Abstract
Mandibular bone depression, also known as Stafne bone cavity, is defined as a bone depression filled mainly with salivary gland tissue. Parotid gland bone defects are infrequently observed. We report the case of a 52-year-old male patient who underwent radiographic examinations due to temporomandibular joint dysfunction, and a radiolucent area was detected in the mandibular ramus, with a provisional diagnosis of traumatic bone cyst or parotid mandibular bone defect. The patient was then referred for magnetic resonance imaging, which demonstrated a hyperintense area eroding the mandibular ramus, which corresponded to glandular tissue. Although the defect was a benign lesion, radiolucencies in the mandibular ramus lead to concerns among professionals, because their radiographic features can resemble various intrabony neoplastic lesions, such as giant cell tumors or benign tumors of the parotid gland.
Mandibular bone depression (MBD) or Stafne bone cavity was first described by Edward Stafne in 1942 as an asymptomatic, well-defined, radiolucent defect located on the posterior and medial surfaces of the mandible.1 Many other names have been applied to describe this lesion, such as latent/idiopathic/developmental bone cavity and cortical mandibular depression.2 It is considered a pseudocyst due to the absence of an epithelial lining. The content of these cavities has been described as mainly salivary gland tissue.34 Muscles, fat or lymphoid tissue, blood vessels, and/or connective tissue can also be found.35
The etiology and pathogenesis of MBD remains controversial and poorly understood.46 The first theory, advocated by Stafne,1 was that a portion of the salivary gland becomes entrapped during the development and ossification of the mandible. However, it has been pointed that the depression may originate from a salivary gland hypertrophic lobe,6 or may be the result of a vascular compression erosion,45 glandular mechanical pressure,7 or even incomplete calcification of Meckel cartilage during ossification.58
The defect itself takes years to develop and can be detected in routine radiographs, rarely before the fifth to sixth decades,68 although the youngest patient reported in the literature was 11 years old.9 It is mostly seen in male patients.1011 MBDs are primarily asymptomatic,21213 and in very rare cases can be palpated, due to the missing bone surface.14
Four variants of MBD have been described: lingual posterior,15 lingual anterior, lingual ramus, and buccal ramus depressions, in decreasing order of frequency.216 Parotid gland depressions at the mandibular ramus are infrequently observed.217 MBDs can present, also in decreasing frequency, as unilateral, bilateral,2 or multiple depressions,6 and they usually are discovered incidentally in routine radiographic examinations due to their lack of symptoms.256 Although MBDs are benign, the identification of the traditional MBD (inferior to the mandibular canal in the mandibular body) is critical to dental practitioners; unusual variants in the ascending ramus lead to even more concerns217 because their radiographic features can resemble various intrabony neoplastic lesions.10
In the present report, we describe the case of a parotid MBD found in a temporomandibular joint (TMJ) radiographic examination; the final diagnosis of which was confirmed as parotid MBD after magnetic resonance imaging (MRI) demonstrated the presence of glandular tissue in the defect.
In the beginning of November 2015, a male Asian patient (52 years old) noticed major discomfort and pain in his left TMJ. A week later, as the symptoms got worse and the patient began to experience difficulties in fully opening his mouth. He visited his general dentist, who observed that the patient had an evident limitation in fully opening his mouth (maximum mouth opening of 16 mm), with a discrete clicking noise and without deviation when opening.
An extraoral examination demonstrated the absence of asymmetry or bulging, but pain was confirmed when the left-side TMJ was palpated. An intraoral examination did not evince any disease of odontogenic etiology. The patient's medical history was not significant.
The general dentist suspected that the patient was affected by temporomandibular disorder and disc displacement. The patient was then medicated with analgesics (500 mg of paracetamol twice a day for 1 week) and radiographic examinations were carried out, with a provisional diagnosis of temporomandibular dysfunction.
Then, on the radiographic examination, the clinician observed a radiolucent lesion in the superior posterior border of the mandibular ramus (left side). Considering that lesions in mandibular ramus may cause neurological disorders, the dentist checked whether the patient had any neurological complaints, such as paresthesia on the left side of the mandible, but the patient did not report any neurological symptoms. The patient was therefore referred to the university clinic.
The panoramic radiograph revealed an oval-shaped radiolucency with well-defined borders that was unilocular and located near the upper third of the ramus, posterior to the mandibular foramen, and close to the mandibular posterior margin. The lesion was homogeneously radiolucent, had no sclerotic margins, no contiguity with the mandible border, and measured about 1 cm in its largest diameter. No alterations were observed in the surrounding tissues, such as periosteal reaction or anatomical structure displacement, as demonstrated in Figure 1.
Open- and closed-mouth TMJ radiographs of the patient were also available, and they confirmed the presence of the oval radiolucency on the left border of the mandibular ramus with radiographic characteristics similar to those observed in the panoramic radiograph (Fig. 2). The TMJ evaluation established that the position of the mandibular condyles was posterior to the articular eminence when the patient's mouth was open, suggesting a reduction of condylar translation.
