Abstract
Objective
We have observed, anecdotally, that the incidence of primary spontaneous intracerebral hemorrhage (sICH), as well as spontaneous subarachnoid hemorrhage, varies in accordance with seasonality and meteorological conditions. This retrospective single-hospital-based study aimed to determine the seasonality of sICH and the associations, if any, between the occurrence of sICH and meteorological parameters in Incheon city, which is a northwestern area of South Korea.
Methods
Electronic hospital data on 708 consecutive patients admitted with primary sICH from January 2008 to December 2010 was reviewed. Traumatic and various secondary forms of ICHs were excluded. Average monthly admission numbers of sICH were analyzed, in relation with the local temperature, atmospheric pressure, humidity, and daily temperature range data. The relationships between the daily values of each parameter and daily admission numbers of sICH were investigated using a combination of correlation and time-series analyses.
Results
No seasonal trend was observed in sICH-related admissions during the study period. Furthermore, no statistically significant correlation was detected between the daily sICH admission numbers and the meteorological parameters of temperature, atmospheric pressure and humidity. The daily temperature range tended to correlate with the number of daily sICH-related admissions (p = 0.097).
Spontaneous intracerebral hemorrhage (sICH) accounts for 8-13% of all strokes and can result from a wide spectrum of disorders, including hypertension. In addition, compared to ischemic stroke or subarachnoid hemorrhage (SAH), primary sICH is more likely to result in death or major disability.2)3)
Several primary risk factors of sICH have been identified, including high blood pressure (BP), tobacco use, use of some drugs and/or alcohol, old age, and female gender.7)12)19)24) However, the relationship between seasonal variation and/or meteorological parameters and spontaneous SAH (sSAH) is unclear, and a few studies have attempted to demonstrate an association between the incidence of sICH and seasonality and/or meteorological parameters.1)6)11)
The aim of this study was to determine if any of the meteorological parameters, such as local temperature, atmospheric pressure, humidity, and daily temperature range, influence the risk of sICH in Incheon metropolitan city, which occupies a wide area of the western seacoast and many islands in the northwestern region of South Korea. Concurrently, we tried to determine whether the risk of sICH was associated with seasonality.
We analyzed data of patients from a tertiary referral emergency center, which is the only level I regional emergency center in the northwestern area of South Korea. At this emergency center, almost all patients with acute sICH coming into this hospital's ER are admitted to the authors' department. The diagnosis of primary sICH was made by the universal standard methods. Electronic medical records and radiological findings for 708 consecutive patients admitted with a diagnosis of primary sICH from January 2008 to December 2010 were reviewed and analyzed. Secondary ICHs or those caused by trauma were excluded. Data on local temperature (℃), temperature range (℃), atmospheric pressure (hPa), and humidity (%) were collected with the help of Incheon Weather Station (latitude: 37°28'N, longitude: 126°37'E, elevation: 69 m).
The correlations between the estimated average monthly number of admissions due to sICH and local temperature, atmospheric pressure, humidity, and daily temperature range were estimated using autocorrelation analysis. The association of daily values of each weather parameter with the daily admission numbers of sICH was analyzed using a combination of correlation and time-series analyses. Autocorrelation analysis was used to measure the degree of self-correlation in the monthly admission numbers of sICH time series. The data were then analyzed statistically using SPSS 19 (IBM corp., Armonk, NY, USA).
Table 1 shows the demographic and clinical characteristics of the patients with sICH enrolled in the present study. Included were 708 patients (387 [54.7%] men, 321 [45.3%] women), with an average age of 58.4 ± 15.6 years. Among the established risk factors for sICH, hypertension (51.3%) and alcoholism (24.2%; alcohol consumption more than twice per week) were the 2 most common risk factors in our study population.
The association between the number of admissions due to sICH and season was not statistically significant (Fig. 1).
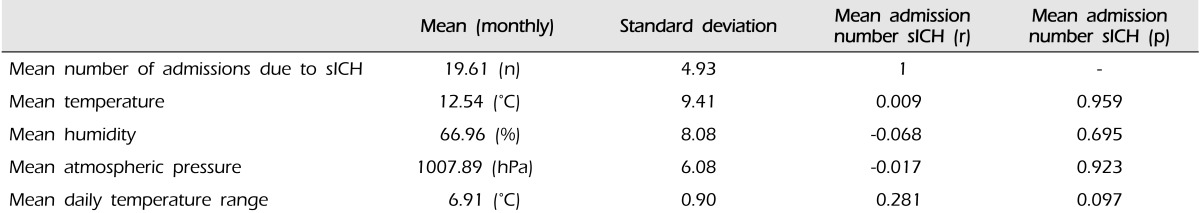
Fig. 2 shows the mean number of monthly admissions due to sICH during the study period. The time series of admissions shows a weak and rather irregular series of peaks and troughs, with no apparent annual or seasonal patterns. Results of autocorrelation analysis, which measured the degree of self-correlation in the monthly admissions due to sICH time series, are presented in Table 2 and Fig. 3.
Despite the findings of no seasonality or annually recurring patterns in the average monthly admissions due to sICH, the possibility that the weather can influence the average monthly sICH-related admissions cannot be excluded. Therefore, the association of changes in the local temperature, atmospheric pressure, humidity, and daily temperature range with changes in the average number of monthly admissions due to sICH, during the study period for 3 years, was separately measured for each weather parameter (Table 2, Fig. 3).
