Abstract
A 21-year-old woman presented with facial asymmetry. Crepitus and clicking of the temporomandibular joint were noted. The midline deviated 5.5 mm to the left, and secondary malocclusion was observed. Panoramic and cone-beam computed tomographic images showed an irregular and exophytic bony mass on the anteromedial surface of the right mandibular condyle. A 3-phase bone scan revealed increased tracer uptake on the affected side. The lesion was treated with excision and reshaping under the diagnosis of osteochondroma confirmed by a histopathological examination. The lesion recurred after 3 years, and the patient underwent condylectomy. Mandibular condylar osteochondroma is often resected because it causes functional and aesthetic problems, but it rarely recurs. To the best of our knowledge, only 2 cases of recurrent osteochondromas of the mandibular condyle have been reported previously. Surgical treatment of the osteochondroma should be performed considering the possibility of recurrence, and long-term follow-up is recommended.
In 2002, the World Health Organization defined osteochondroma as a cartilage-capped bony exostosis on the external surface of a bone containing a marrow cavity continuous with that of the underlying bone.1 Osteochondroma accounts for approximately 35% to 50% of all benign bone tumors and 8% to 15% of all primary bone tumors.2 It can develop in any bone that is generated by endochondral ossification and is known to occur in almost every portion of the craniofacial skeleton, such as the skull base, maxillary sinus, zygomatic arch, nasal septum, and mandible.3 The mandibular condyle and the coronoid process are by far the most common sites of craniofacial osteochondroma.2 The clinical symptoms of mandibular condylar osteochondromas are facial asymmetry, cross-bite on the unaffected side, open bite on the affected side, a deviated opening path, condylar motion limitation, disc displacement, and rarely, pain.45 While long-bone osteochondromas are usually asymptomatic and do not require surgery, resection is often appropriate for mandibular condylar osteochondromas because they cause functional and cosmetic problems6 and very rarely recur after treatment. This report documents the case of a 21-year-old woman with mandibular condylar osteochondroma that recurred with a pattern similar to the original occurrence 3 years after the first excision and reshaping.
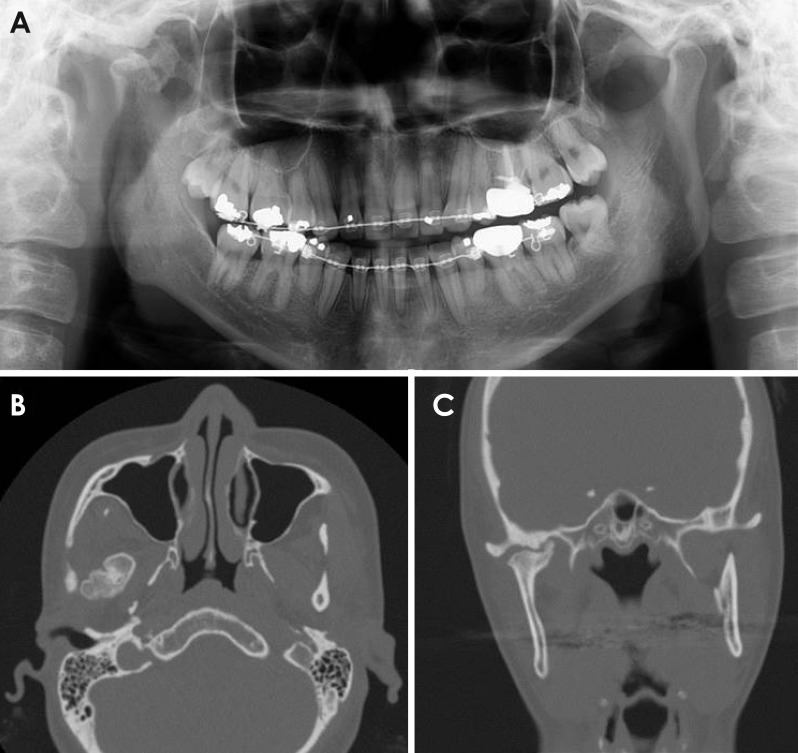
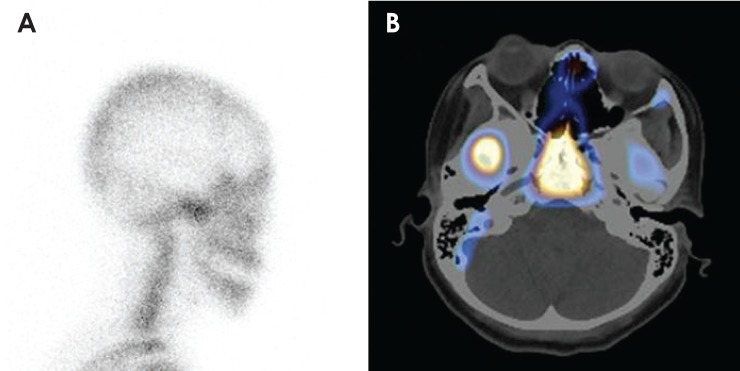
A 21-year-old woman was referred to the Department of Oral and Maxillofacial Surgery, Kyungpook National University Dental Hospital, with facial asymmetry that was noticed 4 years ago. She had no history of facial trauma or ear infection. Crepitus and clicking were noted on the left and right temporomandibular joints, respectively, but pain was absent. The active range of motion was normal at 40 mm; however, the midline deviated 5.5 mm to the left and secondary malocclusion was observed during a physical examination (Fig. 1). A panoramic image (Orthopantomograph OP 100D, Instrumentarium Imaging, Tuusula, Finland) revealed an irregular bony outgrowth on the anterior portion of the right condylar head (Fig. 2). Cone-beam computed tomography (CBCT) images were acquired with Pax-Flex 3D (Vatech, Seoul, Korea), using a 120 mm×85 mm field of view at 90 kVp and 10 mA. A well-defined exophytic bony mass was observed on the anteromedial surface of the condylar neck, which presented as a bifid condylar head and caused a depression of the skull base (Fig. 3). A 3-phase bone scan was performed after intravenously injecting 20-mCi 99mTc-hydroxydiphosphonate (HDP); this revealed increased tracer uptake on the affected side (Fig. 4). Under the provisional diagnosis of osteochondroma, the mass was resected by simple surgical excision and condylar reshaping was performed under general anesthesia using a preauricular approach. The removed mass had the following dimensions: 20 mm×20 mm×18 mm (Fig. 5). A histopathological examination showed the presence of a fibrous perichondrium, chondroblasts, and chondroid matrix with chondrocytes