Abstract
Infraoptic anterior cerebral artery (ACA) is an extremely rare congenital anomaly. This anomalous artery usually arises from the intradural internal carotid artery (ICA) near the level of the ophthalmic artery (OA) or rarely from the extradural ICA. This anomaly frequently harbors a cerebral aneurysm, and may involve other coexisting vascular anomalies. In the case of this anomaly, surgical treatment of the aneurysm at the proximal ACA or anterior communicating artery (ACoA) may sometimes be difficult, because the veiled proximal ACA by the optic nerve would make proximal control inconvenient and the vertical midline segment of the proximal ACA would frequently form a superiorly directing aneurysm with a relatively high position. We report on an extremely rare case of a ruptured aneurysm at the infraoptic azygous ACA, possibly having an extradural origin, accompanied by contralateral ICA agenesis, and also introduce a feasible method for treatment by Y-stent assisted coil embolization.
The first segment (A1) of the anterior cerebral artery (ACA) normally branches off from the terminal of the internal carotid artery (ICA), runs above the optic nerve, and courses anteromedially to join the anterior communicating artery (ACoA). An infraoptic ACA is an exceedingly rare anomaly of the cerebral arterial system, which was first reported by Robinson in 1959.2)4)14)16) This anomalous artery usually arises from the intradural ICA near the level of the ophthalmic artery (OA) or rarely from the extradural ICA, courses medially and horizontally as it passes under the ipsilateral optic nerve, and makes a sharp turn superiorly to join the ACoA or distal branches.4)5) An azygous ACA is another anomaly, with a prevalence of 0.2% to 4%, which represents a single unpaired ACA featured as a solitary midline trunk that supplies both ACA territories; this anomalous artery is known to have an association with persistence of the embryonic median artery of the corpus callosum.13) Both infraoptic and azygous ACAs have been reported in association with an increased risk of aneurysm formation.
We report on an extremely rare case of a ruptured aneurysm at the infraoptic azygous ACA with the contralateral ICA agenesis, and introduce a feasible option for treatment of this aneurysm by Y-stent assisted coil embolization.
A 59-year-old female patient presented with a sudden bursting headache with a drowsy mentality. Brain computed tomography (CT) scan confirmed the presence of a diffuse subarachnoid hemorrhage (Fig. 1). Digital subtraction angiography revealed a ruptured bilobulated broad neck aneurysm at the terminal of the infraoptic azygous portion of the ACA where the bilateral distal ACAs branched off. This anomalous artery originated from the right ICA proximal to the OA, suggesting the possibility of an extradural ICA origin. The bilateral recurrent arteries of Heubner arose from the vertical portion of the azygous ACA in the midline, and coursed laterally to enter the anterior perforated substances. An aortogram showed the common origin of the brachiocephalic trunk and the left common carotid artery, known as the "bovine configuration", and the left carotid angiogram revealed agenesis of the left ICA, visualizing only the external carotid artery (ECA) systems. The territory of the left middle cerebral artery (MCA) was solely supplied via the prominent left posterior communicating artery (PCoA). The aneurysm was bilobulated with the largest diameter of 8.36 mm and had a broad neck of 5 mm slightly incorporating the bilateral branches of the distal ACA (Fig. 2).
Emergent endovascular coil embolization was performed under general anesthesia. A 6F Shuttle guiding sheath (Cook Medical, Bloomington, IN) was transfemorally advanced into the right cervical ICA. A Rebar 18 microcatheter (ev3 Inc, Irvine, CA) was inserted, covering from the azygous ACA to the proximal portion of the left distal ACA, preparing for use of a Solitaire AB (ev3 Inc, Plymouth, MN) afterward. An Excelsior SL-10 microcatheter (Boston Scientific, Natick, MA) was used for delivery of coils into the aneurysm. When the flow into the bilateral branches of the distal ACA began to be compromised during coil packing, a Solitaire AB was deployed into the previously installed Rebar microcatheter and another Solitaire AB was delivered into the right distal ACA in Y-configuration in order to preserve the bilateral distal ACA. The aneurysm was treated successfully without remnant (Fig. 3). The patient later suffered severe vasospasm but recovered fully without neurological deficit after undergoing intraarterial nimodipine angioplasty (Fig. 4). Follow-up brain CT and coronal reconstructions of magnetic resonance (MR) angiography source images provided clarification of the anatomical configuration of the azygous ACA with an infraoptic course in association with the optic nerve (Fig. 5).
