Abstract
Our objective was a retrospective assessment of the management modalities that provided the most beneficial treatment in hemorrhagic moyamoya disease during the last 13 years at our institution. The clinical results of 44 patients with hemorrhagic moyamoya disease were investigated, comparing revascularization surgery (direct, indirect, and combined bypass) or conservative treatment. Angiographic features, rebleeding, and clinical outcome were investigated. Six of the 35 patients (17.1%) with revascularization surgery experienced rebleeding, as did 4 of 9 patients (44.4%) with conservative treatment. However, patients who underwent bypass surgery had a lower chance of rebleeding. No significant difference in chance of rebleeding was observed between bypass surgery and non surgery groups (p > 0.05). Cerebral angiography performed after bypass surgery showed that for achieving good postoperative revascularization, direct and combined bypass methods were much more effective (p < 0.05). While the risk of rebleeding in the revascularization group was generally lower than in the conservative treatment group, there was no statistically significant difference between treatment modalities and conservative treatment. Although statistical significance was not attained, direct and combined bypass may reduce the risk of hemorrhage more effectively than indirect bypass.
Moyamoya disease (MMD) is a rare cerebrovascular disorder characterized by progressive occlusion of the bilateral supraclinoid internal carotid artery (ICA), proximal middle cerebral artery (MCA), and anterior cerebral artery (ACA), and a spontaneously developed collateral vascular network at the base of the brain consisting of the so-called moyamoya vessels.17)23)24) Clinically, MMD can be divided into 2 entities: juvenile and adult onset types.4)16) Although angiographic findings of these 2 types share similar characteristics, whether adult onset MMD represents progression of the juvenile onset form of the disease is not clear. Clinical presentation of MMD includes ischemia and hemorrhage in adults, as well as ischemic attacks in children.4)16) The goal of revascularization surgery for hemorrhagic MMD is to reduce the hemodynamic stress on the moyamoya vessels, but also acts as secondary preventive measure of stroke in the symptomatic moyamoya vessels ipsilateral to the hemorrhage.10)15) However, the treatment that best prevents recurrent intracranial hemorrhagic attack in the type of MMD characterized by hemorrhage is an open question.6)7)25)26)
Therefore, the main aim of this study is to compare the results of 3 surgical procedures performed by 1 neurosurgeon in adult patients with hemorrhagic MMD. Surgical outcomes were examined between 12 months and 13 years after the surgery (mean follow-up time: 55.4 months).
From 1998 to 2010, we diagnosed 44 patients with adult MMD (over 17 years of age) with hemorrhagic attack treated at our institution. In this series, data from these patients' records were retrospectively collected. With approval from the Institutional Review Board at our hospital, 18 men and 26 women participated and completed this syudy. All patients had hemorrhagic symptoms. The median age at the time of diagnosis was 44.9 years (range: 17-65 years). A diagnosis of MMD is based on angiography following published guidelines.2) All patients were evaluated with computed tomography (CT), CT perfusion (CTP) and magnetic resonance image (MRI) scans. Preoperative 6 vessel angiography, including both ICAs and external carotid arteries (ECAs), as well as 1 or both vertebral arteries, was performed in all patients to determine the extent and severity of the disease and to verify the presence of the superficial temporal artery (STA). Angiographic staging of MMD was based on Suzuki angiographic criteria.24) All patients were evaluated with CTP, MRI and single photon emission computed tomography (SPECT) with acetazolamide (Diamox) challenge. A nuclear medicine doctor who did not participate in the surgery interpreted all SPECT data. All patients underwent a detailed clinical assessment as part of the evaluation as a potential surgical candidate. The site, hemisphere, and type of bleeding demonstrated on CT scans at the time of the second bleeding episode were compared to those of the first bleeding episode.
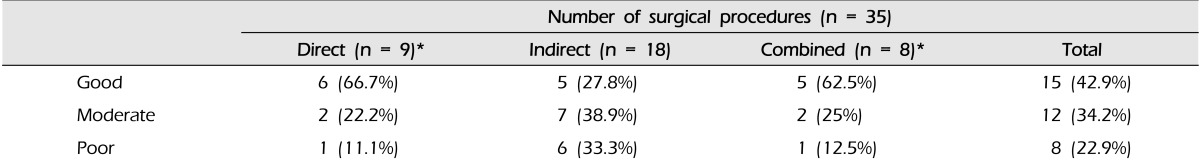
