lin CL, Kwan AL, Lieu AS, Hwang SL, Lin CN, et al. Simultaneous multiple hypertensive intracerebral haemorrhages. Acta Neurochir (Wien). 2005; 4. 147(4):393–399. discussion 399. PMID: 15605198.

Fig. 1
Initial brain non contrast enhanced computed tomography (CT) scan: Intracerebral multiple hematomas with right cerebellar dentate nucleus (A) and left basal ganglia (B).
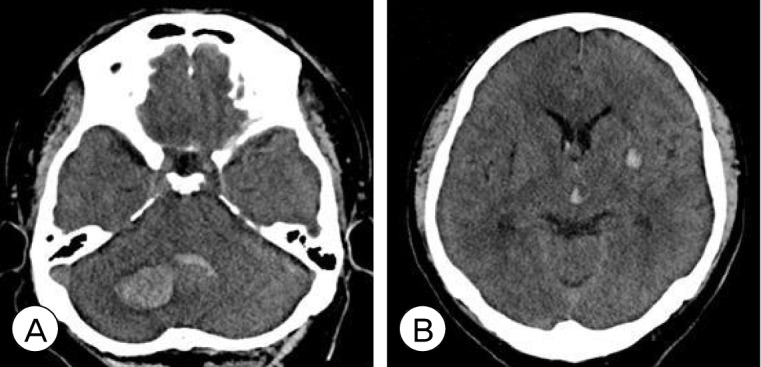
Fig. 2
(A) Brain CT angiography: Right vertebral artery hypoplasia and diffuse cerebral arteriosclerosis. (B, C, D) Brain magnetic resonance image (MRI): Multiple old infarctions in pons, left thalamus, subacute infarction in left frontal and parietal lobes and multiple old microbleeds in pons and both thalami.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download