Fig. 3 has plots depicting the association between the monthly sICH admission numbers and each weather parameter, and Table 2 describes the correlation analysis between them.
The local temperature (correlation coefficient [r] = 0.009, p = 0.959), local atmospheric pressure (r = -0.017, p = 0.923), local humidity (r = -0.068, p = 0.695), and local daily temperature range (r = 0.281, p = 0.097) were not associated with monthly admissions due to sICH. However, although chance findings could not be excluded, there was a tendency for the daily temperature range to be correlated with the number of sICH-related admissions to some degree.
Primary sICH is defined as a non-traumatic abrupt onset of severe headache and altered level of consciousness and/or focal neurologic deficit associated with a focal collection of blood within the brain parenchyma, as observed on neuroimaging or autopsy. It is not caused by rupture of cerebral aneurysms, arteriovenous malformations, hemorrhagic conversion of a cerebral infarction, or other causes of secondary ICH. The widespread availability computed tomography (CT) resulted in a dramatic change in our understanding of the incidence and risk factors of sICH.21)
During the past decades, diurnal and seasonal variations in the onset of primary sICH have been examined in many community- and hospital-based studies.4)10)13)22)
More recently, Shin et al.19) reported in their single institute-based study that winter was the most common season for the occurrence of sICH. Inagawa12) also stated in his population-based study that winter was the most common season for sICH among men belonging to a subgroup of younger patients (age ≤ 69 years) and a hypertension-induced subgroup; however, there was no significant seasonal pattern in women. Contrary to these reports, the present study revealed that, although there was no significant difference, spring was the most common and winter was the least common season for monthly admissions due to sICH (Fig. 1). While the exact reason for this difference remains unknown, we presume that it is due to differences in regional climate, such as the daily temperature range, and risk factors for sICH in the enrolled patients in each study. We further hypothesize that the high temperature range is more influential than the low absolute ambient temperature, as it can cause hemodynamic instability and eventually lead to sICH.
BP, blood viscosity, serum lipid levels, sympathetic nervous system activity, blood clotting time, and fibrinogen levels are affected by season and weather and could alter the risks of a stroke.9) Our study partially supports the concept that changes in meteorological parameters drive the relationship between weather and sICH. In contrast to our finding of winter being the least common season for sICH-related admissions, cold exposure is thought to increase BP by activating the sympathetic nervous system, and the seasonal influence on BP is the highest in the winter.15)18)25)
However, the relevant physiological mechanisms involved in the above-mentioned phenomenon remain unknown. The most physiologically significant alteration associated with low temperatures is an increase in BP. As the temperature decreases, BP increases and becomes more labile. This effect is particularly true in unacclimatized humans who are transitioning from normal temperatures to very cold or freezing temperatures. Therefore, lower temperatures are associated with increases in the risk of coronary artery disease and ICH.5)8)16)
Other potential etiological factors that could increase the risk of sICH include abrupt changes in physical activities and health-associated behaviors such as smoking, heavy alcohol consumption, and the physiologic response to exercise.9)14)17)20)
The present study has several limitations. First, being a retrospective study, it has potential analytic limitations for some clinical variables and characteristics such as risk factors for sICH, including previous/present medication and/or comorbidities (such as antiplatelet administration, amyloid angiopathy, prior cerebral infarction and hypercholesterolemia) that might directly affect the occurrence and precise onset time of sICH. Second, Incheon metropolitan city has a very long coastline and many islands, and the climate parameters used in our study were recorded at the Incheon weather station, not on the site where the sICH occurred. This might influence the association between the occurrence of sICH and meteorological parameters. Third, although patients were enrolled from the only level I regional emergency center within the territory of Incheon metropolitan city, because this is a single hospital-based, and not a population-based study, the true local incidence of sICH and its association with the local meteorological parameters are still unknown.
In our study, the number of admissions due to primary sICH did not vary significantly seasonally or in association with the local meteorological parameters. However, the daily temperature range tended to affect the number of admissions due to sICH. Although our results were not statistically significant, prospective multi-institutional or global studies that include hospitals located in regions with varying latitudes and seasonality should be conducted to investigate the association between sICH incidence and meteorological parameters such as daily temperature range.
References
1. Ali Y, Rahme R, Matar N, Ibrahim I, Menassa-Moussa L, Maarrawi J, et al. Impact of the lunar cycle on the incidence of intracranial aneurysm rupture: Myth or reality? Clin Neurol Neurosurg. 2008; 5. 110(5):462–465. PMID: 18353534.

