Abstract
Historically, Eagle syndrome is a term that has been used to describe radiating pain in the orofacial region, foreign body sensation, and/or dysphagia due to a unilateral or bilateral elongated styloid process impinging upon the tonsillar region. Because elongated styloid processes–with or without associated Eagle syndrome–can present with various symptoms and radiographic findings, it can be challenging for healthcare practitioners to formulate an accurate diagnosis. Abnormal styloid anatomy can lead to a multitude of symptoms, including chronic orofacial/neck pain, thus masquerading as more commonly diagnosed conditions. In this report, we describe a patient who presented to our department with styloid process elongation and fracture. A careful history, physical examination, and a conebeam computed tomography (CBCT) investigation led to the diagnosis. The patient was then referred for appropriate care. This case report demonstrates the utilization of CBCT in differentiating a fracture site from a pseudo-joint that might mimic a fracture.
The styloid process is a bony prominence of the petrous portion of the temporal bone that projects anteriorly, inferiorly, and slightly medially.1234 The normal length of the styloid process is approximately 20 mm, although it can vary on an individual basis.567 When a styloid process exceeds 30 mm in length, it is considered to be elongated.13458910 Approximately 4% of the population has an elongated styloid process,16 and the majority of these patients are diagnosed based on an incidental radiographic finding.8
Among patients with elongated styloid processes, 4%–10% are estimated to have a symptomatic elongated styloid process, known as Eagle syndrome.1358 The most common symptoms include throat pain, dysphagia, foreign body sensation, facial pain, tinnitus, otalgia, and limitation of mandibular movements.361011121314 However, the broad range of symptoms presents a diagnostic challenge.3 Eagle syndrome is characterized by facial pain arising from the compression of adjacent anatomical structures due to an elongated styloid process or a calcified stylohyoid ligament.813 Eagle syndrome has a 3:1 female-to-male predilection, and affected patients most commonly present with an elongated styloid process between the ages of 30 and 50.115 The presence of symptoms is essential for Eagle syndrome to be diagnosed, and clearly marks the distinction from a patient with an asymptomatic elongated styloid process.3816 Simply identifying a calcified stylohyoid ligament or an elongated styloid process radiographically does not warrant the diagnosis of Eagle syndrome.3 Although uncommon, the timely and proper diagnosis of Eagle syndrome is imperative in all medical fields.1517 To confirm the physical examination findings, a panoramic radiograph can be used to identify the elongated styloid process. However, because panoramic imaging does not always reliably capture the area of the styloid process, cone-beam computed tomography (CBCT) may be utilized to visualize the styloid anatomy.2691618 Pain management is critical for some patients who have both Eagle syndrome and other associated findings; therefore, the proper diagnosis is important. In some cases, the comorbid factors may lead to facial or neck pain, rather than Eagle syndrome itself.
It is important to recognize that other conditions, such as a fractured styloid process, may present similarly to Eagle syndrome. The signs and symptoms of an elongated styloid process or a stylohyoid ligament calcification as originally described by Eagle are very similar to the clinical presentation of a fractured styloid process.101112 The differential diagnosis for a patient presenting with a fractured styloid process may include temporomandibular joint dysfunction, tonsillitis, pharyngitis, mastoiditis, pain secondary to unerupted or impacted third molars, glossopharyngeal neuralgia, sphenopalatine neuralgia, trigeminal neuralgia, pharyngeal foreign body or tumor, migraine, degenerative disc disease, chronic laryngopharyngeal reflux, cluster headache, or myofascial pain dysfunction syndrome.15192021
This report presents a 46-year-old patient with cervical pain due to a fractured styloid process, which was originally suspected to be a parotid pathology. Evaluating the patient both clinically and radiographically aided in diagnosing the correct source of pain.
A 46-year-old African-American male presented to the admissions clinic at Penn Dental Medicine with the chief complaint of needing a check-up due to left neck tenderness. The patient's medical history revealed that he had been involved in a brawl 4 months previously, which resulted in an injury in the left infraorbital and malar regions. The patient went to the emergency room, where he received a consultation from an otorhinolaryngologist and a primary care physician. The medical team diagnosed the patient with left orbital fracture, which was reduced and surgically treated with bone plating and screws.
Following surgery, the patient complained of unilateral left-sided jaw and neck pain along with mild swelling for a duration of 3 weeks. The patient reported constant, dull, pressure-like pain that transformed to sharp pain on percussion. The pain was elicited by chewing, swallowing, and lateral neck movements. These sharp pain episodes lasted for a few minutes, and the patient reported that cracking his neck relieved the pain. The patient experienced swelling and tenderness in his left cervical area, which was also associated with similar pain episodes occurring for the past few months. Due to this pain, the patient revisited the otorhinolaryngologist at the local hospital. He was sent for magnetic resonance imaging (MRI) of the cervical spine. MRI showed intact vertebrae with mild degenerative changes, as well as mild canal stenosis. In addition, a parotid salivary gland biopsy and submandibular fine needle aspiration were performed on the left submandibular salivary gland tissue. These procedures were done because it was thought that the pain originated from the salivary glands, specifically the left parotid, as the pain was radiating to that region. The biopsy results revealed normal glandular tissue and no evidence of malignancy. Aspiration of the swelling only managed to provide short-term symptom relief for a period of 2 weeks.
When the patient presented to Penn Dental Medicine for a re-evaluation, he reported a long history of xerostomia, pain with deglutition, and dysphagia. He denied dysgeusia. His further medical history included hypertension, hepatitis C, HIV infection, and epileptic seizures, all of which were medically managed. He reported that although his most recent seizure was after the altercation, his last unprovoked seizure was in 2007.
A repeated clinical exam showed mild diffuse swelling with tenderness on the left posterior auricular area, tenderness on the left side of the submandibular and parotid area, and pinpoint tenderness near the gonial angle at the level of the C3/C4 vertebrae. No tenderness or salivary gland enlargement was noted on bimanual manipulation of the right submandibular and parotid glands. The range of motion for jaw opening was within normal limits and without myofascial pain on the right side. The temporomandibular joint exam was bilaterally within normal limits. However, due to multifocal tenderness and diffuse swelling, it was difficult to appreciate definitive objective findings on the left side. Cranial nerves II-XII were intact. Intraoral examination showed dental caries on tooth #15 with sensitivity to percussion, mild oral dryness, and clear saliva that was scant when milked from the parotid and submandibular ducts.