in the lacuna. The endochondral ossification had matured into a cancellous bone with marrow, and the cartilaginous tissue was seen blending with the cancellous bone. The histopathological findings were consistent with osteochondroma (Fig. 6). Further follow-up was scheduled after 6 months, but the patient did not present for the follow-up. After 3 years, the patient visited again, complaining of a sudden deviation of the mandible to the left during orthodontic treatment. A physical examination revealed a slight facial asymmetry and open bite in the anterior and left posterior areas. A similar pattern of bony outgrowth of the right condyle was observed on the panoramic radiograph and contrast-enhanced computed tomography (CT) (Optima CT660, GE Healthcare, Milwaukee, WI, USA) images (Fig. 7). Single-photon emission CT (SPECT) (Discovery NM/CT 670, GE Healthcare, Milwaukee, WI, USA) with 99mTc-HDP was used for examining the recurrence of the lesion. The 3-phase bone scan and axial-fused SPECT/CT images revealed intense uptake in the right condylar area (Fig. 8). More radical treatment was planned for the recurrent lesion, and condylectomy was performed without reconstruction. A histological analysis revealed that the lesion was consistent with osteochondroma. Physical and radiographic examinations performed during the postoperative follow-up at 6 months were uneventful.
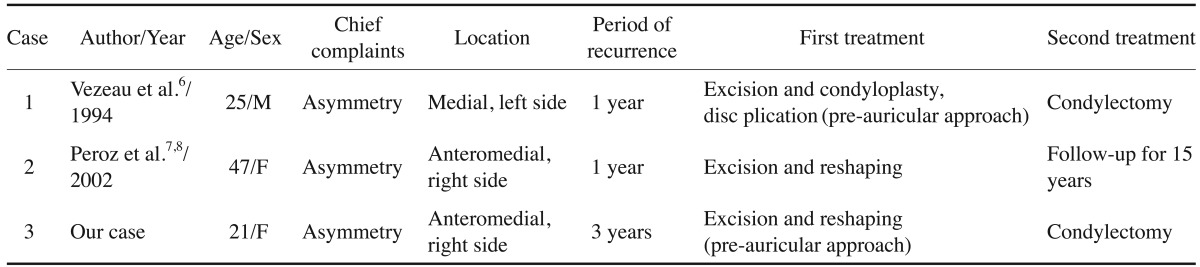
We report a case of recurrent osteochondroma of the mandibular condyle that was initially managed by conservative surgical treatment considering the patient's age. Among the 235 cases of osteochondroma reviewed by Vezeau et al.6 and Peroz.7 in the English literature from 1927 to 2015, only 2 recurrent cases were reported. Therefore, to the best of our knowledge, only 3 recurrent cases of osteochondroma, including the present case, have been reported to date (Table 1). In one of the previously reported cases, the patient was surgically treated twice, and in the other, the patient was under observation for 15 years after the first operation. All lesions were located on the medial side of the condyle, and were on the anterior side in 2 cases. While mandibular condylar osteochondromas have a broad age distribution, ranging from 13 years to 76 years (mean, 41 years),7 recurrent cases are more likely to occur at a young age (recurrence occurred in the third decade of life in 2 of the 3 cases). Two of these 3 patients with recurrence were women; they presented with facial asymmetry as the main symptom and received simple resection initially. Two of the recurrent osteochondromas were detected by a routine radiographic examination without symptoms 1 year later, while the third was discovered after 3 years and was accompanied by asymmetry. While the recurrence rate of osteochondroma in the long bones was 2%, the recurrence rate of mandibular condylar osteochondroma, including this case, was 1.3% (3 out of 236 cases). However, perhaps due to the lack of long-term follow-up, we observed that the recurrent osteochondroma of the mandibular condyle had a border smaller than that of the original lesion. Further studies are needed on the recurrence of osteochondroma.
The cause of osteochondroma is presumed to be the protrusion of cartilaginous precursor cells through a defect in the epiphyseal plate, the migration of precursor cells from the epiphyseal to metaphyseal area, the hyperplasia of cartilaginous cells due to tensional forces, and the differentiation of pluripotent cells in the periosteum into chondroblasts or osteoblasts.6 Hyperplasia of cartilaginous cells by tensional forces is the strongest hypothesis, because condylar osteochondromas occur commonly on the medial side (57%), followed by the anterior side (20%), and almost none occur in the lateral or superior aspects (<1%).8 This is supported by the theory of hyperplastic changes in embryonic cartilaginous potential cells at the position of tendon insertions. Sequential forces at the insertion site of the lateral pterygoid muscle may cause a local accumulation of these cells.25
