Abstract
Purpose
The nasopalatine canal is a well-known, important anatomical structure in the anterior maxilla, but this region contains many accessory canals. The canalis sinuosus (CS) is one of these canals; it contains the anterior superior alveolar nerve, along with veins and arteries. The purpose of this study was to evaluate the CS using conebeam computed tomography (CBCT) in patients with maxillary impacted canines.
Materials and Methods
A total of 111 patients admitted to the Istanbul Medipol University School of Dentistry for the exposure, orthodontic treatment, and/or extraction of an impacted canine were included in this study. CBCT images were obtained for these patients under standard conditions. Axial, coronal, and sagittal sections were evaluated to assess the prevalence of CS, the direction and diameter of the canal, its relation with the impacted canine, and its distance from the alveolar crest. Further, possible correlations with patient gender and age were analyzed.
Results
The CS could be detected bilaterally in all the evaluated tomography images. The mean canal diameter was significantly larger in males than in females (P=.001). The CS ran significantly closer to the impacted canine when the canal was located horizontally (P=.03). Variations of the canal, such as accessory canals, were identified in 6 patients.
It is important for surgeons to pay close attention to the presence of neurovascular structures during operations. The anterior maxilla, also called the premaxilla, is usually considered a safe region for surgery. Adjacent anatomical structures need to be thoroughly evaluated prior to interventions such as implant surgery, bone grafting, endodontic surgery, removal of an impacted canine or a supernumerary tooth, orthognathic surgery, and cyst enucleation.12 The nasopalatine canal and the nasal floor can be easily identified on conventional radiographs and are important anatomical landmarks in the anterior maxilla; however, recent publications have focused on other structures that should be considered to ensure a relatively safe surgical procedure in this region.3
The use of cone-beam computed tomography (CBCT) allows a 3-dimensional evaluation of the jaws; thus, surgeons can obtain more detailed and accurate information about the quality and quantity of the bone, helping them to identify anatomical features. Prior to a surgical procedure, a careful preoperative examination is necessary to avoid complications and to take the appropriate precautions. More attention should be paid to the detection of small neurovascular bundles to reduce the risk of injury. Surgical manipulation of these bundles can lead to hemorrhage and nerve deficits such as paresthesia, anesthesia, and pain.13456
On CBCT images, a twisted bone canal originating laterally from the infraorbital canal on the orbital surface can be detected in the anterior maxilla. This small, poorly recognized bony canal known as the canalis sinuosus (CS) is a normal anatomical structure. The canal was given this name because of its double curved course. The CS originates laterally from the infraorbital canal approximately 25 mm behind the infraorbital foramen (IOF).67 It descends to the orbital floor lateral to the infraorbital canal, curves medially at the anterior wall of the maxillary sinus, and then passes below the IOF to the margin of the anterior nasal aperture in front of the anterior end of the inferior concha. It has visible neurovascular branches that form the dental plexus in the canine region. Its terminal branches follow the lower margin of the aperture and open in front of the incisive canal.8 The CS can be divided into 3 sections: the orbital floor part, the transverse facial part, and the circumnarial part.569 It contains the anterior superior alveolar nerve (ASAN), along with veins and arteries. Further, this canal innervates the incisors and the canines, as well as the adjacent soft tissues.
Many surgeons do not know much about this anatomical structure, and currently, very few publications on the CS are available. The aim of this study was to evaluate the course of the CS using CBCT in patients with a maxillary impacted canine, to determine its diameter and distance to the impacted canine and to the alveolar bone crest, and to identify any variations of the canal. Further, possible correlations with patient gender and age were analyzed.
This was a retrospective study approved by the Ethical Committee of Istanbul Medipol University. The CBCT images of 111 randomly selected patients who presented to our clinic for the exposure or extraction of maxillary impacted canines were included in this study. The patients had no history of trauma or surgery at the anterior maxilla, nor any pathological formations. Maxillary CBCT images were obtained from these patients under standard conditions (field of view, 16 cm×8 cm; slice thickness, 0.2 mm) by an i-Cat CBCT device (Imaging Sciences International Hatfield, PA, USA).
All the obtained images were evaluated twice by the same experienced observer at a 1-month interval. Axial, coronal, sagittal, and cross-sectional sections with a thickness of 1 mm were evaluated to assess the prevalence of CS, direction and diameter of the canal, its relation with the impacted canine and distance from the alveolar crest, and the largest diameter of the canal after the bifurcation site on the coronal views in i-Cat. Canal diameters of the patients were compared between sides involving and not involving the impacted canine, and possible correlations with patient gender and age were analyzed.
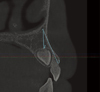