Indications of bypass surgery included 1) clinical symptoms are repeated due to cerebral hemorrhage and 2) regional cerebral blood flow, vascular response, and perfusion reserve were decreased. Patients with exclusion criteria for revascularization surgery had severe neurologic deficits due to hemorrhagic attack such as coma or semicomatose mental status. In this series, we performed 3 types of revascularization surgery for MMD: direct, indirect, and combined bypass. Direct bypass procedure was standard STA-MCA anastomosis.8) If a suitable recipient vessel could not be procured during surgery, indirect bypass, which includes encephalo-duro-arterio-galeo-synangiosis (EDAGS), encephalo-duro-arterio-myo-synangiosis (EDAMS), and encephalo-myo-synangiosis (EMS) was carried out as an alternative.3)9)12)22) Combined bypass was a combination of STA-MCA anastomosis and EDAGS, utilizing inverted STA-galeal flaps or galeal pedicles. Efficacy of the revascularization surgery was evaluated with postoperative angiography performed 6 to 12 months after surgery. The change of the postoperative angiogram was divided into 3 groups: good, moderate, and poor. If the decrease in the number of moyamoya vessels after revascularization exceeded one third of those counted preoperatively, the change was classified as "good". If the number of moyamoya vessels decreased was less than one third of those counted preoperatively, the change was determined to be "moderate". If these criteria were not met or no changes were observed, the angiographic change was determined to be "poor". For ease of statistical analysis, the angiographic changes were converted into a numerical score in which good is equal to 3, moderate is equal to 2, and poor is equal to 1. The follow-up period was 12 to 105 months (mean of 55.4 months). We confirmed recurrent intracranial hemorrhage and ischemic events using CT and MRI scanning. Every patient's neurological status was evaluated preoperatively and postoperatively in an outpatient department using the Rankin disability scale (RDS).20)
The frequency of hemorrhage or ischemic events, extent of revascularization and demographic data were statistically analyzed using chi-square test by treatment modality. A Rankin disability scale was used to determine the neurological functional outcome. The change of patient's neurological status (RDS) was analyzed using the Wilcoxon signed rank test by treatment modality. Freedom from recurrent hemorrhage and ischemic event were estimated using the Kaplan-Meier product-limit method. SPSS software (version 15.0, 2006, SPSS Inc., Chicago, IL, USA) was used throughout. Null hypotheses of no difference were rejected if p values were less than 0.05.
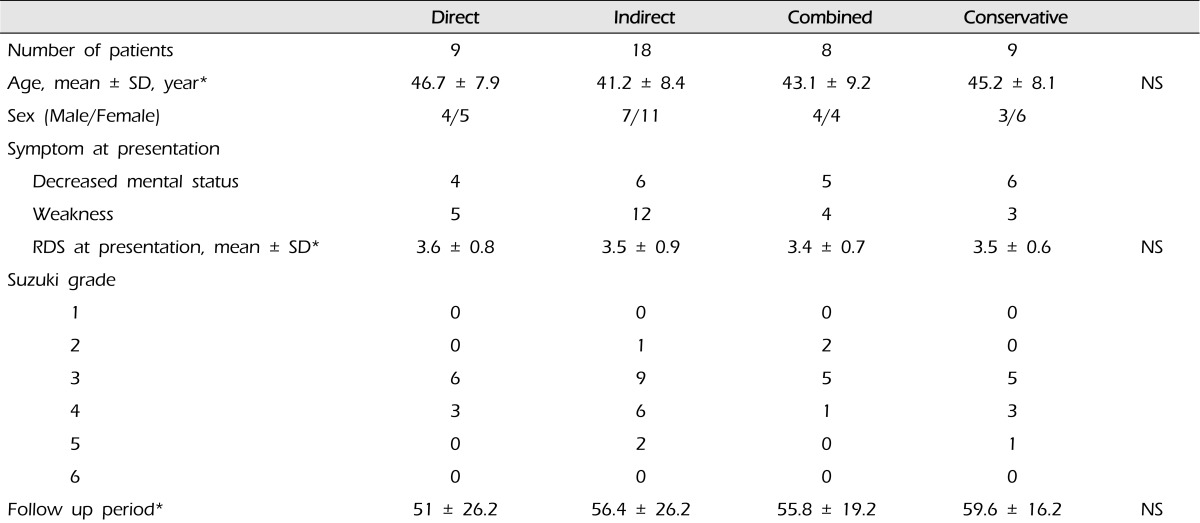
Among the 44 adult hemorrhagic MMD patients, bypass surgery was performed in 35 patients (79.5%) with 53 sides (17 patients unilaterally, 18 patients bilaterally) and conservative treatment in 9 patients (20.4%). All patients had intracranial hemorrhage. Basal cerebral blood flow (CBF) decreased in reaction to acetazolamide challenge in all cases. Revascularization surgery was performed more than a month after first hemorrhagic attack. Among the 35 surgically treated patients, 9 patients (25.7%) underwent direct bypass, 18 patients (51.4%) underwent indirect bypass, and 8 patients (22.9%) underwent combined bypass. Table 1 shows the demographic characteristics of the patients. The mean age was 44.9 years (range: 17-65 years). The age category with the most patients was between 41 and 50 years. There were no significant differences in age, preoperative clinical status (modified Rankin Scale, mRS), or length of follow-up among patients grouped by treatment modalities. Weakness and decreased mental status were the most common symptoms. Digital subtraction angiography was performed in all patients who had a confirmed moyamoya pattern of intracranial vascular morphology. In this study, any patients in whom the presence of aneurysm was confirmed by 6 vessels angiography was excluded from the study group. Suzuki's angiographic staging of the 44 patients showed the following: stage II in 3 patients, stage III in 25 patients, stage IV in 13 patients, stage V in 3 patients, and stage VI in no patients. Stages III and IV were the predominant angiographic finding in our series.
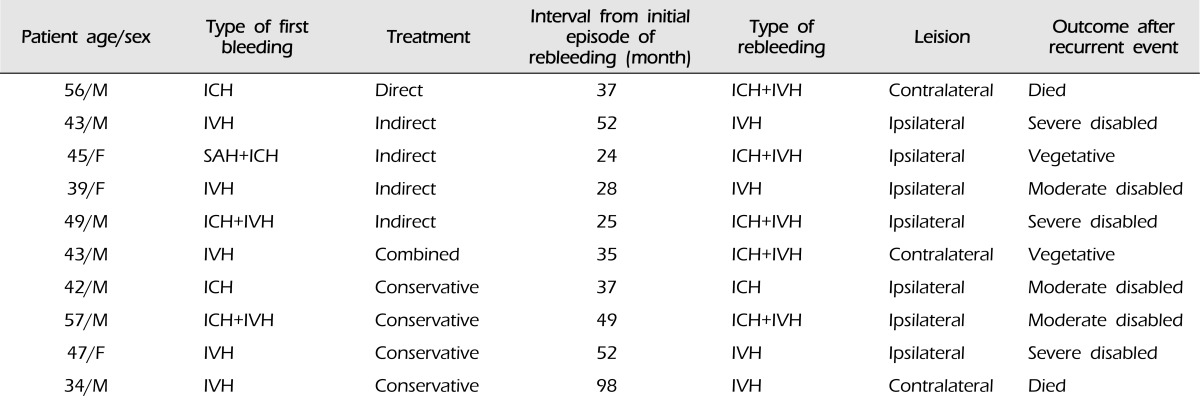
