Abstract
Mycotic aneurysms are rare inflammatory neurovascular lesions. Ruptured mycotic aneurysm manifesting as subdural hematoma is extremely rare. A 72-year-old male patient was admitted to our hospital with headache and drowsiness. Computer tomography (CT) of brain and CT angiography revealed subdural hematoma and an aneurysm located at the M4 segment of the left middle cerebral artery (MCA). Cerebral angiogram revealed 2 aneurysms; one located at the left distal MCA and the other at the bifurcation of left MCA. Laboratory studies showed leukocytosis and elevated inflammatory factors. The patent was treated with antibiotic therapy for 4 weeks. The follow-up CT and cerebral angiography showed that the mycotic aneurysm was completely resolved, and the patient was nearly free of symptoms.
Mycotic aneurysms are rare inflammatory neurovascular lesions first described in 1855.6) Mycotic aneurysms account for approximately 2.5 ~ 4.5% of all intracranial aneurysms and are unique in their natural history, pathologic findings, location and common multiplicity.6)8)26)27)34) Their spontaneous rupture mostly results in subarachnoid and intracerebral hemorrhage, accompanied by morbidity and mortality as high as 60 ~ 90% in older case reports, and 12 ~ 32% in more recent reports.17)29) Ruptured mycotic aneurysm manifesting as subdural hematoma (SDH) is extremely rare; only 10 cases have been reported.2-4)13-15)20)26)31)34) We present a case of mycotic aneurysm associated with SDH, which was resolved with medical treatment.
A 72-year-old male patient visited our hospital for headache and drowsiness. He slipped and suffered from blunt traumas to his head 10 days before his visit to the hospital. He showed right hemiparesis with a motor power of grade IV/V in the right upper and lower limbs. The initial Glasgow coma scale score was 12 (Eye response - 3, Verbal response - 4, Motor response - 5). He had no extracranial wounds and the vital signs were stable, but his body temperature was mildly elevated. The patient had a history of type 2 diabetes mellitus and hypertension, and he was a heavy alcoholic.
Enhanced computer tomography (CT) of the brain showed subacute subdural hematomas on both fronto-parietal areas and an enhancing nodule in the left parietal area (Fig. 1). No signs of scalp contusion and skull fracture were found. CT angiography revealed that the enhancing nodule was a saccular aneurysm located at the M4 segment of the left middle cerebral artery (MCA). Cerebral angiogram showed 2 aneurysms; one located at the distal left MCA and the other at the bifurcation of the left MCA (Fig. 2).
Laboratory studies revealed an elevated erythrocyte sedimentation rate (ESR, 49 mm/hr), white blood cell count (WBC, 12,990/µL) and C-reactive protein (CRP, 9.28 mg/L), but other hematological and biochemical parameters were within normal range. Blood cultures were negative and there was no evidence of infective endocarditis in the echocardiography.
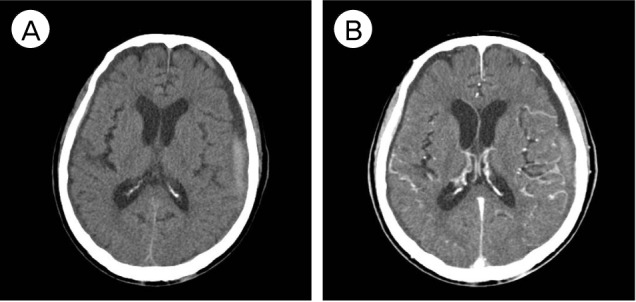
Intravenous ceftriaxone 1 g every 12 hours was started. His symptoms improved gradually over the next few days. The enhanced CT 10 days after admission revealed disappearance of the aneurysm located at the M4 segment and partial resolution of SDH (Fig. 3). Additional angiography was performed 20 days after antibiotic therapy. It revealed complete resolution of the aneurysm at the left distal MCA (Fig. 4). Antibiotics were continuously given for 4 weeks with moderate improvement of his symptoms and the patient was discharged. Because the aneurysm located at the bifurcation of the left MCA was small and had no interval change, we decided to observe it in our outpatient department.
Mycotic aneurysms are rare inflammatory neurovascular lesions, comprising 0.7-5.4% of all intracranial aneurysms.1) Sixty five percent of patients of mycotic aneurysms have underlying endocarditis.1) Other common sources of infection are intravenous drug abuse (6.3%), bacterial meningitis (5.2%), poor dental hygiene (4.2%) and cavernous sinus thrombosis (2.8%).1) In this case, no infective endocarditis or infectious diseases were found. However, the patient was old, a heavy alcoholic and had a history including diabetes mellitus. This can increase the risk of infectious diseases, but the origin of the mycotic aneurysm was not found.
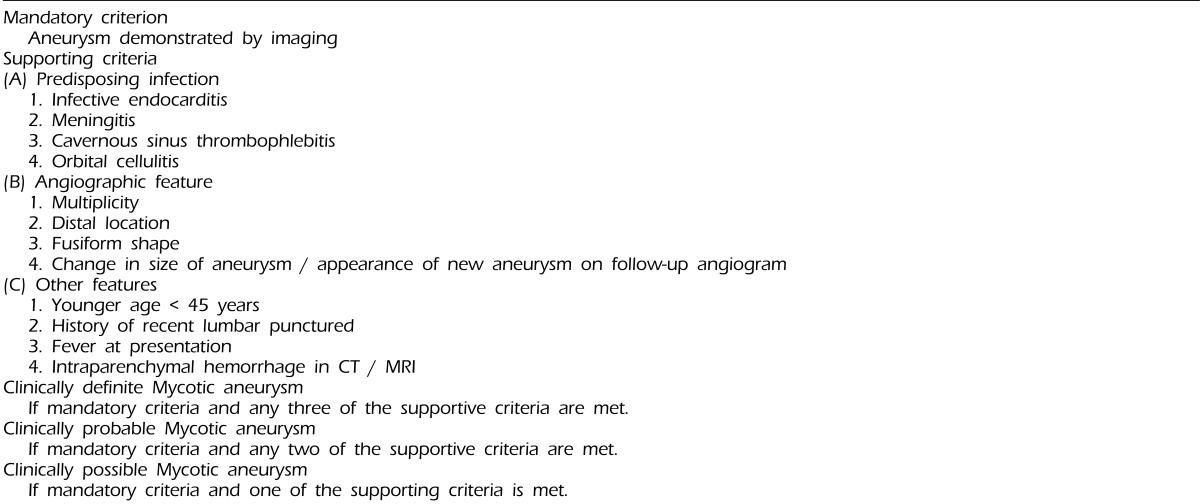