An infraoptic course of the ACA is an extremely rare vascular anomaly. Since the first reported case in 1959, approximately 50 cases of this anomaly have been reported during autopsy, surgery, or angiography.4)14)16)17) An infraoptic ACA originating from the extradural ICA was reported in only four of these previous cases.1)4)6)8) Various terminologies, including infraoptic ACA and carotid-ACA anastomosis, have been used.12)14) This ACA anomaly is characterized by three features: an anomalous artery branches off from the ICA at the level of the OA, it courses beneath the optic nerve, and supplies the territory of the normal ACA.9)12)17) Our patient also presented with these features, and, in addition, showed an unusual anomaly of the contralateral ICA agenesis with the prominent PCoA solely providing collateral flow to the MCA territory; these findings appeared to show a close association with formation of the azygous ACA with the solitary midline trunk from where the bilateral branches of the distal ACA and the bilateral recurrent arteries of Heubner originated. The origin of this anomalous artery was proximal to the OA, possibly having an extradural location. The OA is the conventional anatomical landmark on angiography for differentiation between the intradural and extradural space; it typically originates from the dorsal ICA immediately adjacent to the dura. However, because the origin of the OA varies to some degree and the OA cannot always be visualized on an angiogram, this landmark is not always reliable.1) In the present case, the origin of the OA was clarified on the lateral view of the right carotid angiogram, and the origin of this anomalous artery appeared to be cavernous or clinoid ICA below the distal dural ring where the ICA penetrates into the intradural space.
The proposed embryogenesis of this anomaly is still controversial. There are three proposed theories: persistence of embryonic anastomosis between the primitive maxillary artery and the primitive olfactory artery, which later gives rise to the ACA, persistence of in utero communication between the primitive dorsal and ventral ophthalmic arteries, and persistence and enlargement of prechiasmatic anastomosis between the prechiasmal branch of the OA and chiasmal branches of the ACA.7)10)14)16)17)
The infraoptic ACA may be associated with other coexisting vascular anomalies, such as variants of carotid-basilar anastomosis, agenesis of the contralateral ICA, anomalous origin of the OA from the ECA, and fused pericallosal arteries.1)3)11)16) It can also accompany symptoms related to the optic nerve or optic chiasma compression.4)15)
The prevalence of intracranial aneurysms in association with infraoptic azygous ACA is high, probably due to local intrinsic structural and hemodynamic factors, and the most common site is the ACA-ACoA complex.3)6)7)8)11)12)15)16)17) However, according to previous reports, aneurysm formation may occur anywhere.1)4)
Diagnosis of this anomaly is important in planning for surgical treatment of the ACA aneurysm. Failure to notice the anomaly may result in unnecessary or inadequate dissection around the optic nerve, causing possible damage or excessive brain retraction in the effort to find the proximal ACA, causing an intraoperative aneurysm rupture. Therefore, a detailed preoperative inspection of cerebral angiography is necessary.
Surgical treatment of the aneurysm at the terminal portion of the infraoptic azygous ACA may sometimes be difficult, because the hidden proximal ACA behind the optic nerve would make proximal control inconvenient and the vertical midline segment of the proximal ACA would frequently cause development of a superiorly directing aneurysm with a relatively high position. Proximal control for aneurysm clipping may not be easy in an infraoptic location and the choice of surgical approaches between unilateral pterional versus bicoronal interhemispheric approaches, from its relatively high position in the midline, may be difficult; therefore, coil embolization can be an alternative treatment option. In the case of a broad neck aneurysm at the azygous ACA, preservation of bilateral distal branches of the ACA is essential in order to prevent further neurological deficits. Therefore, Y-stent assisted coil embolization, which is often used for treatment of a basilar top aneurysm, may be a feasible option, when endovascular treatment is considered as obliteration method for a large broad neck aneurysm at the terminal of the infraoptic azygous ACA.
The infraoptic azygous ACA is an extremely rare congenital anomaly related to interference in embryogenesis during the early stage of cranial artery development.4)16)17) The extradural origin of this anomaly is even more rare. It has a typical appearance on angiography: apparent low bifurcation of the ICA with the ACA arising near the OA, and a horizontal and medial course of the proximal ACA as it passes under the optic nerve before turning superiorly to join the bilateral branches of the ACA.4)5) It may accompany other vascular anomalies, such as variants of carotid-basilar anastomosis, or agenesis of the contralateral ICA, as in our case. Association of this anomaly with an intracranial aneurysm is frequent, and a detailed inspection of angiography is required when deciding on treatment modalities.
Figures and Tables
Fig. 1
Initial brain computed tomography (CT) scan reveals a diffuse and thick subarachnoid hemorrhage in the basal cisterns, the bilateral Sylvian fissures, and the anterior interhemispheric fissure.