The types of hemorrhage in the first hemorrhagic event included 16 intracerebral hemorrhage (ICH), 20 intraventricular hemorrhage (IVH), 7 ICH with IVH and 1 subarachnoid hemorrhage (SAH). Ten of 44 patients (22.7%), including 7 males and 3 females, suffered rebleeding (Table 2). The interval from the initial episode of rebleeding ranged from 2 to 9 years (mean 3.6 years): 2 years for 3 patients, from 2 to 5 years for 6 patients, and from 6 to 10 years for 2 patients. Rebleeding tended to occur within 5 years of the initial hemorrhage. Of note, in 1 case, recurrent hemorrhage happened more than 9 years after the initial hemorrhagic event. Types of rebleeding were as follows: 1 ICH, 5 IVH, and 4 ICH with IVH. In 3 cases, the second bleeding episode occurred in the opposing hemisphere compared to the first episode; in 1 case, a shift in the type of bleeding, such as from SAH with IVH to ICH with IVH, was observed.
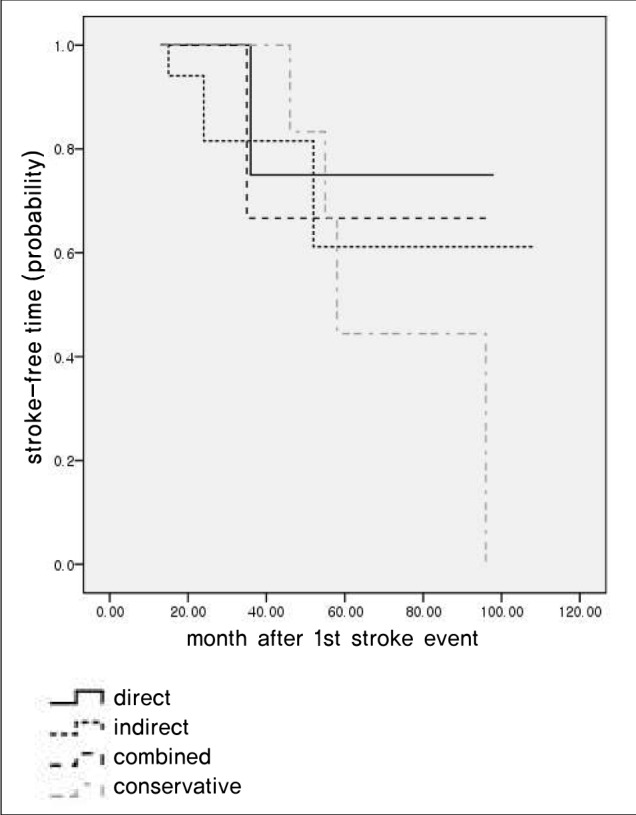
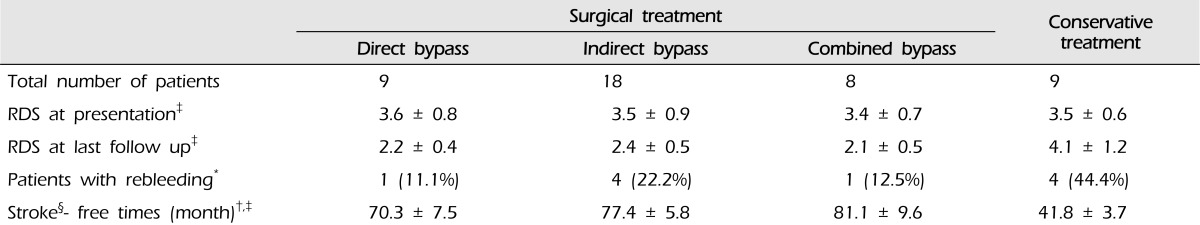
Patients were tracked for 12 to 105 months (mean: 55.4 months). Among 35 patients with revascularization surgery, 29 patients (82.9%) had stabilization of symptoms with no further episodes during the observation period. Six of 35 patients (17.1%) had recurrent episodes of hemorrhagic symptoms after revascularization surgery. In contrast, of 9 patients in the conservative treatment group, 4 (44.4%) experienced recurrent hemorrhagic episode. The frequency of new hemorrhagic events was lower in the revascularization group than the conservative treatment group. There was no significant difference between the groups (p = 0.101, χ2 test). The frequency of hemorrhagic events following each treatment modality was as follows: 1 of 9 patients (11.1%) treated with direct bypass (p = 0.06, χ2-test), 4 of 18 patients (22.2%) treated with indirect bypass (p = 0.22, χ2-test), and 1 of 8 patients (12.5%) treated with combined bypass (p = 0.18, χ2-test). No statistical difference was observed between treatment modalities and conservative treatment (Table 3). According to Kaplan-Meier plots of stroke free time, patients with revascularization surgery remained stroke free longer than conservatively treated patients. The mean stroke free times of patients in the direct bypass group were 70.3 ± 7.5 months, 77.4 ± 5.8 months in the indirect bypass group, 81.1 ± 9.6 months in the combined bypass group, and 41.8 ± 3.7 months in the conservative treatment group. There was no statistical difference (p = 0.09) between revascularization and conservative treatment groups (Fig. 1).
Clinical status at the end of the study was assessed using the RDS.21) Among 35 patients who underwent revascularization surgery, 22 patients (62.9%) had improvement of the RDS scores at last follow-up. According to the bypass methods, the RDS score for the 9 patients with direct bypass improved from 3.6 ± 0.8 to 2.2 ± 0.4, from 3.5 ± 0.9 to 2.4 ± 0.5 in the 18 patients with indirect bypass, and from 3.4 ± 0.7 to 2.1 ± 0.6 in the 8 patients with combined surgery (p < 0.05). The RDS score for the 9 patients with conservative treatment changed from 3.5 ± 0.6 to 4.1 ± 1.2 (p > 0.05). The RDS score improved significantly in the revascularization surgery group, while no improvement was observed in the conservative treatment group. Between bypass methods, no significant difference was observed in degree of improvement. A second hemorrhagic event resulted in 7 of 10 patients experiencing worsening of clinical symptoms. Among the 7 patients, 2 patients (28.6%) died, 2 (28.6%) deteriorated to a persistent vegetative state, and 3 (42.9%) were severely disabled.
Clinical complications were divided into transient neurological deficits and permanent neurological deficits. In direct bypass group, perioperative neurological complications occurred in 2 of 9 patients (22.2%). For the indirect bypass group, it was 3 out of 18 patients (16.7%), which included 2 transient and 1 permanent neurological deficit from cerebral infarct. In the combined group, 1 of 9 patients (11.1%) experienced transient neurological deficit. Perioperative neurological complications tend to be slightly high in the direct group, but there is no significant difference among bypass groups statistically (p = 0.97, linear-by-linear association). One permanent neurological deficit was related to ipsilateral cerebral infarction. No reperfusion-induced hemorrhage occurred. Perioperative non-neurological complications such as delayed wound healing, wound infection or subdural fluid collection occurred in 1 patient in the direct group, 2 patients in the indirect group and 1 patient in the combined group.