The patient was then referred for MRI to investigate TMJ alterations that might explain the symptoms and confirm the diagnosis of temporomandibular dysfunction. For the radiolucent area, provisional diagnoses of traumatic bone cyst and parotid MBD were also considered.
MRI was performed in a 3-T system (Siemens Magnetom Skyra, Siemens, Munich, Germany) using dedicated head and neck surface coils. Axial T1- and T2-weighted images were obtained. The section thickness was 4 mm.
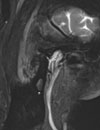
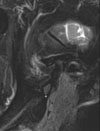
On MRI, abnormal findings of the bilateral joint discs were not observed, despite the limitation of mouth opening, and the patient's symptoms were relieved by analgesic medications. At the same time, the radiolucent lesion was also further investigated. An axial scout image (Fig. 3) demonstrated a tiny hyperintense image eroding the left mandibular ramus on the lingual side, which corresponded to continuous glandular tissue from the parotid gland. A proton-weighted image (Fig. 4) and T2-weighted images (Fig. 5) exhibited a well-defined hyperintense signal area on the mandibular ramus, surrounded by a thick cortical bone-like area with a hypointense signal.
Due to the imaging characteristics demonstrated by MRI, it was concluded that the well-defined hyperintense area observed in Figures 4 and 5 was glandular tissue, and other types of bone lesions were then disregarded. The bone cavity was filled by soft tissue, clearly continuous to the parotid gland. The adipose tissue within the glandular cells was responsible for the hyperintense image detected in the T2-weighted sequences.
After the final diagnosis of parotid MBD was made by MRI and the TMJ symptoms completely disappeared, the patient did not come back for regular follow-up visits.
MBDs from any salivary gland are unusual, with a prevalence of about 0.5%,18 and they are mostly seen in panoramic radiographs as a posterior lingual depression on the mandible,27 located between the bicuspid and first molar,4 or in the mandibular angle, below the mandibular canal.2 Parotid gland MBD was first described in 1985,1920 and it may be referred to as the “ramus variant.” It is less frequent than the variant located in the mandibular angle,26 making it a diagnostic challenge for the clinical practitioner or oral radiologist. To our knowledge, only 7 cases of parotid MBD have been previously described in the literature.8171920212223
On panoramic radiographs, MBDs classically exhibit a dense circumscribed unilocular4 area of radiolucency,2 with an oval or round shape and well-defined limits.6 Although MBD is most characteristically unilocular, a multilocular aspect has also been previously reported, as well as irregular borders.4 The border of the defect may also have a radiopaque line.6 The diagnosis of typically-appearing MBDs can easily be made with a panoramic radiograph.2 The greatest disadvantage of panoramic radiographs in diagnosing MBDs is the lack of information about continuity of the anterior mandible border due to the technical limitations inherent to 2-dimensional examinations. Computed tomography can demonstrate the margins of the mandible; eventually the defect may interrupt the continuity of the inferior border of the mandible.415 Nevertheless, in atypical cases such as the one described in this report, advanced imaging investigations need to be carried out4 in order to eliminate the possibility of a potentially harmful lesion.215
Manifold radiologic methods have been suggested to assess the presence of salivary gland tissues inside bone defects.616 MRI can offer better resolution when investigating soft tissues, and has the advantages of multiple imaging planes and not exposing the patient to ionizing radiation.4 The diagnosis of MBD may be confirmed with a limited MRI examination, without exposing the patient to other ionizing radiographic techniques. MRI can demonstrate a mandibular defect containing soft tissue from the submandibular gland, which appears hyperintense on both T1- and T2-weighted sequences.4 Intravenous contrast material is not necessary to diagnose an MBD if the inherent soft-tissue contrast is adequate.4 Sialography may also be an option for diagnosing MBDs,7 and it can determine whether glandular tissue is present in the defect.15
The differential diagnosis of MBD should include aneurysmal bone cyst, traumatic bone cyst, benign tumors of the salivary gland, lipoma, salivary gland hypertrophy,17 non-ossifying fibroma, brown tumor of hyperparathyroidism, osteoporotic bone marrow defect, giant cell tumor, multiple myeloma, eosinophilic granuloma, and metastatic disease.315 Fatty tissue deposition, blood vessels, and soft tissue deposition should also be considered.17 However, unlike MBDs, parotid-region tumors usually present with symptoms such as swelling, paresthesia, and/or motor deficiencies.17 Exclusively in panoramic radiographs, a pseudoforamen referred to as a “medial sigmoid depression,” defined as a radiolucency also located in the mandibular ramus, can have similar features to an MBD.24
In conclusion, because MBDs are considered structural changes in the mandible2 and since patients are free of complaints,12 no treatment is required.4 Biopsy should be performed only in atypical cases when the diagnosis is inaccurate and clinical symptoms are present.4 In the present case, the symptoms were clearly from the TMJ and we observed glandular tissue in the defect by MRI, so a biopsy was not indicated. Notwithstanding, regular follow-ups are strongly recommended.225
Figures and Tables
Fig. 2
Four-part panoramic radiograph of the temporomandibular joint. Views of the temporomandibular joint with the mouth open and closed demonstrate the oval-shaped radiolucency in the left side of the mandibular ramus.