There are several limitations in diagnosing mycotic aneurysms, because the infectious pathological lesions can be identified histopathologically only in resected specimens. It is possible to diagnose mycotic aneurysm when the lesion was resolved completely under treatment. The recently published diagnostic criteria enable early diagnosis of mycotic aneurysm (Table 1).12) These criteria are easy to apply and have 96% sensitivity and 100% specificity to differentiate mycotic aneurysm from a noninfectious aneurysm.12) In our case, the patient had a fever at presentation, multiplicity and distal location of the aneurysm. The distal MCA aneurysm completely disappeared in angiography after antibiotic therapy. Following the criteria mentioned above, the aneurysm located at the M4 segment of left MCA can be diagnosed with a mycotic aneurysm.
The rupture of mycotic aneurysm causes intraparenchymal (28%), subarachnoid (22%) and intraventricular hemorrhage (5%).1) A mycotic aneurysm associated with SDH is a rare case.16) Only 10 cases have been reported.2-4)14-16)20)26)31)34) In this case, his head trauma may have caused the rupture of the underlying mycotic aneurysm. On the other hand, the trauma could directly cause bilateral subdural hematomas and the mycotic aneurysm could be found incidentally.
CT angiography is a useful non-invasive tool in the diagnosis of mycotic aneurysms and detecting intracranial hemorrhage and edema.1) Cerebral angiography is the gold standard for the diagnosis of mycotic aneurysms and is often used in determining treatment method and prognosis.5) Laboratory studies are typically suggestive of an underlying inflammatory process and may include leukocytosis, elevated ESR, CRP, and anemia.6) Elevated ESR, CRP and leukocytosis provide supporting evidences of mycotic aneurysms.35) Blood cultures are positive in only 35.6% of patients.1) In our case, WBC count, ESR and CRP were elevated but blood cultures were negative.
There is no randomized controlled trial or prospective cohort study evaluating treatment approaches to mycotic aneurysms. Because there is no standard recommendation about clinical decision making, treatment of mycotic aneurysms is highly individualized and varied.18) Treatment approach is usually dependent on the rupture status. In the case of unruptured mycotic aneurysms, the treatment was generally initiated with antibiotic therapy alone.1) Antibiotic therapy should be guided by culture results obtained from blood or cerebrospinal fluid samples, but if cultures are negative, empirical antibiotics should be initiated according to the suspected predisposing infection. The existing literature generally supports a minimum of 4 to 6 weeks of antibiotic therapy.18) Serial CT scan or angiography should be followed to monitor the status of the aneurysm during conservative care.
In the case of ruptured mycotic aneurysms, definitive treatment relies on surgical clipping, endovascular coiling, or trapping of the aneurysm. Patients with hematoma and significant mass effect require emergency surgery. Frazee recommended antibiotic therapy as the first line of treatment for mycotic aneurysm.9) Some studies suggested that standard recommendations of treatment were to initiate intravenous antibiotics on an empirical basis.7)28)30) In Kanoth's study, 25 patients were treated with medical, surgical and endovascular method, and some cases with intracranial hemorrhage were completely resolved by antibiotic therapy alone.24) Some cases required surgery because the lesions were not resolved or enlarged.24) In our case, the treatment was started with antibiotics alone because he didn't have significant mass effect from the subdural hematomas and no signs of tentorial herniation. The subdural hematomas in initial CT were subacute types and there was no presence of midline shift. We planned urgent surgery if his neurologic deterioration aggravated or the hematomas expanded. However, his symptoms improved gradually after antibiotic therapy. Both subdural hematomas were resolved in later CT and the follow-up cerebral angiography revealed disappearance of the distal MCA aneurysm.
We experienced a rare case of ruptured mycotic aneurysm associated with SDH without infective endocarditis and any other infectious disease. After treatment with antibiotics for 4 weeks, the patient was nearly relieved of symptoms. The mycotic aneurysm resolved completely in the follow-up angiography.
References
1. Ducruet AF, Hickman ZL, Zacharia BE, Narula R, Grobelny BT, Gorski J, et al. Intracranial infectious aneurysms: A comprehensive review. Neurosurg Rev. 2010; 1. 33(1):37–46. PMID: 19838745.