In 35 patients with revascularization surgery, a postoperative angiogram was obtained for all patients. The postoperative 6 vessels angiographic changes were as follows: direct bypass was good in 6 patients (66.7%), moderate in 2 patients (22.2%), and poor in 1 patient (11.1%). Indirect bypass was good in 5 patients (27.8%), moderate in 7 patients (38.9%), and poor in 6 patients (33.3%). Combined bypass was good in 5 patients (62.5%), moderate in 2 patients (25%), and poor in 1 patient (12.5%). Comparisons of angiographic changes according to revascularization surgery type showed 2.56 ± 0.7 after direct bypass, 1.8 ± 0.6 after indirect bypass, and 2.76 ± 0.6 in combined bypass (Table 4). More significant decrease of moyamoya vessels and increase of neovascularization were observed in direct/combined bypass groups compared to indirect groups (p < 0.05).
Moyamoya disease is a progressive, occlusive disease of the cerebral vasculature with particular involvement of the circle of Willis that affects more those of young age.23)27)
The clinical symptoms of MMD relate directly to abnormal vasculature, known as Moyamoya vessels.5) In children it tends to cause recurrent cerebral ischemic attacks or seizures. In adults it tends to cause intracranial hemorrhage.17) The prevalence of hemorrhage is reported to be greater than 60% in adults, much higher than the 10% seen in children.6) The reason for higher prevalence in adults is not known. However, the difference may be a result of the stability of systemic hemodynamics between adult and pediatric patients, as flexibility of moyamoya vessels might be higher in children.17) In hemorrhagic MMD, whether bypass surgery would prevent recurrent hemorrhagic attack is an important debate, as recurrent hemorrhagic attacks interfere with a good long-term prognosis. According to Kobayashi et al., in hemorrhagic moyamoya patients recurrent hemorrhagic attack long after the initial hemorrhage is not uncommon.14) After rebleeding, the chance of good recovery dropped from 45.5% to 21.4%, and the mortality rate increased from 6.8% to 28.6%. Saeki et al. observed that rebleeding is usually the same for the type of initial hemorrhage (IVH or ICH) and occurs at a different site, even on the contralateral hemisphere.21) That the type and site of hemorrhage changes in subsequent rebleeding presents a major challenge in prevention of recurrent hemorrhage. Kawaguchi et al. statistically confirmed that direct bypass in patient with hemorrhagic MMD may prevent the recurrent hemorrhage and ischemic stroke and recommended direct bypass over indirect bypass or conservative treatment for prevention of future stroke events.12)
In our study, 6 of 35 patients (17.1%) had recurrent episodes of hemorrhagic symptoms after revascularization surgery. In contrast, of 9 patients with conservative treatment, 4 patients (44.4%) experienced recurrent hemorrhagic attacks. However, as indicated in our results, we found the risk of rebleeding tends to be lower in the revascularization group than the conservative treatment group. Unfortunately, even a long observation period of 13 years failed to reveal a relation between surgical treatment modalities and the risk of rebleeding. A major cause for this lack of statistical association is that the subjects of this study all came from a single institution, which made the already limited number of cases even smaller. Additionally, we found it difficult to calculate bypass surgery's preventive effect on rebleeding based on past cases while taking account of various biases, such as adaptation to surgery, strict surgical indication in individual cases, and surgical methods. Another cause that has been postulated is that although direct and combined bypass supply an immediate blood flow with good clinical outcome, supposedly because of progressive occlusion of the recipient (moyamoya) artery, the direct anastomosis alone failed to maintain enduring filling of the MCA.1)8)18) These findings explain why our study, even after 13 years of observation, did not find a significant association between surgical treatment modalities and risk of recurrent hemorrhage.