Mandibular condylar osteochondroma appears as a mixed-density mass on panoramic radiographs because of the cartilage component and the calcified bone coexisting in the lesion, and the density increases with an increase in the calcified tissue.9 CT can reveal the calcified cartilaginous cap and anatomical location of the lesion and may help in preoperative treatment planning.10 Magnetic resonance imaging can help confirm the cartilaginous cap, which is characteristic of osteochondroma.9 Moreover, a bone scan can help identify abnormal metabolic bone activity through increased uptake of 99mTc-HDP in the affected condylar region, as seen in the present study. In most studies, the radiological appearance of condylar osteochondroma is described as nodular or mushroom-like.9 However, adjoining structures such as the joint tuberosity, joint space, joint fossa, and joint capsule may affect the shape of the lesion by limiting the lesion growth.9 In the present case, the presence of an exophytic radiopaque mass protruding from the affected condylar neck to the anteromedial side suggested that its appearance was affected by the surrounding structure.
Benign tumors that mainly develop in the condyle include osteochondroma, osteoma, chondroma, condylar hyperplasia, condylar giant cell tumor, fibro-osseous lesions, and vascular malformations.6 In the present case, osteochondroma, osteoma, and chondroma were included in the differential diagnosis. Osteoma could be excluded because it usually appears as a pedunculated osseous mass on the mandibular condyle or neck, unlike the broad base seen in our case.4911 Chondroma, a benign tumor that forms mature cartilage, is characterized radiologically by the presence of a mainly radiolucent and irregular mass, which can be distinguished from osteochondroma.1213 Osteochondromatosis was also ruled out because no hot spots other than the mandibular condyle were observed on the bone scan.6
Condylar osteochondroma can be monitored without surgical intervention when it is asymptomatic and determined to be stable by routine radiological and clinical examinations.14 However, most cases are treated surgically. Radical resection such as condylectomy is the traditional treatment with or without reconstruction.5 In contrast to this invasive surgical method, some authors recommend preserving as much of the condyle as possible,7 because the recurrence rate after surgical excision has been reported to be 2% in solitary osteochondroma cases of the long bone.3515 Conservative methods have the advantage of preserving the vertical height and allowing stable occlusion, simplifying the procedure and eliminating the need for additional reconstruction.315 In the present case, the first surgical procedure was conservative, involving surgical excision and condylar reshaping using the pre-auricular approach, considering the patient's age, although the lesion recurred 3 years later. This suggests that condylar osteochondroma treated conservatively can recur and that long-term follow-up is required for the surveillance of recurrence.
In conclusion, we reported a case of recurrent osteochondroma of the mandibular condyle that was treated conservatively. Complete removal of the lesion and long-term follow-up are recommended for the prevention of recurrence, despite the benign neoplastic nature of this osteochondroma.
References
1. Zhou Q, Yang C, Chen MJ. Osteochondroma of bilateral mandibular condyle: a case report. Int J Clin Exp Med. 2015; 8:2989–2992. PMID: 25932269.
2. Karras SC, Wolford LM, Cottrell DA. Concurrent osteochondroma of the mandibular condyle and ipsilateral cranial base resulting in temporomandibular joint ankylosis: report of a case and review of the literature. J Oral Maxillofac Surg. 1996; 54:640–646. PMID: 8632254.
3. Aydin MA, Küçükçelebi A, Sayilkan S, Celebioğlu S. Osteochondroma of the mandibular condyle: report of 2 cases treated with conservative surgery. J Oral Maxillofac Surg. 2001; 59:1082–1089. PMID: 11526583.
4. Arora P, Deora SS, Kiran S, Bargale SD. Osteochondroma of condyle: case discussion and review of treatment modalities. BMJ Case Rep. 2014; 2014:pii: bcr2013200759.