2. Bamford J, Hodges J, Warlow C. Late rupture of a mycotic aneurysm after cure of bacterial endocarditis. J Neurol. 1986; 2. 233(1):51–53. PMID: 3754002.

3. Bandoh K, Sugimura J, Hosaka Y, Takagi S. Ruptured intracranial mycotic aneurysm associated with acute subdural hematoma - Case report. Neurol Med Chir (Tokyo). 1987; 1. 27(1):56–59. PMID: 2441289.
4. Barami K, Ko K. Ruptured mycotic aneurysm presenting as an intraparenchymal hemorrhage and nonadjacent acute subdural hematoma, case report and review of the literature. Surg Neurol. 1994; 4. 41(4):290–293. PMID: 8165497.

5. Bartakke S, Kabde U, Muranjan MN, Bavdekar SB. Mycotic aneurysm: An common cause for intra-cranial hemorrhage. Indian J Pediatr. 2002; 10. 69(10):905–907. PMID: 12450304.
6. Bohmfalk GL, Story JL, Wissinger JP, Brown WE Jr. Bacterial intracranial aneurysm. J Neurosurg. 1978; 3. 48(3):369–382. PMID: 580294.

7. Bonow RO, Carabello BA, Chatterjee K, de Leon AC Jr, Faxon DP, Freed MD, et al. 2008 Focused update incorporated into the ACC/AHA 2006 Guidelines for the management of patients with valvular heart disease: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): Endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2008; 10. 118(15):e523–e661. PMID: 18820172.

8. Frazee JG, Cahan LD, Winter J. Bacterial intracranial aneurysm. J Neurosurg. 1980; 11. 53(5):633–641. PMID: 6893602.
9. Frazee JG. Inflammatory intracranial aneurysm. In : Wilikins RH, Rengachary SS, editors. Neurosurgery. New York: McGraw-Hill;1996. p. 2379–2382.
10. Horstkotte D, Follath F, Gutschik E, Lengyel M, Oto A, Pavie A, et al. Guidelines on prevention, diagnosis and treatment of infective endocarditis executive summary; The task force on infective endocarditis of the European society of cardiology. Eur Heart J. 2004; 2. 25(3):267–276. PMID: 14972429.