The goal of revascularization surgery in patients with MMD is to prevent intracranial hemorrhage by reducing the hemodynamic stress and the number of moyamoya vessels. Generally, moyamoya vessels diminished only in only 25-60% of adults with MMD after revascularization surgery, whereas in pediatric cases, significant change in moyamoya vessels was seen in 100%.14)17) Houkin et al. studied 35 adult moyamoya patients and found that moyamoya vessels decreased only 25% in patients after revascularization.6) Kawaguchi et al. reported that direct surgery is superior to indirect bypass surgery to reduce the extent and number of moyamoya vessels.12) In our series, we analyzed the collateral formation and the decrease in the number of moyamoya vessels on postoperative 6 vessel angiography in patients with revascularization surgery. Direct and combined bypass is more effective to reduce the number of moyamoya vessels than indirect bypass, statistically significant (p < 0.05). Why indirect revascularization in adult cases is not as effective remains unclear. We postulated that the extent of the postoperative collateral circulation seemed to be limited in indirect bypass because the operative field was usually made along the course of the parietal branch of the STA, compare with combined bypass which covered the widest surgical field for revascularization.
Kobayashi et al. reported that the second bleeding episode frequently occurred at a different site, even on the alternate side of the brain.14) Based on this finding, a rupture of a specific vulnerable point did not lead to rebleeding, but rather resulted from diffuse weak points of moyamoya vessels close to the lateral ventricle. Mainly because of this randomness and unpredictability, the effect of revascularization surgery remains uncertain.
In our series, among 10 patients who had recurrent episodes of hemorrhagic symptoms, 4 patients (40%) experienced a recurrent intracranial hemorrhage with changes in the type of bleeding and hemisphere during the follow-up period. It seems that revascularization surgery can supply blood flow in ischemic brain and promote perfusion, and as a result reduce the abnormal moyamoya vessels around the lateral ventricles.11)13)19) This is of great importance when considering the strategy of bypass surgery. In earlier years, we performed bypass to only the symptomatic hemisphere. More studies are demonstrating that rebleeding changes the type of bleeding and the hemisphere. Therefore, the recommended treatment for hemorrhagic MMD is to perform prophylactic bypass surgery bilaterally, maximally expose the brain surface, and use potential tissue, such as STA, galea pedicle, and dura mater, as widely as possible as a source of revascularization.
Some limitations are present in our study. First of all, ours was not a prospective randomized study and treatment assignments were not random, which could lead to selection bias. Lack of generalizability or external validity could also be a problem as our subjects are from a single institution. Secondly, the postoperative evaluation period that includes analysis of angiographic and clinical outcomes were not constant in all patients. This presented difficulties in comparing with other treatment modalities. Thirdly, there were no strict indications of which bypass was applied for individual cases in our present study. As of today, we have adopted exclusive use of direct and combined methods whenever possible, as more data showing their effectiveness have accumulated and more advanced surgical methods have developed. We performed the indirect bypass surgery only as an alternative method when no adequate recipient artery for STA-MCA bypass existed.
From the results of our study, although there is still no clear evidence that revascularization surgery completely excludes chance of rebleeding in patients with hemorrhagic MMD, a preventive effect is expected. We statistically confirmed that both direct and combined bypass were much more effective for achieving a good extent of revascularization and decrease of moyamoya vessels than indirect bypass. To sum up these results, we cautiously recommend direct and combined bypass as a choice of treatment in hemorrhagic MMD over indirect bypass. A long-term, large, prospective, randomized clinical trial is needed to clarify which surgical method is best in patients with hemorrhagic MMD.
References
1. Asfora WT, West M, McClarty B. Angiography of encephalomyosynangiosis and superficial temporal artery to middle cerebral artery anastomosis in moyamoya disease. AJNR Am J Neuroradiol. 1993; Jan-Feb. 14(1):29–30. PMID: 8427106.
2. Fukui M. Research Committee on Spontaneous Occlusion of the Circle of Willis (Moyamoya Disease) of the Ministry of Health and Welfare, Japan. Guidelines for the diagnosis and treatment of spontaneous occlusion of the circle of Willis ('Moyamoya' disease). Clin Neurol Neurosurg. 1997; 10. 99(Suppl 2):S238–S240. PMID: 9409446.