2. Anderson CS, Chakera TM, Stewart-Wynne EG, Jamrozik KD. Spectrum of primary intracerebral haemorrhage in Perth, Western Australia, 1989-90: Incidence and outcome. J Neurol Neurosurg Psychiatry. 1994; 8. 57(8):936–940. PMID: 8057117.

3. Broderick JP, Brott T, Tomsick T, Miller R, Huster G. Intracerebral hemorrhage is more than twice as common as subarachnoid hemorrhage. J Neurosurg. 1993; 2. 78(2):188–191. PMID: 8421201.
4. Capon A, Demeurisse G, Zheng L. Seasonal variation of cerebral hemorrhage in 236 consecutive cases in Brussels. Stroke. 1992; 1. 23(1):24–27. PMID: 1731416.

5. Chambers JB, Williams TD, Nakamura A, Henderson RP, Overton JM, Rashotte ME. Cardiovascular and metabolic responses of hypertensive and normotensive rats to one week of cold exposure. Am J Physiol Regul Integr Comp Physiol. 2000; 10. 279(4):R1486–R1494. PMID: 11004019.

6. Cowperthwaite MC, Burnett MG. The association between weather and spontaneous subarachnoid hemorrhage: An analysis of 155 US hospitals. Neurosurgery. 2011; 1. 68(1):132–138. discussion 138-9. PMID: 21099710.

7. Feldmann E, Broderick JP, Kernan WN, Viscoli CM, Brass LM, Brott T, et al. Major risk factors for intracerebral hemorrhage in the young are modifiable. Stroke. 2005; 9. 36(9):1881–1885. PMID: 16081867.

8. Giaconi S, Ghione S, Palombo C, Genovesi-Ebert A, Marabotti C, Fommei E, et al. Seasonal influences on blood pressure in high normal to mild hypertensive range. Hypertension. 1989; 7. 14(1):22–27. PMID: 2737734.

9. Gill RS, Hambridge HL, Schneider EB, Hanff T, Tamargo RJ, Nyquist P. Falling temperature and colder weather are associated with an increased risk of aneurysmal subarachnoid hemorrhage. World Neurosurg. 2013; 1. 79(1):136–142. PMID: 22732514.

10. Haberman S, Capildeo R, Rose FC. The seasonal variation in mortality from cerebrovascualr disease. J Neurol Sci. 1981; 10. 52(1):25–36. PMID: 7299414.
11. Hughes MA, Grover PJ, Butler CR, Elwell VA, Mendoza ND. A 5-year retrospective study assessing the association between seasonal and meteorological change and incidence of aneurysmal subarachnoid haemorrhage. Br J Neurosurg. 2010; 8. 24(4):396–400. PMID: 20726749.

