Abstract
Objective
This study investigated the clinical and angiographic outcomes of treatment with stent-assisted coil embolization using the Solitaire AB stents for wide-necked intracranial aneurysms.
Methods
From October 2010 to December 2011, 22 patients with aneurysms were treated with the Solitaire AB stent. One patient with a dissecting aneurysm was excluded, thus 21 patients with 21 wide-necked saccular aneurysms were included in this study. The technical success rate, procedure-related complications, initial and follow-up angiographic results, and clinical outcomes were retrospectively collected.
Results
The locations of aneurysms were as follows: paraclinoid in 14, distal internal carotid artery in 4, and vertebral artery in 3 patients. All aneurysms were unruptured and less than 10 mm-sized. The mean dome-to-neck ratio of the aneurysms was 1.00 (range: 0.45-1.81). The mean follow-up duration was 12.1 (7-15) months after the initial procedure. The technical success rate was 21 (95.5%) of 22 patients with aneurysms. Fortunately, there were no procedure-related complications. Follow-up angiography showed that the rate of complete occlusion was 57.1%, neck remnants 38.1%, and incomplete occlusion 4.8%.
The use of self-expanding stents has revolutionized endovascular treatment (EVT) of wide-necked aneurysms.11) These stents provide support to minimize the risk of coil herniation into the parent vessel, potentially provide a scaffold for orifice endothelialization and permit increased packing density of the aneurysm.16)18) They also create flow diversion.11)
Self-expandable stents, such as the Neuroform and Enterprise,1)14) are widely used in the treatment of wide necked aneurysms. Initial angiographic results indicate that the use of the Neuroform stents result in complete occlusion rates of 17-94.4% and Enterprise stents 6.9%.5)11) Navigation or deployment inability rates of 4-14% have been oserved with the use of the Neuroform stent, and distal migration rates of 1.4% with the Enterprise stent.7)10)11)15) The Solitaire AB stent (ev3, Irvine, CA, USA) was recently approved to treat intracranial aneurysms for these purposes.
The Solitaire AB stent is circular and cylindrical and is connected to a push-wire that is electrically detached after full deployment, allowing retrieval or repositioning of stent, superior to other stents.8)
This study retrospectively investigated the clinical and angiographic results of patients treated with stent-assisted coil embolization using Solitaire AB stent for wide-necked intracranial aneurysms.
From October 2010 to December 2011, 61 patients with 62 aneurysms underwent EVT of intracranial aneurysms at our institution. Among these patients, 22 were treated with stent-assisted coil embolization using Solitaire AB stents. One patient with a dissecting aneurysm was excluded. Thus, this study included 21 patients (male: female ratio, 4:17; mean age, 56.1 years; range, 38-70 years) with 21 unruptured wide-necked aneurysms. Aneurysm size and morphology were measured using digital subtraction angiography with 3-dimensional rotational imaging. Wide-necked aneurysms were defined by a neck width of ≥ 4 mm or a dome-to-neck ratio of < 2.
Treatment modality was decided by consensus of a neurosurgeon and neuro-interventionist considering patient co-morbidities, clinical status, and surgical feasibility. Solitaire stents were chosen according to the surgeon's preference with respect to anatomic variations. All procedures were performed under general anesthesia. A 6-Fr or 7-Fr guiding catheter was positioned in the internal carotid artery for anterior circulation aneurysms or in the vertebral artery for posterior circulation aneurysms. Stent-assisted coil embolization was performed using the "jailing" technique in all cases.6) Solitaire stents were deployed on the parent vessels across the neck of the aneurysms through a Rebar 0.018 or 0.027 inch microcatheter (ev3, Irvine, CA, USA). Patients were pre-medicated for 7 days before surgery with aspirin (100 mg/day) and clopidogrel (75 mg/day). After surgery, the patients were prescribed clopidogrel 75 mg/day for 3 months and aspirin 100 mg/day for 12 months or for life. During the procedure, patients were heparinized to maintain an activated clotting time of > 250 seconds.
The angiographic results were evaluated by 2 independent investigators and categorized according to the Raymond-Roy classification as follows:9) Class I (no filling of the aneurysm or dome), Class II (residual filling of the neck, but not the dome), and Class III (residual filling of the neck and dome). Clinical outcomes were assessed based on the modified Rankin Scale (mRS). The clinical outcomes, angiographic results, procedure-related complications, and technical success rate were reviewed.
We performed the stent-assisted coil embolization using Solitaire AB stent in all 21 patients. There were 4 males and 17 females. The mean age of these patients was 56.1 year (38-70). The locations of aneurysms were as follows: paraclinoid in 14, distal ICA in 4, and vertebral artery in 3 patients. Eighteen aneurysms were located in the anterior circulation, and 3 were located in the posterior circulation. All aneurysms were classified as small (< 10 mm) and unruptured. The mean dome-to-neck ratio of the aneurysms was 1.00 (range: 0.45-1.81). Nine aneurysms had a neck width of ≥ 4 mm and 11 had a dome-to-neck ratio of < 1. During the procedures, there were no complications related to delivery or deployment of the Solitaire stent. In 2 cases, stents were repositioned after full deployment. Follow-up angiography was performed in 18 of 21 patients between 7 and 15 months (mean, 12.1 months) after the procedure, and clinical follow-up was performed between 8 and 25 months (mean, 17.8 months). Follow-up angiography was not performed on 3 patients who were lost to follow up.
Immediate post-embolization angiographic results were classified as Class I in 12 patients (57.1%), Class II in 8 patients (38.1%), and Class III in 1 patient (4.8%). Follow-up angiographic results were obtained in 18 of 21 patients (85.7%). These results were classified as Class I in 16 patients (88.9%) and Class II in 2 patients (11.1%). Only 1 patient (patient No. 10) showed recanalization of the aneurysm neck on follow-up angiography. No stent migration or in-stent stenosis was seen on follow-up angiography.