3. Golby AJ, Marks MP, Thompson RC, Steinberg GK. Direct and combined revascularization in pediatric moyamoya disease. Neurosurgery. 1999; 7. 45(1):50–58. discussion 58-60. PMID: 10414566.

4. Han DH, Nam DH, Oh CW. Moyamoya disease in adults: Characteristics of clinical presentation and outcome after encephalo-duro-arterio-synangiosis. Clin Neurol Neurosurg. 1997; 10. 99(Suppl 2):S151–S155. PMID: 9409427.
5. Horowitz M, Yonas H, Albright AL. Evaluation of cerebral blood flow and hemodynamic reserve in symptomatic moyamoya disease using stable xenon-CT blood flow. Surg Neurol. 1995; 9. 44(3):251–261. discussion 262. PMID: 8545777.

6. Houkin K, Kamiyama H, Abe H, Takahashi A, Kuroda S. Surgical therapy for adult moyamoya disease. Can surgical revascularization prevent the recurrence of intracranial hemorrhage? Stroke. 1996; 8. 27(8):1342–1346. PMID: 8711799.
7. Ikezaki K, Fukui M, Inamura T, Kinukawa N, Wakai K, Ono Y. The current status of the treatment for hemorrhagic type moyamoya disease based on a 1995 nationwide survey in Japan. Clin Neurol Neurosurg. 1997; 10. 99(Suppl 2):S183–S186. PMID: 9409433.