The smallest distance between the impacted canine and the CS was determined by measuring several points on the cross-sectional and coronal views. Possible associations between the position of the impacted tooth and the smallest distance were analyzed. The distance between the terminal portion of the CS and the region of the buccal alveolar ridge was measured on the sagittal plane (Fig. 1). If the canal ended in the anterior palatine region with additional foramina, the distance was determined to be zero.
To assess the results, a statistical analysis using IBM SPSS version 22 (IBM SPSS, Armonk NY, USA) was performed. Compliance with a normal distribution of the parameters was evaluated using the Shapiro-Wilk test. The Student t-test was used for analyzing the descriptive statistical parameters (mean, standard deviation, and frequency) and for comparing the quantitative data and the normal distribution showing the parameters between the 2 groups. The Mann-Whitney U test was used for assessing parameters that did not show a normal distribution between the 2 groups. Further, 1-way analysis of variance was used for comparisons between more than 2 groups of parameters with a normal distribution. The Fisher exact test was used for comparing the qualitative data. P values <.05 were considered to indicate statistical significance.
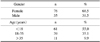
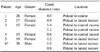
CBCT scans of 111 patients were assessed. The sample consisted of 76 (68.5%) females and 35 (31.5%) males. The mean age of the patients was 21.39±12.26 years (range, 12-79 years). Sixty-one of these patients (55%) were under the age of 18 years, whereas 39 (35.1%) were in the age group of 18-35 years, and 11 (9.9%) were older than 35 years. Twenty-two patients had bilateral impacted canines, and 89 patients had unilateral impacted canines, with a total of 133 impacted canines examined (Table 1).
The CS was observed bilaterally in all the samples; therefore, the 111 patients presented a total of 222 canals in the anterior maxilla. The average canal diameter was 1.37 mm (range, 0.75-2.25 mm). The mean canal diameter in the males was significantly higher than that in the females (P=.001) (Table 2). Furthermore, the canal diameter did not show a statistically significant difference between the sides with and without the impacted canine (P=.664) (Table 2). The average distance between the terminal portion of the CS and the buccal alveolar ridge was 16.81 mm (range, 0-23.5 mm). The smallest distance between the impacted canine and the CS was 0.75 mm, with a mean of 5.27 mm.
The impacted teeth could be located in 3 positions: horizontal, oblique, and vertical. The smallest distance was significantly shorter in the horizontal position than in the other positions of the impacted tooth (P=.030). However, no statistically significant difference was observed between the other 2 positions.
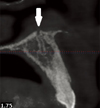
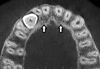
In almost all the samples, the CS terminated near the incisive canal on the nasal floor. Only in 1 case did the terminal portion of the CS merge superiorly with the nasopalatine canal (Fig. 2). A few of the patients had anatomical variations associated with the CS. Accessory bony canals presented as a direct extension of the CS, which ran downward towards the alveolar ridge (Fig. 3). In 6 cases, 8 accessory canals and foramina were registered. The mean diameter of the additional foramina measured on the axial images was 1.06 mm (range, 1.41-0.89 mm). Their location was variable, but the most common location was palatal to the lateral incisors (62.5%) (Table 3).
The presence of neurovascular bundles in the surgical field can adversely influence the surgical outcome. Many professionals are not aware of the CS, which contains the ASAN. The ASAN is a division of the maxillary branch of the trigeminal nerve that follows the anterior maxilla to innervate the central and lateral incisors and the canines. Previous studies indicated that the CS rose laterally to the IOF, but a recent study showed that the CS emerged medially, centrally, and laterally to the IOF in 15%, 43%, and 43% of cases, respectively.10
Heasman et al.9 determined the position of the origin of the ASAN in 20 cadaver heads. It emerged from the infraorbital nerve at distances between 2 mm and 20 mm from the IOF, and the vertical distance from the inferior margin of the IOF to the superior border of the CS ranged between 0 mm and 3 mm. A total of 111 patients were randomly selected from our hospital files. We found that the CS was a common anatomical structure and that it could be observed bilaterally in the CBCT scans of all the patients. The CS was observed bilaterally in 87% of the patients and unilaterally in 1% in a previous study by Wanzaler.1 This difference may be related to the quality or thickness of the image slices and the fact that canals with a diameter of less than 1 mm were also considered in our study.
The CS frequently ends on the lower border of the nasal aperture; however, it may extend to the alveolar ridge and can rarely be found close to the incisors' apical region. Shelley et al.11 reported a case in which a well-defined radiolucency simulating a pathologic lesion was recognized around the top-left canine apex. Further radiographs and detailed clinical examinations proved that it was a variation of the CS. Because of its proximity to the upper teeth, the CS may be inaccurately diagnosed; hence, inappropriate treatment may be applied. Only in 1 case did we observe that the canal joined the nasopalatine canal superiorly and could form an anastomosis with the incisive nerve.