A panoramic radiograph was obtained to rule out any odontogenic pathology and to visualize the immediate vicinity of the submandibular region. The radiograph showed bilaterally elongated styloid processes and what appeared to be a horizontal lucency right through the left styloid process at the level of C3 and C4. CBCT was then performed to evaluate the extent of the mineralization and to review the suspected fracture 3-dimensionally. The CBCT images (Figs. 1,2,3,4,5) revealed multiple pseudo-jointed bilateral elongated styloid processes, a well-mineralized stylohyoid process with an almost uniform thickness of 11mm, and a confirmed fracture on the left side at the level of C3/C4. Based on the radiographic findings and the patient's symptoms, he was eventually diagnosed with a left fractured styloid process as the source of his neck pain. The fracture site was clearly evident on all multiplanar reconstructions (included here are axial, sagittal, and coronal slices) and was clearly different from the pseudo-joint formations and pseudo-articulations. Although pseudo-joints have a central radiolucency, they are covered by ossifications all around, demonstrating the presence of a joint. Fractured bone can be easily identified radiographically, as the area is devoid of any pseudo-joint formations (Fig. 6). The patient was then referred to the Department of Oral and Maxillofacial Surgery at the Hospital of the University of Pennsylvania for left styloidectomy.
The CBCT scan revealed elongated styloid processes, pseudo-arthroses of the stylohyoid ligaments, and a left fractured styloid process. A clear definition of the stylohyoid complex can be seen using the coronal view, while the axial view allows for thorough identification of the stylohyoid chain location and its anatomical relationships.22 Although the stylohyoid calcification on the panoramic radiograph was an incidental finding, it is likely that the patient's fractured elongated styloid process was the primary cause of the symptoms he presented with. Other factors, such as myofascial discomfort and sialadenitis secondary to his underlying oral dryness, could not be ruled out at that time. Given his symptoms upon presentation and his imaging results, the cervical pain was attributed to his elongated styloid process, and the patient was subsequently diagnosed with a fractured styloid process inducing prolonged cervical pain. A detailed medical history, thorough clinical examination by palpation of the tonsillar fossa and retromandibular region, and radiographic examination using CBCT are essential in making a definitive diagnosis of a fractured styloid process.1619
Styloid process fracture is considered to be a rare traumatic condition, and it is poorly understood in the literature.1923 Characterizing and diagnosing the source of orofacial pain is becoming extremely difficult for dentists, oral maxillofacial surgeons, and otorhinolaryngologists.23 While our case report describes a patient with a fractured styloid process presenting with neck pain, Kermani et al. reported a patient who also had a fractured styloid process, but presented with temporomandibular joint disorder.23 Gayathri et al.24 discussed a more complicated case in which a patient was diagnosed with a styloid fracture co-existing with a mandibular fracture. It is evident that the symptoms associated with a styloid fracture are easy to misdiagnose, making a careful examination a critical aspect of deciphering the source of pain.
Dental outpatient settings are not the only healthcare site where a fractured styloid process can be diagnosed and treated.17 Due to the varying, non-specific, symptomatic presentations of a fractured styloid process, it is not uncommon for patients with this condition to present to a wide range of healthcare professionals, such as primary care physicians, otorhinolaryngologists, neurologists, neurosurgeons, and psychiatrists.17 Having a thorough understanding of the treatment modalities for styloid process fracture and guiding the patient in the appropriate direction to help manage their condition are critical steps. The management of styloid process fracture can include conservative therapy, medical management, or surgical treatment.2526 A conservative approach typically includes heat, rest, liquid diet, non-steroidal anti-inflammatory agents, and muscle relaxants.2527 Medical management consists of steroidal injections, administration of long-acting local anesthetics in the tonsillar fossa region, and oral administration of carbamazepine.1225 Surgical management can be done through either the intraoral or extraoral approach.2562829 If the symptoms can be relieved with conservative treatment, that is the preferred route;25 however, surgery was prudent for the patient in our case due to his presenting and ongoing symptoms. The patient was initially prescribed analgesics for pain management, but the relief was only temporary, so he was referred for surgical intervention due to the limitations of the conservative regimen. Intraoral surgical management of this condition is via an incision on the periosteum at the tip of the styloid process, followed by an appropriate excision of the bony projection.628 For the extraoral method, the incision is more extensive and starts from the mastoid process, extends to the hyoid bone, and then extends to the midline of the chin.2172930 The advantages of the intraoral technique are that it is safe, simple, less time-consuming, and leaves no scar. However, deep neck infection, injury to the major vessels, and poor visualization are its drawbacks.62830 In contrast, the external approach provides adequate visualization and reduces the risk of a deep cervical infection. Scarring, the length of the procedure, and the relatively high likelihood of injuring the facial nerve are disadvantages of the extraoral surgical procedure.282931
It is inherently difficult to properly diagnose a fractured styloid process due to conflicting factors and the obscure clinical presentation. While an elongated styloid process is a condition that can be easily diagnosed, it is still important to include styloid process fracture within the differential diagnosis for applicable cases to provide patients with the appropriate treatment. Due to similarities in the clinical presentation, a clinician can easily mistake a fractured styloid process for a number of other commonly identified conditions, such as facial neuralgias and craniofacial diseases associated with dental, oral, or temporomandibular joint regions.3132 By reviewing this case study, all healthcare practitioners have been alerted of the appropriate strategies for managing patients with symptoms associated with a fractured styloid process or an elongated styloid process, as well as how to differentiate these possibilities from other conditions that can present similarly. Styloidectomy is the treatment of choice for a fractured styloid process.
Eagle syndrome-like symptoms, when masquerading as chronic neck pain, are challenging for clinicians to diagnose. The patient described herein was initially suspected to have having a salivary gland pathosis; therefore, MRI and a parotid gland biopsy were obtained unnecessarily. A proper history, physical examination, and utilization of CBCT led to the correct diagnosis in our case.
Figures and Tables
Fig. 1
A panoramic reconstruction cone-beam computed tomography image of the patient shows the elongated styloid processes bilaterally and the fractured left styloid process (arrow).
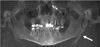
Fig. 2
A sagittal cone-beam computed tomography image of the skull shows only the left styloid process (arrows).
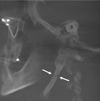
Fig. 3
A coronal cone-beam computed tomography image shows the styloid processes bilaterally and identifies the fractured left styloid process (arrows).
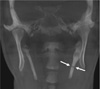
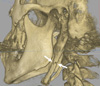
Fig. 4
An axial cone-beam computed tomography image shows the styloid processes bilaterally and identifies the fractured left styloid process (arrows).