8. Kim H, Kim YW, Joo WI, Park HK, Joo JK, Lee KJ, et al. [Effect of direct bypass on the prevention of hemorrhage in patients with hemorrhagic type of moyamoya disease]. Korean J Cerebrovasc Surg. 2007; 3. 9(1):14–19. Korean.
9. Karasawa J, Touho H, Ohnishi H, Miyamoto S, Kikuchi H. Cerebral revascularization using omental transplantation for childhood moyamoya disease. J Neurosurg. 1993; 8. 79(2):192–196. PMID: 8331399.

10. Karasawa J, Touho H, Ohnishi H, Miyamoto S, Kikuchi H. Long-term follow-up study after extracranial-intracranial bypass surgery for anterior circulation ischemia in childhood moyamoya disease. J Neurosurg. 1992; 7. 77(1):84–89. PMID: 1607976.

11. Kashiwagi S, Yamashita T, Katoh S, Kitahara T, Nakashima K, Yasuhara S, et al. Regression of moyamoya vessels and hemodynamic changes after successful revascularization in childhood moyamoya disease. Acta Neurol Scand Suppl. 1996; 166:85–88. PMID: 8686450.
12. Kim DS, Yoo DS, Huh PW, Kim JK, Cho KS, Kang JK. Recent surgical treatment of moyamoya disease. J Korean Neurosurg Soc. 2001; 6. 30:800–804.
13. Kawaguchi T, Fujita S, Hosoda K, Shose Y, Hamano S, Iwakura M, et al. Multiple burr-hole operation for adult moyamoya disease. J Neurosurg. 1996; 3. 84(3):468–476. PMID: 8609560.