With respect to clinical outcomes, fortunately, all of the patients achieved a mRS score of 0 during the follow-up period. The data and outcomes of all 21 patients are summarized in Table 1.
Stent-assisted coil embolization was broadly considered effective for the treatment of wide-necked intracranial aneurysms.1)13) Self-expandable stents, such as the Neuroform and Enterprise,1)14) are often used in the treatment of wide necked aneurysms. Their efficacy and safety in improving anatomical results as well as low procedure-related morbidity and mortality have been validated.1)13)
Solitaire AB stents are currently used in the treatment of intracranial aneurysms. Solitaire stents have a navigability advantage compared with other stent systems available in the intracranial lesions. They are fully retrievable and can be repositioned even after full deployment. Experiences with the Neuroform stent demonstrated rates of 4-14% for the inability to navigate or deploy, 8-17.8% for inaccurate deployment, and 24-31% for deployment difficulty.7)10)15) The Enterprise stent demonstrated rates of 3% for the inability to navigate or deploy.2) Klisch J et al.8) reported deployment failure rates of 4.1% for the Solitaire stent. In our case, despite very tortuous vessels, we did not find difficulty and failure in navigation and stent deployment (Fig. 1).
A high degree of navigability is associated with excellent flexibility and an easy delivery system through Rapid Transit or Rebar 0.018 or 0.027 inch microcatheters.8)
We had experience repositioning Solitaire AB stents, which are fully retrievable and detachable. In our case, the stent was deployed and coil insertion was performed. However, we detected that 1 stent marker was outside the vessel. We thought that the stent marker might be in the small perforator. Therefore, we pulled the stent pusher wire out slightly. Finally, the stent was repositioned and the marker was inside the vessel (Fig. 2). During the packing of coiling within the aneurysm with jailing technique, if microcatheter kick back occurs into the parent artery, a Solitaire AB stent can be recaptured within another microcatheter. After the selection of aneurysm, Solitaire stent can be re-deployed. In the case of branch vessel occlusion observed on angiography during the procedure, the stent is also retrieved and repositioned.
Like another self-expandable stents such as Neuroform or Enterprise, in our study, Solitaire stents demonstrated successful occlusion rates on immediate postoperative angiographies. Immediate angiographic results reported with the use of Neuroform stents vary, with Class I rates of 17-94.4%.5) Lee et al.11) reported the results of 289 patients who underwent Enterprise stent-assisted coiling as follows: 6.9% in Class I, 64% in Class II, and 29.1% in Class III. Izar et al.7) documented the occlusion rates for comparison between Neuroform stent and Enterprise stent as follows: Class I (42.8%/30.95%), Class II (40.5%/38.1%), and Class III (13.3%/30.95%). Zhang J et al.19) noted the rates of 31 aneurysms treated with Solitaire stents as follows: 26 aneurysms (83.9%) in Class I, 3 aneurysms (9.7%) in Class II, and 2 aneurysms (6.4%) in Class III. Klisch J et al.8) observed the following occlusion rates of 43 aneurysms treated using Solitaire stents: 23 aneurysms (53.5%) in Class I, 18 aneurysms (42%) in Class II, and 2 aneurysms (4.7%) in Class III.
In this study, angiographic results were classified as Class I in 12 patients (57.1%), Class II in 8 patients (38.1%), and Class III in 1 patient (4.8%). These occlusion rates are similar to those reported in a series of aneurysm coil embolization using Solitaire stents, although further evaluation with more patients is needed.
The intracranial stent induces progressive occlusion via flow diversion, facilitating intra-aneurysmal endothelial growth.10) This study improved anatomical results with progressive occlusion in 6 patients (28.6%) at follow-up periods ranging from 7 to 16 months. Specifically, 5 patients converted from Class II to Class I, while 1 patient converted from Class III to Class II. Fiorella et al.3) and Maldonado et al.13) pointed out that the Neuroform stent improved anatomical results, with progressive thrombosis in 52% and 55% of the respective cases. Izar et al.7) noted a 36% progressive occlusion rate with Enterprise stent-assisted coil embolization. Yavuz et al.17) observed an 87.5% progressive occlusion rate with SOLO stent (first generation Solitaire AB stent) assisted coil embolization. Further analysis with long term follow-up is needed to support these observations.
In this study, no in-stent stenosis was observed during the follow-up period. Fiorella et al.4) saw rates of 5.8% for in-stent stenosis using the Neuroform stent. The Enterprise stent had in-stent stenosis rates of 8.6-25% in the treatment of aneurysms.12)
In addition, no stent migration was observed, possibly because of the stronger radial force of the Solitaire stent (0.0106 N/mm of stent length) compared to other stents.8)
Reported recanalization rate of aneurysms treated with Solitaire stents is 6.5%.19) The Neuroform stent had recanalization rates of 1.3-5.8% and those of the Enterprise stent were 8.7-28.6%.7)11)14) In this study, except for 3 patients who were lost to follow-up, 1 of 18 (5.6%) aneurysms recanalized, confirming total occlusion (Class I) on immediate postoperative angiography.
This study has some limitations. We did not have a control group, so we compared the results and outcome of this study to those of previously published studies. In addition, data were collected retrospectively and the number of patients was limited. The follow-up periods may not be long enough to result in any definitive conclusion. Therefore, longer follow-up and more clinical and angiographic data are needed to determine the efficacy and safety of Solitaire stent-assisted coil embolization in wide-necked aneurysm cases.
References
1. Fargen KM, Hoh BL, Welch BG, Pride GL, Lanzino G, Boulos AS, et al. Long-term results of enterprise stent-assisted coiling of cerebral aneurysms. Neurosurgery. 2012; 8. 71(2):239–244. discussion 244. PMID: 22472556.