References
2. Naik SM, Naik SS. Tonsillo-styloidectomy for Eagle's syndrome: a review of 15 cases in KVG Medical College Sullia. Oman Med J. 2011; 26:122–126.
3. Mupparapu M, Robinson MD. The mineralized and elongated styloid process: a review of current diagnostic criteria and evaluation strategies. Gen Dent. 2005; 53:54–59.
4. Feldman VB. Eagle's syndrome: a case of symptomatic calcification of the stylohyoid ligaments. J Can Chiropr Assoc. 2003; 47:21–27.
5. Han MK, Kim DW, Yang JY. Non surgical treatment of Eagle's syndrome - a case report -. Korean J Pain. 2013; 26:169–172.

6. Politi M, Toro C, Tenani G. A rare cause for cervical pain: Eagle's syndrome. Int J Dent. 2009; 2009:781297.

7. Chandler JR. Anatomical variations of the stylohyoid complex and clinical significance. Laryngoscope. 1977; 87:1692–1701.
8. Murtagh RD, Caracciolo JT, Fernandez G. CT findings associated with Eagle syndrome. AJNR Am J Neuroradiol. 2001; 22:1401–1402.
9. Gokce C, Sisman Y, Sipahioglu M. Styloid process elongation or Eagle's syndrome: is there any role for ectopic calcification? Eur J Dent. 2008; 2:224–228.

