Abstract
Organized hematoma is a pseudo-tumorous lesion mostly occurs at sinonasal cavity and often confused with malignant neoplasm. The initiation of this lesion is blood accumulation, probably due to trauma, and this hematoma develops into organized hematoma as it encapsulated with fibrous band and neo-vascularized. Since it is uninformed at temporomandibular joint (TMJ) region, imaging diagnosis might be challenging. Also, delayed detection of mass involving TMJ is not uncommon due to confusion with joint disorder. Thus, this report introduced the rare pathology, organized hematoma on TMJ with advanced imaging features. Also, diagnostic point for early detection was described for the TMJ tumors and pseudo-tumors considering complexity of surgical intervention in this region.
Organized hematoma is a rare pseudo-tumorous lesion mostly occurs in confined and vascularized region such as sinonasal cavity.12 Even though it is not a true tumor, it continually makes expansion and aggressively destructs adjacent structures, thus frequently misdiagnosed as malignant tumor. The pathogenesis of the lesion is not clearly elucidated, and it is suspected to occur when hematoma is not absorbed and became chronic under the condition of drainage absence.
While, various kinds of tumors and pseudo-tumors can be shown in temporomandibular joint (TMJ) region, including synovial chondromatosis, osteochondroma, pigmented villonodular synovitis, metastatic tumors and plasmacystoma, the organized hematoma is uninformed on this area. Additionally, the clinical detection of neoplasms involving TMJ is often delayed due to the similar manifestations of it to ordinary TMJ internal derangement.34 In fact, approximately 20% of patient, actually having mass on TMJ, initially diagnosed and treated as joint derangement. The mean delayed in time in diagnosis of tumor or tumor-like lesion of TMJ was 2.5 years. Thus, diagnosis of organized hematoma might be challenging for both clinician and radiologist.34
Therefore, this report introduced the useful imaging features of organized hematoma occurred on TMJ for precise diagnosis. Also, diagnostic point for early detection was described for the TMJ tumors and pseudo-tumors to avoid delayed diagnosis.
A 68-year-old male patient presented with a swelling and pain on the left pre-auricular region initiated about two to three years ago. He also had pain increases during opening his mouth. He had botulinum toxin injected on the affected area three month ago, and the symptom was not relieved at all. There was no particular underlined systemic disease in his medical record.
A TMJ panoramic radiography, an imaging technique especially for assessing TMJ structure, was performed to evaluate if there is degenerative change of condyle and articulating eminence as well as relative position of condyle to articular fossa. The image revealed that joint space was slightly widened on left TMJ compared with the right side (Fig. 1A). While, there was no restriction of both condyles during mouth opening (Fig. 1B). No significant destruction or remodeling of bony structure was seen on joint components.
A computed tomography (CT) and magnetic resonance (MR) imaging, both without contrast-media, were also obtained to evaluate any minor degenerative change of condyle and disc problem of TMJ. On the CT images, round soft tissue attenuation was localized on the posterolateral aspects of left condyle head (Fig. 2A). The lesion showed soft-tissue equivalent attenuation compared with the adjacent muscles. As it was shown in the TMJ panoramic radiography, there was no significant bony destruction; however, slight thinning and focal discontinuity of cortical bone was detected on the condyle head contacting with the lesion. Also, mild subchondral sclerosis was found on this site (Fig. 2B).
On MR image of proton density and T1-weighted sequence, the lesion was well-encapsulated and showed heterogeneous signal indicating solid mass rather than cyst (Fig. 3). The left mandibular condyle showed anterior dislocation due to a mass on the posterior aspect. However, TMJ discs were in normal position during the mouth open and close conditions. Local T1 hyper-intensity was recognized as it indicated that there was hematogenous component included in this lesion (Fig. 3C).
With preliminary diagnosis of organized hematoma or giant cell tumor based on the images, the ovoid mass located on the postero-lateral aspect of left condylar head was surgically removed (Fig. 4A). On the histopathologic exam, the lesion was composed of blood cells intermixed with granulation tissue. It was encapsulated with fibrous band and there was slight neovascularization was observed on the border of the capsule (Fig. 4B). With the above findings, organized hematoma has been made as final diagnosis. No significant complications were found during a month of follow-up period.
Histopathologically, this lesion is composed of multinucleated foreign-body-type giant cells, thick fibrotic capsule with neovascularization.2 Its pathogenesis is not clear, however, blood accumulation without proper drainage is suggested as the initial stage. The known cause of this initial stage is traumatic hemorrhage, while, the time interval between the trauma and the symptom occurrence may vary from a month to years.5 The hematoma usually dissolves in several days, however it is not absorbed and became chronic hematoma, it starts organizing with neovascularization.125
Even though very rare, there have been reports of organized hematoma on other body part including retroperitonium, thigh and lower leg rather than sinonasal cavity.678 In addition, there was one case with similar pathology, involving TMJ, and authors introduced this lesion as a hematic cyst.9 However, Bergin et al.10 stated that hematic cyst was basically describing the same pathologic entity as organized hematoma, thus, the current case was the second report of this unusual disease, as far as the author knows. Considering TMJ region is confined space with capsule and rich in vascular supply close to maxillary artery, the possibility of organized hematoma occurrence cannot be disregarded in this area.
Currently, MR imaging feature of organized hematoma involving sinonasal cavity has been well described. The heterogeneous internal signal indicating various stages of hemorrhage is characteristic in MR imaging.1 This feature was also useful for diagnosis of TMJ case. Both previous case9 and our case showed the heterogeneous signal including T1-hyperintesity, which could be correlated with hemosiderin component of the mass. Still, this feature might also be suitable for describing tumors showing internal hemorrhage signal such as vascular malformation or giant cell tumors.1112 Compared with vascular malformation and giant cell tumors, organized hematoma showed hypointense peripheral rim indicating fibrous capsule around the mass.9 In addition, giant cell tumors occurred in this region showed more aggressive expansion involving cranial base or condyle head destruction compared to the organized hematoma.12
Early diagnosis is challenging for TMJ tumors and pseudotumors. The patient in our case also had been diagnosed with joint disorder, initially and underwent botolinium toxin injection. Considering trauma is suspected as the etiology of organized hematoma, thus, the injection might also be a causative factor. Thus, clinician may give a careful diagnosis and close check-up after such process including the arthrocentesis on TMJ, which is one of a known treatment option for TMJ disorder. Also, for the TMJ showing intact bony contour of condyle and articular eminence while joint space increased in TMJ panoramic radiography, as it was shown in our case, the advanced imaging modality might be useful for differential diagnosis between the mass and the joint problems. In the internal derangement of TMJ, according to previous research, decreased joint space or retropositioned condyle was shown in the radiography.13
Organized hematoma in sinonasal cavity shows aggressive expansion of the mass occupying the whole cavity, which may not distinguishable from malignant tumor. For the TMJ lesion, both cases did not show aggressive feature. This might be due to the small size of the lesion. Even with the small size, the previous organized hematoma occurred in TMJ region caused deformity and erosion of lateral condyle head. In our case, very subtle but reactive subchondral sclerosis was appeared on the contact surface of the condyle. Overall, this lesion seemed to possess potential to show mass effect on bone structure, surgical removal would be the primary choice as stated in previous studies.129 Since the surgical intervention of TMJ region is complex and may accompany complications including nerve damage, infection and malocclusion, early diagnosis and removal would be important.14
In conclusion, organized hematoma of TMJ is rare but possibly occurring disease and MR imaging is helpful for diagnosis. This lesion may involve bony structure of this lesion, thus careful and early diagnosis is essential to prevent challenging surgical procedure and post-operative complications.
Figures and Tables
Fig. 1
A. Temporomandibular joint (TMJ) panoramic radiography taken during mouth closing. There is slight enlarged space between the articular fossa and condyle on the left side. B. TMJ panoramic radiography taken during mouth opening. Both sides of condyle show no limitation during mouth opening.