2. Ferrell AS, Golshani K, Zomorodi A, Smith TP, Britz GW. Improved delivery of the Neuroform 3 stent: Technical note. J Neurointerv Surg. 2012; 7. 4(4):287–290. PMID: 21990486.

3. Fiorella D, Albuquerque FC, Deshmukh VR, McDougall CG. Usefulness of the Neuroform stent for the treatment of cerebral aneurysms: Results at initial (3-6-mo) follow-up. Neurosurgery. 2005; 6. 56(6):1191–1201. discussion 1201-2. PMID: 15918935.

4. Fiorella D, Albuquerque FC, Woo H, Rasmussen PA, Masaryk TJ, McDougall CG. Neuroform in-stent stenosis: Incidence, natural history, and treatment strategies. Neurosurgery. 2006; 7. 59(1):34–42. discussion 34-42. PMID: 16823298.

5. Gu DQ, Zhang X, Luo B, Long XA, Duan CZ. The effect of Neuroform stent-assisted coil embolization of wide-necked intracranial aneurysms and clinical factors on progressive aneurysm occlusion on angiographic follow-up. J Clin Neurosci. 2013; 2. 20(2):244–247. PMID: 23201094.

6. Hong B, Patel NV, Gounis MJ, DeLeo MJ 3rd, Linfante I, Wojak JC, et al. Semi-jailing technique for coil embolization of complex, wide-necked intracranial aneurysms. Neurosurgery. 2009; 12. 65(6):1131–1138. discussion 1138-9. PMID: 19934972.