11. Bederson JB, Meyer SA. Infectious intracranial aneurysm. In : Winn HR, editor. Youmans neurological surgery. 6th edition. Philadelphia, PA: Elsevier Saunders;2012. p. 3972–3977.
12. Kannoth S, Thomas SV, Nair S, Sarma PS. Proposed diagnostic criteria for intracranial infectious aneurysms. J Neurol Neurosurg Psychiatry. 2008; 8. 79(8):943–946. PMID: 18303107.

13. Kasuya H, Shimizu T, Tajika T, Kitamura K, Okada N, Sugama M, et al. [A case of septic aneurysm complicated with simultaneous subdural and intracerebral hematoma]. No Shinkei Geka. 1985; 10. 13(10):1109–1113. Japanese. PMID: 3841193.
14. King AB. Successful surgical treatment of an intracranial mycotic aneurysm complicated by a subdural hematoma. J Neurosurg. 1960; 7. 17:788–791. PMID: 14409147.

15. Matsuda T, Kiyosue H, Yamashita M, Tanoue S, Okahara M, Nagatomi H, et al. [A case of multiple mycotic intracranial aneurysms presenting with subdural hematoma]. No Shinkei Geka. 2002; 1. 30(1):73–78. Japanese. PMID: 11806111.
16. Morawetz RB, Karp RB. Evolution and resolution of intracranial bacterial (mycotic) aneurysms. Neurosurgery. 1984; 7. 15(1):43–49. PMID: 6548001.

17. Osler W. The Gulstonian lectures, on malignant endocarditis. Br Med J. 1885; 3. 1(1262):467–470.

18. Peters PJ, Harrison T, Lennox JL. A dangerous dilemma: Management of infectious intracranial aneurysms complicating endocarditis. Lancet Infect Dis. 2006; 11. 6(11):742–748. PMID: 17067923.

19. Phuong LK, Link M, Wijdicks E. Management of intracranial infectious aneurysms: A series of 16 cases. Neurosurgery. 2002; 11. 51(5):1145–1151. discussion 1151-2. PMID: 12383359.

20. Piastra M, Chiaretti A, Tortorolo L. Ruptured intracranial mycotic aneurysm presenting as cerebral haemorrhage in an infant: Case report and review of the literature. Childs Nerv Syst. 2000; 3. 16(3):190–193. PMID: 10804057.

21. Pruitt AA, Rubin RH, Karchmer AW, Duncan GW. Neurologic complications of bacterial endocarditis. Medicine (Baltimore). 1978; 7. 57(4):329–343. PMID: 580794.

22. Sonneville R, Mirabel M, Hajage D, Tubach F, Vignon P, Perez P, et al. Neurologic complications and outcomes of infective endocarditis in critically ill patients: The ENDOcardite en REAnimation prospective multicenter study. Crit Care Med. 2011; 6. 39(6):1474–1481. PMID: 21358398.

23. Kannoth S, Thomas SV. Intracranial microbial aneurysm (Infectious aneurysm): Current options for diagnosis and management. Neurocrit Care. 2009; 11(1):120–129. PMID: 19322683.

24. Kannoth S, Iyer R, Thomas SV, Furtado SV, Rajesh BJ, Kesavadas C, et al. Intracranial infectious aneurysm: Presentation, management and outcome. J Neurol Sci. 2007; 5. 256(1-2):3–9. PMID: 17360002.