14. Kobayashi E, Saeki N, Oishi H, Hirai S, Yamaura A. Long-term natural history of hemorrhagic moyamoya disease in 42 patients. J Neurosurg. 2000; 12. 93(6):976–980. PMID: 11117870.
15. Matsushima Y, Fukai N, Tanaka K, Tsuruoka S, Inaba Y, Aoyagi M, et al. A new surgical treatment of moyamoya disease in children: A preliminary report. Surg Neurol. 1981; 4. 15(4):313–320. PMID: 7245020.

16. Matsushima Y, Inaba Y. Moyamoya disease in children and its surgical treatment. Introduction of a new surgical procedure and its follow-up angiograms. Childs Brain. 1984; 11(3):155–170. PMID: 6723433.
17. Morimoto M, Iwama T, Hashimoto N, Kojima A, Hayashida K. Efficacy of direct revascularization in adult moyamoya disease: Haemodynamic evaluation by positron emission tomography. Acta Neurochir (Wien). 1999; 141(4):377–384. PMID: 10352747.

18. Nakagawa Y, Abe H, Sawamura Y, Kamiyama H, Gotoh S, Kashiwaba T. Revascularization surgery for moyamoya disease. Neurol Res. 1988; 3. 10(1):32–39. PMID: 2899853.

19. Okada Y, Shima T, Nishida M, Yamane K, Yamada T, Yamanaka C. Effectiveness of superficial temporal artery-middle cerebral artery anastomosis in adult moyamoya disease: Cerebral hemodynamics and clinical course in ischemic and hemorrhagic varieties. Stroke. 1998; 3. 29(3):625–630. PMID: 9506603.
20. Rankin J. Cerebral vascular accidents in patients over the age of 60. II. Prognosis. Scott Med J. 1957; 5. 2(5):200–215. PMID: 13432835.

21. Saeki N, Nakazaki S, Kubota M, Yamaura A, Hoshi S, Sunada S, et al. Hemorrhagic type moyamoya disease. Clin Neurol Neurosurg. 1997; 10. 99(Suppl 2):S196–S201. PMID: 9409437.

22. Scott RM, Smith JL, Robertson RL, Madsen JR, Soriano SG, Rockoff MA. Long-term outcome in children with moyamoya syndrome after cranial revascularization by pial synangiosis. J Neurosurg. 2004; 2. 100(2 Suppl Pediatrics):142–149. PMID: 14758941.

23. Suzuki J, Kodama N. Moyamoya disease- A review. Stroke. 1983; Jan-Feb. 14(1):104–109. PMID: 6823678.
24. Suzuki J, Takaku A. Cerebrovascular "moyamoya" disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol. 1969; 3. 20(3):288–299. PMID: 5775283.
25. Ueki K, Meyer FB, Mellinger JF. Moyamoya disease: The disorder and surgical treatment. Mayo Clin Proc. 1994; 8. 69(8):749–757. PMID: 8035631.

26. Wanifuchi H, Takeshita M, Izawa M, Aoki N, Kagawa M. Management of adult moyamoya disease. Neurol Med Chir (Tokyo). 1993; 5. 33(5):300–305. PMID: 7687036.

27. Yoshida Y, Yoshimoto T, Shirane R, Sakurai Y. Clinical course, surgical management, and long-term outcome of moyamoya patients with rebleeding after an episode of intracerebral hemorrhage: An extensive follow-up study. Stroke. 1999; 11. 30(11):2272–2276. PMID: 10548656.
Fig. 1
Kaplan-Meier plots of stroke-free time demonstrates that patients with revascularization surgery had longer stroke-free times than those with conservative treatment, but there was no statistical difference (p = 0.09).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download