Fig. 2
Non-contrast Computed tomography (CT) images. A. Soft tissue window of CT images reveal round mass on the postero-lateral aspect of the condyle (arrow head). B. Cropped CT image in bone-tissue window shows slight subchondral sclerosis (hollow arrow head) and erosive change of cortex (arrow) on the left condyle compared to the right side.
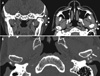
Fig. 3
A. Proton density of magnetic resonance image during mouth opening shows heterogeneous internal signal with thick and dark encapsulation. B. The condyle is not reduced to its normal position during mouth closing. C. T1-weighted image shows hyperintense signal within the lesion, which indicate hemorrhagic contents.

References
1. Hur J, Kim JK, Byun JS, Lee WJ. Imaging characteristics of sinonasal organized hematoma. Acta Radiol. 2015; 56:955–959.

2. Ohta N, Watanabe T, Ito T, Kubota T, Suzuki Y, Ishida A, et al. Clinical and pathological characteristics of organized hematoma. Int J Otolaryngol. 2013; 2013:539642.

3. Yanagi Y, Asaumi J, Maki Y, Murakami J, Hisatomi M, Matsuzaki H, et al. Incidentally found and unexpected tumors discovered by MRI examination for temporomandibular joint arthrosis. Eur J Radiol. 2003; 47:6–9.

4. Poveda-Roda R, Bagán JV, Sanchis JM, Margaix M. Pseudotumors and tumors of the temporomandibular joint. A review. Med Oral Patol Oral Cir Bucal. 2013; 18:e392–e402.

5. Som PM, Curtin HD. Head and neck imaging. 5th ed. St. Louis: Mosby;2011.
6. Negoro K, Uchida K, Yayama T, Kokubo Y, Baba H. Chronic expanding hematoma of the thigh. Joint Bone Spine. 2012; 79:192–194.

7. Wollina U, Heinig B, Langner D. Chronic expanding organized hematoma of the lower leg: a rare cause for nonhealing leg ulcers. Int J Low Extrem Wounds. 2015; 14:295–298.
8. Ivankiv T, Ogurtsov O, Pokhylevych G. Organized hematoma mimicking retroperitoneal cystic tumors. Int J Surg Case Rep. 2016; 19:147–149.

9. Orhan K, Nishiyama H, Mitsunobu K, Furukawa S, Delilbasi C. Chronic hematic cyst of the temporomandibular joint: MRI features and dynamic magnetic resonance imaging. Eur J Radiol Extra. 2004; 52:97–101.

10. Bergin DJ, McCord CD, Dutton JJ, Garrett SN. Chronic hematic cyst of the orbit. Ophthal Plast Reconstr Surg. 1988; 4:31–36.

11. Zhou Q, Yang C, Chen MJ, Qiu YT, Qiu WL, Zheng JW. Primary intra- and juxta-articular vascular malformations of the temporomandibular joint: a clinical analysis of 8 consecutive patients. Int J Clin Exp Med. 2015; 8:2247–2253.
12. Hu Y, Kuang B, Chen Y, Shu J. Imaging features for diffuse-type tenosynovial giant cell tumor of the temporomandibular joint: a case report. Medicine (Baltimore). 2017; 96:e7383.
13. Ren YF, Isberg A, Westesson PL. Condyle position in the temporomandibular joint. Comparison between asymptomatic volunteers with normal disk position and patients with disk displacement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995; 80:101–107.
14. Holmlund AB. Surgery for TMJ internal derangement. Evaluation of treatment outcome and criteria for success. Int J Oral Maxillofac Surg. 1993; 22:75–77.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download