25. Sugg RM, Weir R, Vollmer DG, Cacayorin ED. Cerebral mycotic aneurysm treated with a neuroform stent: Technical case report. Neurosurgery. 2006; 2. 58(2):E381. discussion E381. PMID: 16462464.
26. Sugino T, Yamamoto K, Kidooka M, Otsuka S. [A ruptured mycotic aneurysm, simultaneously associated with acute subdural hematoma and intracerebral hemorrhage: Case report and review of the literature]. No Shinkei Geka. 2002; 11. 30(11):1211–1215. Japanese. PMID: 12428355.
27. Suzuki Y, Kawamata T, Omura M, Matsumoto K. [Multiple bacterial aneurysms: case report]. No Shinkei Geka. 1998; 4. 26(4):357–362. Japanese. PMID: 9592817.
28. Tashima T, TakaKi T, Hikita T, Kuroiwa S, Hamanaka N, Takahashi M. [Bacterial intracranial aneurysm associated with infective endocarditis: A case showing enlargement of aneurysm size]. No Shinkei Geka. 1995; 11. 23(11):985–989. Japanese. PMID: 7477721.
29. Theodore S, Unnikrishnan M, Neelakandhan KS. Extracranial carotid aneurysms in young patients. Ann Thorac Surg. 2006; 5. 81(5):1943. author reply 1943-4. PMID: 16631720.

30. Tice AD, Rehm SJ, Dalovisio JR, Bradley JS, Martinelli LP, Graham DR, et al. Practice guidelines for outpatient parenteral antimicrobial therapy. IDSA guidelines. Clin Infect Dis. 2004; 6. 38(12):1651–1672. PMID: 15227610.
31. Tsuboi M, Adachi H. [A ruptured distal aneurysm, thought to be a mycotic aneurysm, associated with acute subdural hematoma: Case report and review of the literature]. No Shinkei Geka. 2002; 2. 30(2):177–181. Japanese. PMID: 11857942.
32. Tunkel AR, Hartman BJ, Kaplan SL, Kaufman BA, Roos KL, Scheld WM, et al. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis. 2004; 11. 39(9):1267–1284. PMID: 15494903.

33. Wakamoto H, Tomita H, Miyazaki H, Ishiyama N, Akasaka Y. [The early hemorrhage and development of a bacterial aneurysm after a cerebral ischemic attack caused by a septic embolism - A case report]. No Shinkei Geka. 2001; 5. 29(5):415–420. Japanese. PMID: 11449712.
34. Yamakawa H, Hattori T, Tanigawara T, Enomoto Y, Ohkuma A. Ruptured infectious aneurysm of the distal middle cerebral artery manifesting as intracerebral hemorrhage and acute subdural hemorrhage - Case Report. Neurol Med Chir (Tokyo). 2003; 11. 43(11):541–545. PMID: 14705320.
35. Yoon JO. Not just an aneurysm, but an infected one: A case report and literature. J Vasc Nurs. 2006; 3. 24(1):2–8. quiz 9-10. PMID: 16504845.

Fig. 1
Enhanced computed tomography (CT) of brain shows subacute subdural hematoma (SDH) and an enhancing nodule in the left fronto-parietal region and scanty subacute SDH in right fronto-parietal region. The CT angiography reveals that the enhancing nodule is a saccular aneurysm located at the M4 segment of left middle cerebral artery.
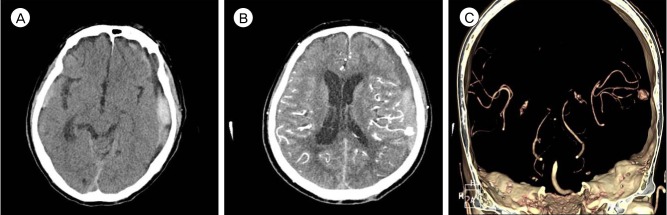
Fig. 2
Initial cerebral angiogram reveals 2 aneurysms; one located at the M4 segment of the left middle cerebral artery (MCA) and the other at the bifurcation of the left MCA.
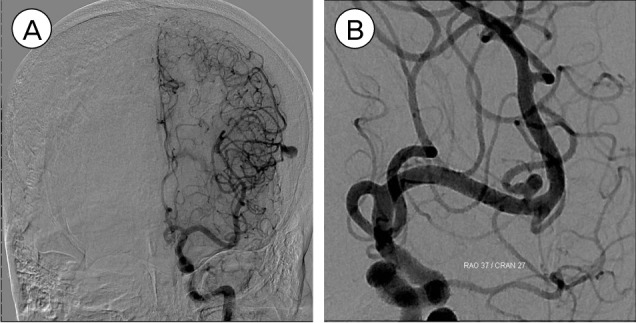
Fig. 3
Follow-up computed tomography (CT) scan 10 days after admission shows that both subdural hematomas were partially resolving state, and the enhanced CT scan shows that the enhancing nodule in the left parietal area disappears.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download