7. Izar B, Rai A, Raghuram K, Rotruck J, Carpenter J. Comparison of devices used for stent-assisted coiling of intracranial aneurysms. PLoS one. 2011; 6(9):e24875. PMID: 21966374.

8. Klisch J, Clajus C, Sychra V, Eger C, Strasilla C, Rosahl S, et al. Coil embolization of anterior circulation aneurysms supported by the Solitaire AB Neurovascular Remodeling Device. Neuroradiology. 2010; 5. 52(5):349–359. PMID: 19644683.

9. Kwon HJ, Kwon Y. Embolization of cerebral aneurysms with stent and detachable platinum coils-Single center experience. J Korean Soc Intravasc Neurosurg. 2006; 1:1–6.
10. Lee JI, Ko JK, Choi BK, Choi CH. In-stent stenosis of stent-assisted coil embolization of the supraclinoid internal carotid artery aneurysm. J Korean Neurosurg Soc. 2012; 6. 51(6):370–373. PMID: 22949968.

11. Lee SJ, Cho YD, Kang HS, Kim JE, Han MH. Coil embolization using the self-expandable closed-cell stent for intracranial saccular aneurysm: A single-center experience of 289 consecutive aneurysms. Clin Radiol. 2013; 3. 68(3):256–263. PMID: 23017739.

12. Lylyk P, Ferrario A, Pasbon B, Miranda C, Doroszuk G. Buenos Aires experience with the Neuroform self-expanding stent for the treatment of intracranial aneurysms. J Neurosurg. 2005; 2. 102(2):235–241. PMID: 15739550.

13. Maldonado IL, Machi P, Costalat V, Mura T, Bonafe A. Neuroform stent-assisted coiling of unruptured intracranial aneurysms: Short- and midterm results from a single-center experience with 68 patients. AJNR Am J Neuroradiol. 2011; 1. 32(1):131–136. PMID: 20966053.

14. Santillan A, Greenberg E, Patsalides A, Salvaggio K, Riina HA, Gobin YP. Long-term clinical and angiographic results of Neuroform stent-assisted coil embolization in wide-necked intracranial aneurysms. Neurosurgery. 2012; 5. 70(5):1232–1237. discussion 1237. PMID: 22095221.

15. Wakhloo AK, Mandell J, Gounis MJ, Brooks C, Linfante I, Winer J, et al. Stent-assisted reconstructive endovascular repair of cranial fusiform atherosclerotic and dissecting aneurysms: Long-term clinical and angiographic follow-up. Stroke. 2008; 12. 39(12):3288–3296. PMID: 18772450.
16. Wanke I, Doerfler A, Schoch B, Stolke D, Forsting M. Treatment of wide-necked intracranial aneurysms with a self-expanding stent system: Initial clinical experience. AJNR Am J Neuroradiol. 2003; Jun-Jul. 24(6):1192–1199. PMID: 12812954.
17. Yavuz K, Geyik S, Pamuk AG, Koc O, Saatci I, Cekirge HS. Immediate and midterm follow-up results of using an electrodetachable, fully retrievable SOLO stent system in the endovascular coil occlusion of wide-necked cerebral aneurysms. J Neurosurg. 2007; 7. 107(1):49–55. PMID: 17639873.

18. Yoon PH, Ahn JY, Kim SH, Choi EW. Endovascular treatment of wide-necked aneurysms with a stent and detachable coils. Korean J Cerebrovasc Neurosurg. 2004; 1. 6(1):31–37.
19. Zhang J, Lv X, Yang J, Wu Z. Stent-assisted coil embolization of intracranial aneurysms using Solitaire stent. Neurol India. 2012; May-Jun. 60(3):278–282. PMID: 22824683.