10. Eagle WW. Symptomatic elongated styloid process: report of two cases of styloid process-carotid artery syndrome with operation. Arch Otolaryngol. 1949; 49:490–503.

11. Eagle WW. Elongated styloid process: report of two cases. Arch Otolaryngol. 1937; 25:584–587.
12. Eagle WW. Elongated styloid process; symptoms and treatment. AMA Arch Otolaryngol. 1958; 67:172–176.

13. Balbuena L Jr, Hayes D, Ramirez SG, Johnson R. Eagle's syndrome (elongated styloid process). South Med J. 1997; 90:331–334.

14. Langlais RP, Miles DA, Van Dis ML. Elongated and mineralized stylohyoid ligament complex: a proposed classification and report of a case of Eagle's syndrome. Oral Surg Oral Med Oral Pathol. 1986; 61:527–532.

15. Mendelsohn AH, Berke GS, Chhetri DK. Heterogeneity in the clinical presentation of Eagle's syndrome. Otolaryngol Head Neck Surg. 2006; 134:389–393.

16. Balasubramanian S. The ossification of styloid ligament and its relation to facial pain. Br Dent J. 1964; 116:108–111.
17. Khandelwal S, Hada YS, Harsh A. Eagle's syndrome - a case report and review of the literature. Saudi Dent J. 2011; 23:211–215.

18. Keur JJ, Campbell JP, McCarthy JF, Ralph WJ. The clinical significance of the elongated styloid process. Oral Surg Oral Med Oral Pathol. 1986; 61:399–404.

19. Tiwary P, Sahoo N, Thakral A, Ranjan U. Styloid process fracture associated with maxillofacial trauma: incidence, distribution, and management. J Oral Maxillofac Surg. 2017; 75:2177–2182.

20. Pinheiro TG, Soares VY, Ferreira DB, Raymundo IT, Nascimento LA, Oliveira CA. Eagle's syndrome. Int Arch Otorhinolaryngol. 2013; 17:347–350.

21. Gossman JR Jr, Tarsitano JJ. The styloid-stylohyoid syndrome. J Oral Surg. 1977; 35:555–560.
22. Alcalde RE, Ueyama Y, Nishiyama A, Mizuguchi T, Matsumura T, Kishi K. Diagnostic imaging of Eagle's syndrome: report of three cases. Oral Radiol. 1994; 10:63–68.

23. Kermani H, Dehghani N, Aghdashi F, Esmaeelinejad M. Nonsyndromic isolated temporal bone styloid process fracture. Trauma Mon. 2016; 21:e24395.

24. Gayathri G, Elavenil P, Sasikala B, Pathumai M, Krishnakumar Raja VB. ‘Stylo-mandibular complex’ fracture from a maxillofacial surgeon's perspective-review of the literature and proposal of a management algorithm. Int J Oral Maxillofac Surg. 2016; 45:297–303.
25. Dubey KN, Bajaj A, Kumar I. Fracture of the styloid process associated with the mandible fracture. Contemp Clin Dent. 2013; 4:116–118.

26. Blythe JN, Matthews NS, Connor S. Eagle's syndrome after fracture of the elongated styloid process. Br J Oral Maxillofac Surg. 2009; 47:233–235.

27. Smith GR, Cherry JE. Traumatic Eagle's syndrome: report of a case and review of the literature. J Oral Maxillofac Surg. 1988; 46:606–609.

28. Chase DC, Zarmen A, Bigelow WC, McCoy JM. Eagle's syndrome: a comparison of intraoral versus extraoral surgical approaches. Oral Surg Oral Med Oral Pathol. 1986; 62:625–629.

29. Chrcanovic BR, Custódio AL, de Oliveira DR. An intraoral surgical approach to the styloid process in Eagle's syndrome. Oral Maxillofac Surg. 2009; 13:145–151.

30. Strauss M, Zohar Y, Laurian N. Elongated styloid process syndrome: intraoral versus external approach for styloid surgery. Laryngoscope. 1985; 95:976–979.
31. Baseer MA, Alenazy MS. Eagle's syndrome: a rare case of young female. Dent Res J (Isfahan). 2013; 10:568–570.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download