Fig. 3
An axial scout magnetic resonance image demonstrating a tiny hyperintense area in the left mandibular ramus, facing the lingual side (arrow number 1). Note the parotid glandular tissue (arrow number 2), which is also hyperintense. Arrow number 3 indicates the mandibular ramus.

References
1. Stafne EC. Bone cavities situated near the angle of the mandible. J Am Dent Assoc. 1942; 29:1969–1972.

2. Kaya M, Ugur KS, Dagli E, Kurtaran H, Gunduz M. Stafne bone cavity containing ectopic parotid gland. Braz J Otorhinolaryngol. (in press).

3. Quesada-Gómez C, Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. Stafne bone cavity: a retrospective study of 11 cases. Med Oral Patol Oral Cir Bucal. 2006; 11:E277–E280.
4. Taysi M, Ozden C, Cankaya B, Olgac V, Yıldırım S. Stafne bone defect in the anterior mandible. Dentomaxillofac Radiol. 2014; 43:20140075.

5. Minowa K, Inoue N, Sawamura T, Matsuda A, Totsuka Y, Nakamura M. Evaluation of static bone cavities with CT and MRI. Dentomaxillofac Radiol. 2003; 32:2–7.

6. Philipsen HP, Takata T, Reichart PA, Sato S, Suei Y. Lingual and buccal mandibular bone depressions: a review based on 583 cases from a world-wide literature survey, including 69 new cases from Japan. Dentomaxillofac Radiol. 2002; 31:281–290.