12. Inagawa T. Diurnal and seasonal variations in the onset of primary intracerebral hemorrhage in individuals living in Izumo City, Japan. J Neurosurg. 2003; 2. 98(2):326–336. PMID: 12593619.

13. Inagawa T, Takechi A, Yahara K, Saito J, Moritake K, Kobayashi S, et al. Primary intracerebral and aneurysmal subarachnoid hemorrhage in Izumo City, Japan. Part I: Incidence and seasonal and diurnal variations. J Neurosurg. 2000; 12. 93(6):958–966. PMID: 11117868.
14. Jabbour P, Tjoumakaris S, Dumont A, Gonzalez LF, Rosenwasser R. Aneurysm rupture: Lunar cycle, weather, atmospheric pressure, myth or reality? World Neurosurg. 2011; Jul-Aug. 76(1-2):7–8. PMID: 21839928.

15. Keatinge WR, Coleshaw SR, Cotter F, Mattock M, Murphy M, Chelliah R. Increases in platelet and red cell counts, blood viscosity, and arterial pressure during mild surface cooling: Factors in mortality from coronary and cerebral thrombosis in winter. Br Med J (Clin Res Ed). 1984; 11. 289(6456):1405–1408.

16. Kleinpeter G, Schatzer R, Bock F. Is blood pressure really a trigger for the circadian rhythm of subarachnoid hemorrhage? Stroke. 1995; 10. 26(10):1805–1810. PMID: 7570729.
17. Macdonald RL. Whether subarachnoid hemorrhage depends on the weather? World Neurosurg. 2013; 1. 79(1):64–65. PMID: 23103265.

18. Minami J, Kawano Y, Ishimitsu T, Yoshimi H, Takishita S. Seasonal variations in office, home and 24 h ambulatory blood pressure in patients with essential hypertension. J Hypertens. 1996; 12. 14(12):1421–1425. PMID: 8986924.

19. Shin MH, Park HK, Joo WI, Lee KJ, Rha HK. [Diurnal and Seasonal Variations in the Onset of Spontaneous Intracerebral Hemorrhage]. Korean J Cerebrovasc Surg. 2007; 3. 9(1):46–51. Korean.
20. Rønning P, Langmoen IA. Aneurysm rupture-does the weather matter? World Neurosurg. 2013; 1. 79(1):62–63. PMID: 22858847.

21. Special report from the National Institute of Neurological Disorders and Stroke. Classification of cerebrovascular diseases III. Stroke. 1990; 4. 21(4):637–676. PMID: 2326846.
22. Sobel E, Zhang ZX, Alter M, Lai SM, Davanipour Z, Friday G, et al. Stroke in the Lehigh valley: Seasonal variation in incidence rates. Stroke. 1987; Jan-Feb. 18(1):38–42. PMID: 3810768.

23. Takebayashi S. Ultrastructural morphometry of hypertensive medial damage in lenticulostriate and other arteries. Stroke. 1985; May-Jun. 16(3):449–453. PMID: 4002259.

24. Wang K, Li H, Liu W, You C. Seasonal variation in spontaneous intracerebral hemorrhage frequency in Chengdu, China, is independent of conventional risk factors. J Clin Neurosci. 2013; 4. 20(4):565–569. PMID: 23317754.

25. Woodhouse PR, Khaw KT, Plummer M. Seasonal variation of blood pressure and its relationship to ambient temperature in an elderly population. J Hypertens. 1993; 11. 11(11):1267–1274. PMID: 8301109.