Impacted canines more commonly lead to some problems in patients aged ≤39 years or >60 years when they need removable dentures. In the present study, 133 impacted canines were examined in 111 patients; 89 of these patients had unilateral impacted canines, and 22 had bilateral impacted canines. The smallest distance from the CS to the impacted tooth was 0.75 mm, and the average distance was 16.81 mm. Because of the small distance, the canal may be damaged during surgical interventions involving the removal of an impacted canine, particularly in the horizontal position; thus, more attention should be paid in these cases.
In this study, the mean diameter of the CS was 1.37 mm. With respect to patient age, no statistically significant change was observed in the canal diameter. The presence of impacted canines also had no influence on the canal diameter. In contrast, the canal diameter was larger in males than in females. This result may be related to the wider anatomical structures in males.
Injury of the ASAN in patients with midface fractures can cause sensory disturbances including hypoesthesia, hyperesthesia, paresthesia, and neuropathic pain localized to the incisors, canines, and the anterior maxilla. Following a trauma, obliteration of the CS and formation of neuromas could be responsible for post-traumatic midface pain. The anterior surface of the canal is covered by a thin bone that makes the ASAN susceptible to injury after trauma. The integrity of the CS may be disrupted in the case of craniofacial injury, as well as during Le Fort I osteotomy and dental surgery.12
Previous studies have shown that accessory canals with various sizes and contents can exist in the premaxilla. In fact, von Arx et al.2 evaluated the frequency of accesso-ry canals in 176 cases and reported that more than half of the accessory canals communicated with the CS. The contents of the other small canals are as yet unknown. In a study of preoperative CBCT images, Neves et al.4 observed that bilateral canals related to the CS extended to the foramina located in the hard palate adjacent to the lateral incisor. During surgery, these foramina and neurovascular bundles became visible after a careful dissection of the periosteum. If surgeons do not consider the presence of these variations during a surgical procedure, such as the removal of the impacted canine, then neurosensory disturbances, extensive bleeding, and/or other complications may occur. Surgical damage to the CS can cause some neuronal dysfunction; therefore, further studies assessing the relationship between clinical evidence and possible injury of the canal are required to clarify the importance of this anatomical structure. The existing studies are based on radiographic findings, and clinical observations and anatomical dissections are lacking.
In this radiological study, 8 accessory canals opening into the foramina on the anterior palate were described as a direct extension of the CS. Two patients had bilateral canals and foramina, and 4 others had unilateral canals. Most of the foramina were located palatal to the lateral incisor. With respect to gender, a higher frequency of additional canals was observed in females; however, the number of females considered was almost twice that of the males considered. Moreover, a few samples had accessory canals. Therefore, a statistical comparison of these findings would not be appropriate.
Older individuals tended to have more than one accessory canal, and none of the patients under 20 years of age presented with an accessory canal in the study of von Arx et al.2 However, in this study, 5 of the 6 patients who had an accessory canal were under 20 years of age. Furthermore, Sekerci et al.13 analyzed the presence of the accessory foramina and canals having a diameter of at least 1 mm within the premaxilla in 368 pediatric patients using CBCT. Eighty-two patients had additional canals; in 6 of them, the canals presented as a direct extension of the CS.
Walzeler et al.1 evaluated the CBCT images in 100 patients and classified the site of bifurcation using the nasal cavity as a reference. The branch point of the CS from the infraorbital canal was located just below the orbital floor and was always above the floor of the nasal cavity. Accordingly, the description of the bifurcation site as being above or below the nasal cavity floor was redundant. Patients who had a pathologic lesion were excluded in our examination; however, pathologies in the anterior maxillarymaxillary region, such as cysts and odontomas, can contain the CS.
This article emphasizes that a presurgical radiological examination of the CS is essential for evaluating the possibility that it may be located very close to the impacted canine. The CS and its anatomical variations should be considered, particularly when its branches are located close to the teeth and run towards the alveolar ridge. Careful presurgical imaging analyses of the neurovascular structures and individual variations in the maxilla and the mandible, such as the CS, should be performed to ensure safer surgical procedures on the basis of improved knowledge of the macroscopic and microscopic anatomy. Unidentified pain with some sensory changes after trauma or surgery can be associated with the injury of the CS; thus, the presence of this canal should be considered.
Figures and Tables
References
1. Wanzeler AM, Marinho CG, Alves Junior SM, Manzi FR, Tuji FM. Anatomical study of the canalis sinuosus in 100 cone beam computed tomography examinations. Oral Maxillofac Surg. 2015; 19:49–53.