Fig. 1
Patient No. 11: A 60-year-old woman with unruptured aneurysm of a tortuous left distal internal carotid artery (ICA) is treated with coil embolization. (A) The aneurysm is shown on left ICA angiography. (B) A Solitaire stent is positioned at the left distal ICA (white arrow: proximal and distal stent marker). (C) Immediate left ICA angiography after embolization shows no contrast filling of the aneurysmal neck or dome. (D) Twelve months after embolization, angiography shows no recanalization.
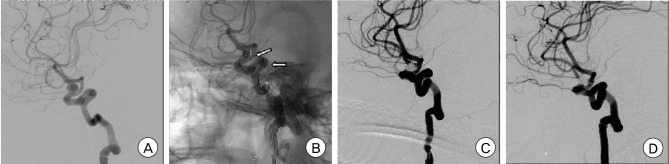
Fig. 2
Patient No.8: A 55-year-old woman with an unruptured aneurysm of the left distal internal carotid artery (ICA) was treated with coil embolization by repositioning the stent. (A) ICA angiography shows that the stent marker was outside the vessel. (B) The stent was pulled out slightly and the stent marker was moved back inside the vessel.
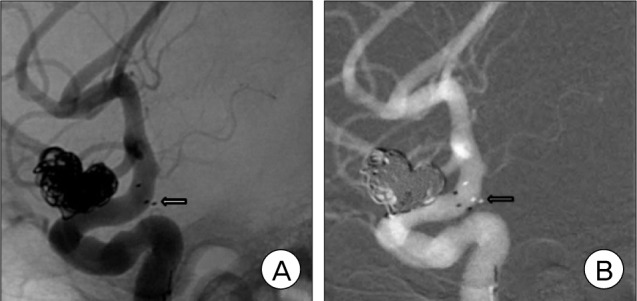
Table 1
Demographic data and outcomes of the 21 patients treated with Solitaire AB stent-assisted coil embolization.
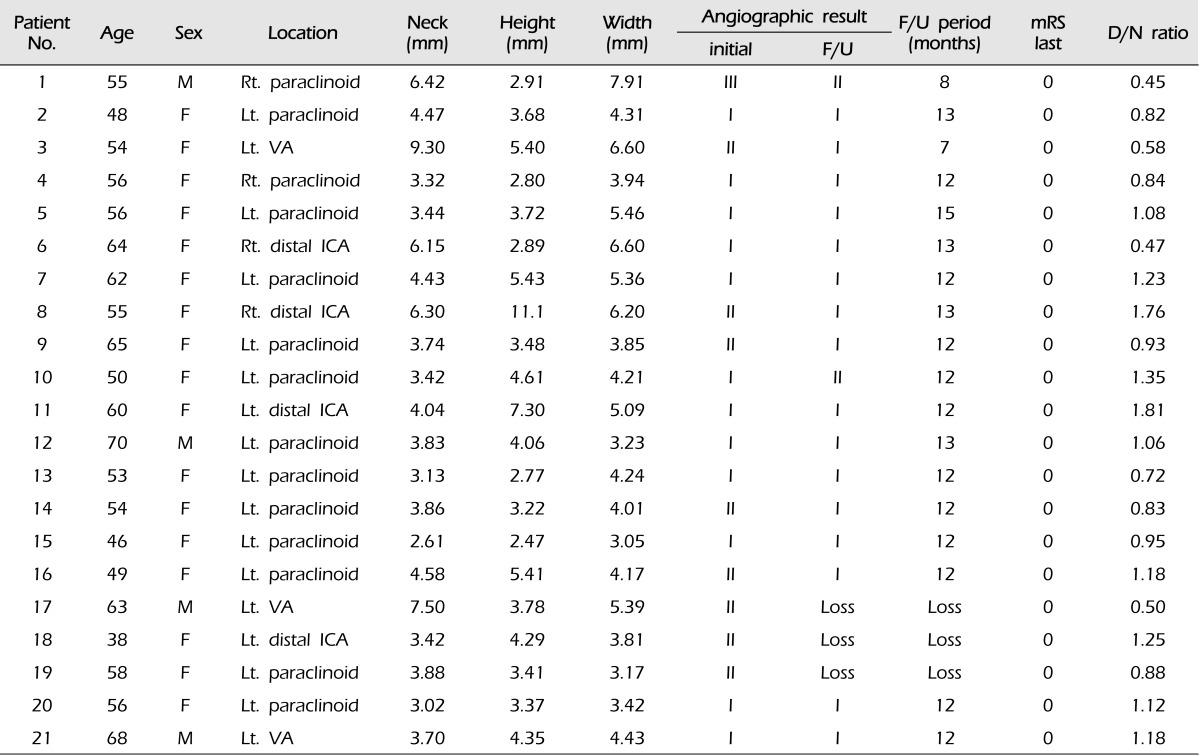
Width: the short axis dome measurement of a cylindrical aneurysm, the dome/neck ratio is based on the height/neck ratio, Class I: no filling of the aneurysm neck or dome, Class II: residual filling of the neck but not the dome, Class III: residual filling of the neck and dome. D= dome; N= neck; F/U= follow-up; ICA= internal carotid artery; mRS= modified Rankin Scale; VA= vertebral artery; Lt= left; Rt= right.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download