Fig. 1
The relationship between the seasons and the monthly number of admissions due to spontaneous intracerebral hemorrhage (sICH). The association between the number of admission due to spontaneous intracerebral hemorhage and season was not statistically significant (F = 1.089, p = 0.368) (F: F distribution, p : p value). Analytical method: one-way analysis of variance between groups (ANOVA). Spring includes March, April and May; summer includes June, July and August; autumn includes September, October and November; and winter includes December, January and February.
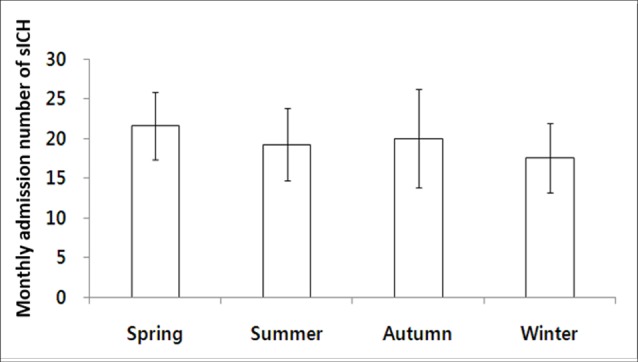
Fig. 2
Monthly number of admissions due to primary sICH and seasonality of each meteorological parameter during the study period. Top panel indicates rates of sICH admissions from 2008 to 2011. The lower 4 panels show the expected seasonality in the standardized weather readings from 2008 to 2011.

Fig. 3
The number of monthly admissions due to primary sICH plotted against each meteorological factor. Mean temperature (r = 0.009, p = 0.959); mean humidity (r = -0.068, p = 0.695); mean atmospheric pressure (r = -0.017, p = 0.923); mean daily temperature range (r = 0.281, p = 0.097). sICH= spontaneous ICH.
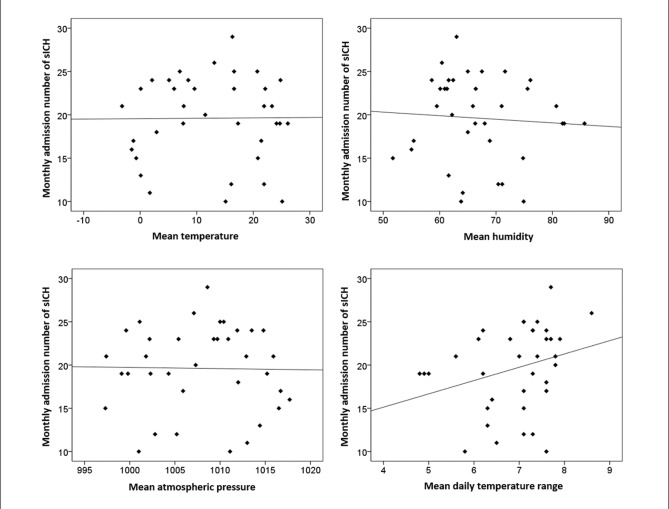
Table 1
Demographic and clinical characteristics of the 708 patients
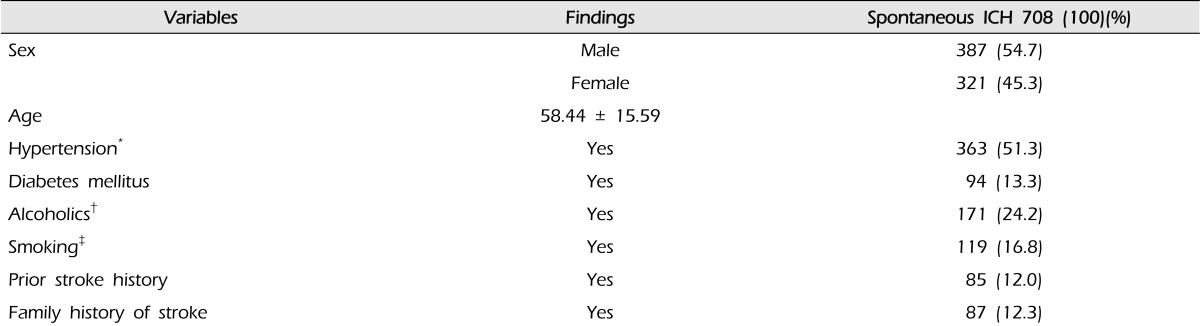
*Patients with history of antihypertensive medication or systolic/diastolic blood pressure over 140/90 mmHg and those with hypertension controlled with antihypertensive at the time of admission were not included; †Alcohol consumption more than twice per week; ‡Current or former smoker. ICH= intracerebral hemorrhage.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download