2. von Arx T, Lozanoff S, Sendi P, Bornstein MM. Assessment of bone channels other than the nasopalatine canal in the anterior maxilla using limited cone beam computed tomography. Surg Radiol Anat. 2013; 35:783–790.

3. Tanaka R, Hayashi T, Ohshima H, Ida-Yonemochi H, Kenmotsu S, Ike M. CT anatomy of the anterior superior alveolar nerve canal: a macroscopic and microscopic study. Oral Radiol. 2011; 27:93–97.

4. Neves FS, Crusoé-Souza M, Franco LC, Caria PH, Bonfim-Almeida P, Crusoé-Rebello I. Canalis sinuosus: a rare anatomical variation. Surg Radiol Anat. 2012; 34:563–566.

5. Torres MG, de Faro Valverde L, Vidal MT, Crusoé-Rebello IM. Branch of the canalis sinuosus: a rare anatomical variation-a case report. Surg Radiol Anat. 2015; 37:879–881.

6. de Oliveira-Santos C, Rubira-Bullen IR, Monteiro SA, León JE, Jacobs R. Neurovascular anatomical variations in the anterior palate observed on CBCT images. Clin Oral Implants Res. 2013; 24:1044–1048.
7. Jones FW. The anterior superior alveolar nerve and vessels. J Anat. 1939; 73:583–591.
8. von Arx T, Lozanoff S. Anterior superior alveolar nerve (ASAN). Swiss Dent J. 2015; 125:1202–1209.
9. Heasman PA. Clinical anatomy of the superior alveolar nerves. Br J Oral Maxillofac Surg. 1984; 22:439–447.

10. Robinson S, Wormald PJ. Patterns of innervation of the anterior maxilla: a cadaver study with relevance to canine fossa puncture of the maxillary sinus. Laryngoscope. 2005; 115:1785–1788.

11. Shelley AM, Rushton VE, Horner K. Canalis sinuosus mimicking a periapical inflammatory lesion. Br Dent J. 1999; 186:378–379.

12. Olenczak JB, Hui-Chou HG, Aguila DJ 3rd, Shaeffer CA, Dellon AL, Manson PN. Posttraumatic midface pain: clinical significance of the anterior superior alveolar nerve and canalis sinuosus. Ann Plast Surg. 2015; 75:543–547.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download