7. Lee JI, Kang SJ, Jeon SP, Sun H. Stafne Bone cavity of the mandible. Arch Craniofac Surg. 2016; 17:162–164.

8. Campos PS, Panella J, Crusoé-Rebello IM, Azevedo RA, Pena N, Cunha T. Mandibular ramus-related Stafne’s bone cavity. Dentomaxillofac Radiol. 2004; 33:63–66.

9. Hansson LG. Development of a lingual mandibular bone cavity in an 11-year-old boy. Oral Surg Oral Med Oral Pathol. 1980; 49:376–378.

10. Bornstein MM, Wiest R, Balsiger R, Reichart PA. Anterior Stafne’s bone cavity mimicking a periapical lesion of endodontic origin: report of two cases. J Endod. 2009; 35:1598–1602.

11. Sisman Y, Etöz OA, Mavili E, Sahman H, Tarim Ertas E. Anterior Stafne bone defect mimicking a residual cyst: a case report. Dentomaxillofac Radiol. 2010; 39:124–126.

12. Assaf AT, Solaty M, Zrnc TA, Fuhrmann AW, Scheuer H, Heiland M, et al. Prevalence of Stafne’s bone cavity - retrospective analysis of 14,005 panoramic views. In Vivo. 2014; 28:1159–1164.
13. Krafft T, Eggert J, Karl M. A Stafne bone defect in the anterior mandible - a diagnostic dilemma. Quintessence Int. 2010; 41:391–393.
14. Friedrich RE, Zustin J, Scheuer HA, Assaf AT, Gröbe A. An unilateral basal bone defect of the mandible occupied by fatty tissue: Stafne’s cavity. In Vivo. 2012; 26:1045–1048.
15. Etöz M, Etöz OA, Sahman H, Sekerci AE, Polat HB. An unusual case of multilocular Stafne bone cavity. Dentomaxillofac Radiol. 2012; 41:75–78.

16. Mauprivez C, Sahli Amor M, Khonsari RH. Magnetic resonance sialography of bilateral Stafne bone cavities. J Oral Maxillofac Surg. 2015; 73:934.e1–934.e7.

17. Chen CA, Ahn Y, Odell S, Mupparapu M, Graham DM. Developmental salivary gland depression in the ascending mandibular ramus: a cone-beam computed tomography study. Imaging Sci Dent. 2016; 46:223–227.

18. Sisman Y, Miloglu O, Sekerci AE, Yilmaz AB, Demirtas O, Tokmak TT. Radiographic evaluation on prevalence of Stafne bone defect: a study from two centres in Turkey. Dentomaxillofac Radiol. 2012; 41:152–158.

19. Wolf J. Bone defects in mandibular ramus resembling developmental bone cavity (Stafne). Proc Finn Dent Soc. 1985; 81:215–221.
20. Barker GR. A radiolucency of the ascending ramus of the mandible associated with invested parotid salivary gland material and analogous with a Stafne bone cavity. Br J Oral Maxillofac Surg. 1988; 26:81–84.

21. Shields ED. Technical note: Stafne static mandibular bone defect-further expression on the buccal aspect of the ramus. Am J Phys Anthropol. 2000; 111:425–427.

22. Kahn JL, Bourjat P, Barrière P. Ectopic parotid gland in the mandible and masseter muscle. Rev Stomatol Chir Maxillofac. 2002; 103:195–197.
23. Lee KH, Thiruchelvam JK, McDermott P. An unusual presentation of Stafne bone cyst. J Maxillofac Oral Surg. 2015; 14:841–844.

24. Langlais RP, Glass BJ, Bricker SL, Miles DA. Medial sigmoid depression: a panoramic pseudoforamen in the upper ramus. Oral Surg Oral Med Oral Pathol. 1983; 55:635–638.

25. Deyhimi P, Darisavi S, Khalesi S. Stafne bone cavity with ectopic salivary gland tissue in the anterior of mandible. Dent Res J (Isfahan). 2016; 13:454–457.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download