5. Wolford LM, Mehra P, Franco P. Use of conservative condylectomy for treatment of osteochondroma of the mandibular condyle. J Oral Maxillofac Surg. 2002; 60:262–268. PMID: 11887135.

6. Vezeau PJ, Fridrich KL, Vincent SD. Osteochondroma of the mandibular condyle: literature review and report of two atypical cases. J Oral Maxillofac Surg. 1995; 53:954–963. PMID: 7629631.
7. Peroz I. Osteochondroma of the condyle: case report with 15 years of follow-up. Int J Oral Maxillofac Surg. 2016; 45:1120–1122. PMID: 27156430.

8. Peroz I, Scholman H, Hell B. Osteochondroma of the mandibular condyle: a case report. Int J Oral Maxillofac Surg. 2002; 31:455–456. PMID: 12361086.

9. Zhang J, Wang H, Li X, Li W, Wu H, Miao J, et al. Osteochondromas of the mandibular condyle: variance in radiographic appearance on panoramic radiographs. Dentomaxillofac Radiol. 2008; 37:154–160. PMID: 18316507.

10. Avinash KR, Rajagopal KV, Ramakrishnaiah RH, Carnelio S, Mahmood NS. Computed tomographic features of mandibular osteochondroma. Dentomaxillofac Radiol. 2007; 36:434–436. PMID: 17881606.

11. Kondoh T, Seto K, Kobayashi K. Osteoma of the mandibular condyle: report of a case with a review of the literature. J Oral Maxillofac Surg. 1998; 56:972–979. PMID: 9710193.

12. Chandu A, Spencer JA, Dyson DP. Chondroma of the mandibular condyle: an example of a rare tumour. Dentomaxillofac Radiol. 1997; 26:242–245. PMID: 9442616.

13. Dhirawani RB, Anand K, Lalwani G, Pathak S, Thakkar B. True chondroma of the mandibular condyle: a rare case. Ann Maxillofac Surg. 2014; 4:220–223. PMID: 25593880.

14. Ward BB, Pires CA, Feinberg SE. Osteochondromas of the mandible: case reports and rationale for treatment. J Oral Maxillofac Surg. 2005; 63:1039–1044. PMID: 16003637.

15. Ortakoglu K, Akcam T, Sencimen M, Karakoc O, Ozyigit HA, Bengi O. Osteochondroma of the mandible causing severe facial asymmetry: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 103:e21–e28. PMID: 17331758.

Fig. 1
A. Preoperative photograph shows facial asymmetry with chin deviation to the left side. B. Intraoral photograph reveals midline deviation to the left (arrow) and secondary malocclusion in the closed position.

Fig. 2
Panoramic radiograph reveals an irregular and large bony mass extending from the anterior portion of the right condylar head.