Fig. 2
Anterior-posterior view (A) and lateral view (B) of the right internal carotid angiogram shows an aneurysm (black arrows) at the terminal of the infraoptic azygous portion of the anterior cerebral artery (ACA) (white arrows). This anomalous artery originates from the internal cerebral artery proximal to the ophthalmic artery (white arrowheads). The bilateral recurrent arteries of Heubner (black arrowheads) arise from the vertical portion of the azygous ACA in the midline, and course laterally into the anterior perforated substances. Left carotid angiogram (C) shows agenesis of the ICA. The left middle cerebral artery is visualized on the vertebral angiogram (D) via the prominent posterior communicating artery. Working projection view (E) shows a bilobulated aneurysm with a broad neck slightly incorporating the bilateral distal ACA branches.

Fig. 3
Angiogram after coil embolization shows complete occlusion of the aneurysm. Proximal and distal markers (black arrowheads) indicate partially overlapping double stents in Y-configuration protecting the distal ACA branches.

Fig. 4
Vasospasm (black arrowheads) is prominent at the ACA branches distal to the stents on the follow-up angiogram.
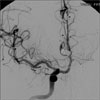
Fig. 5
Anatomical locations of the infraoptic azygous ACA (white arrows) with stent, optic nerve (black arrows), optic canal (black arrowheads), anterior clinoid process (black asterisks), and ophthalmic artery (white arrowheads) are shown in axial (brain setting, A) and coronal views (bone setting, B) of follow-up brain CT, and serial coronal reconstructions (C) of MR angiography source images from anterior to posterior. Note that the stents are replaced by metal artifacts (white asterisks) on MR images.

References
1. Akiyama Y, Okada T, Hayashi N, Yokoi T. Infraoptic course of the anterior cerebral artery originating from the extradural internal carotid artery associated with contralateral internal carotid artery agenesis and multiple intracerebral aneurysms. Neurol Med Chir (Tokyo). 2010. 11. 50(11):984–987.
2. Al-Qahtani S, Tampieri D, Brassard R, Sirhan D, Mellanson D. Coil embolization of an aneurysm associated with an infraoptic anterior cerebral artery in a child. AJNR Am J Neuroradiol. 2003. 05. 24(5):990–991.
3. Fujimoto S, Murakami M. Anomalous branch of the internal carotid artery supplying circulation of the anterior cerebral artery: case report. J Neurosurg. 1983. 06. 58(6):941–946.
4. Given CA II, Morris PP. Recognition and importance of an infraoptic anterior cerebral artery: case report. AJNR Am J Neuroradiol. 2002. 03. 23(3):452–454.
5. Gupta V, Chugh M, Vaishya S. Infraoptic azygous anterior cerebral artery. Neurol India. 2008. Oct-Dec. 56(4):487–488.

6. Hillard VH, Musunuru K, Nwagwu C, Das K, Murali R, Zablow B, et al. Treatment of an anterior communicating artery aneurysm through an anomalous anastomosis from the cavernous internal carotid artery. J Neurosurg. 2002. 12. 97(6):1432–1435.

7. Isherwood I, Dutton J. Unusual anomaly of the anterior cerebral artery. Acta Radiol Diagn (Stockh). 1969. 9:345–351.
8. Kessler LA. Unusual anomaly of the anterior cerebral artery: report of a case. Arch Neurol. 1979. 08. 36(8):509–510.
9. Ladzinski P, Maliszewski M, Majchrzak H. The accessory anterior cerebral artery: case report and anatomic analysis of vascular anomaly. Surg Neurol. 1997. 08. 48(2):171–174.
10. McLaughlin N, Bojanowski MW. Infraoptic course of anterior cerebral arteries associated with abnormal gyral segmentation. Case report. J Neurosurg. 2007. 08. 107(2):430–434.
11. Nutik S, Dilenge D. Carotid-anterior cerebral artery anastomosis: Case report. J Neurosurg. 1976. 03. 44(3):378–382.
12. Odake G. Carotid-anterior cerebral artery anastomosis with aneurysm: case report and review of the literature. Neurosurgery. 1988. 11. 23(5):654–658.

13. Osborn AG. Diagnostic cerebral angiography. 1999. 2nd ed. Philadelphia: Lippincott Williams and Wilkins;125. 128.
14. Robinson LR. An unusual human anterior cerebral artery. J Anat. 1959. 01. 93(1):131–133.
15. Senter HJ, Miller DJ. Interoptic course of the anterior cerebral artery associated with anterior cerebral artery aneurysm. Case report. J Neurosurg. 1982. 02. 56(2):302–304.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download