Fig. 3
A-C. Cone-beam computed tomography (CBCT) images demonstrate the well-defined margin of the radiopaque mass on the anteromedial surface of the condylar neck (arrow) with a focal erosive change (dotted arrow). Depression and cortical thickenings of the skull base (arrowhead) can also be seen.
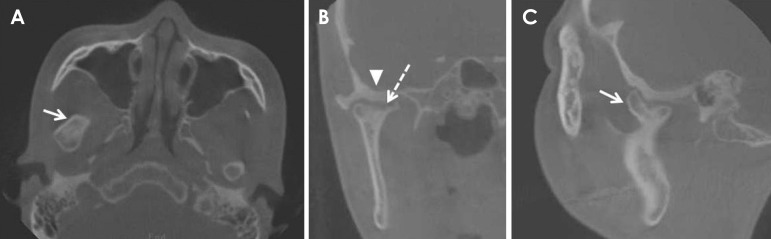
Fig. 4
A. 99mTc-hydroxydiphosphonate bone scan, with a lateral spot view, showing an abnormal tracer uptake in the right condylar head. B. No significant tracer avidity is seen on the left side.
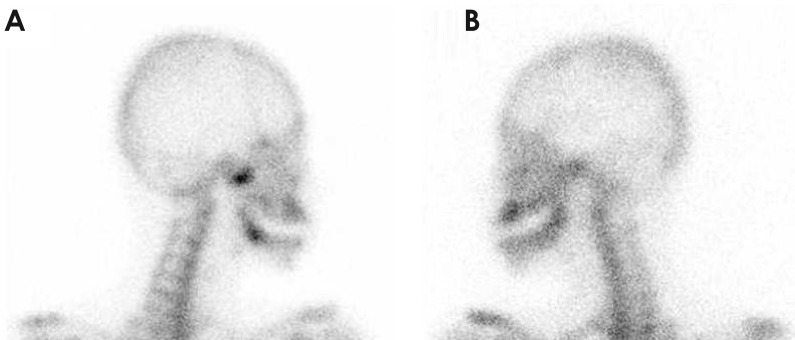
Fig. 5
A. A pre-auricular approach was used for exposing the condyle. B. The surgical specimen was approximately 20 mm in length.
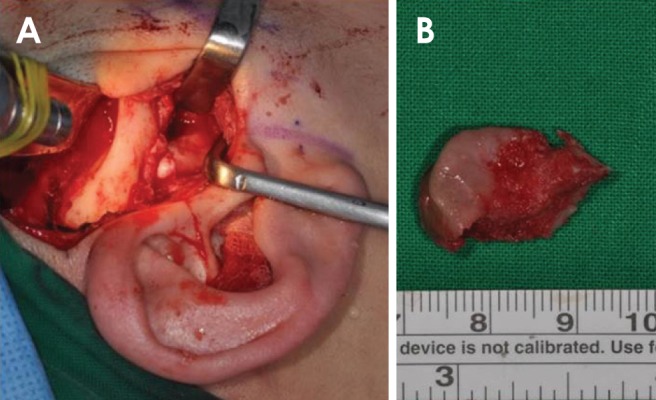
Fig. 6
Osteochondroma showing a fibrous perichondrium and chondroid matrix with chondrocytes in the lacuna. The cartilaginous tissue is seen blending with the cancellous bone (hematoxylin and eosin, original magnification: ×200).
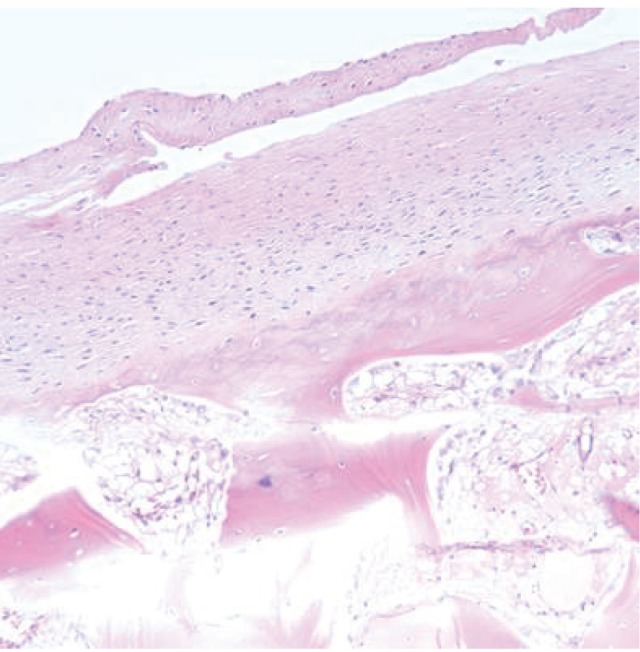
Fig. 7
A. Panoramic radiograph of recurred osteochondroma shows the exophytic mass on the right condyle. B-C. An axial and coronal computed tomograph shows a similar pattern of bony outgrowth on the affected side.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download