Introduction
Apical periodontitis (AP) is a frequently observed consequence of intracanal infections, and is usually detected and monitored with the aid of digital or conventional periapical radiographs along with clinical tests.
1 The precise diagnosis of AP is critical in order to allow clinicians to select the proper therapeutic approach.
2
Digital periapical radiography (DPR) has been preferred by clinicians and researchers due to well-documented advantages when compared with conventional periapical radiography; mainly, the fact that it does not require processing.
3 In addition, DPR is considered significantly more accurate and sensitive in detecting AP than conventional periapical radiography.
45
However, in many cases, bone lesions associated with AP can be present, but undetectable in periapical radiographs.
6 According to a study in which apical lesions were artificially created in human jaws, conventional periapical radiographs were successful in the detection of apical lesions, with higher accuracy when the cortical bone was involved.
7 In fact, at present, researchers agree that periapical radiographs have a limited ability to diagnose AP, and that they should not be used for scientific investigations because of the low sensitivity and accuracy of the method.
89
A cadaveric study observed that roots that seemed healthy on conventional periapical radiographs in reality showed histological evidence of inflammation,
10 while a comparison among conventional periapical radiographs, histological evaluations, and cone-beam computed tomography (CBCT) showed that periapical radiographs failed to detect AP in 22% of the cases, while CBCT failed in only 9% of the cases.
11 According to a position statement published by the American Association of Endodontists together with the American Academy of Oral and Maxillofacial Radiology, CBCT should be considered an adjunct to 2-dimensional imaging in dentistry, especially in complex cases.
12
Recent findings showed that CBCT outperformed conventional periapical radiographs in the detection of artificially created apical bone lesions.
13 Similar results were found in animal models
8 and clinical studies.
29 Additionally, CBCT has exerted a substantial impact on diagnostic thinking in endodontics, since 41% of the diagnoses previously based on periapical radiographs were found to have changed after CBCT evaluation.
14
Although CBCT is an important tool used for diagnostic purposes as well as for surgical planning, most dentists lack the proper training needed to adequately evaluate the images obtained with CBCT. Moreover, the proper indications for CBCT and the diagnostic/planning resources provided by the visualization software are unknown by many professionals, which limits the accuracy of CBCT examinations and deprives patients of the benefits of CBCT.
15
Thus, the present study aimed to compare the diagnostic accuracy of previously trained endodontists in the detection of artificially created periapical lesions, using CBCT and DPR in an ex vivo model with dry skulls.
Go to :

Materials and Methods
Selection of the anatomical pieces
Two well-preserved dry skulls obtained from the Department of Anatomy were selected to be used in the study. The anatomical specimens had at least 20 teeth. After a visual inspection, the skulls were scanned with a CBCT machine (Kodak 9500 3D System, Carestream Health, Rochester, NY, USA) in order to identify teeth presenting signs of previous endodontic treatment, caries, deep fillings, fracture, AP, or a close relationship with the sinus, nasal cavity, or mandibular canal.
After the first CBCT screening, teeth presenting any of the previously described conditions were excluded from the study. The remaining teeth considered for inclusion in the study were carefully extracted using periotomes and forceps. After extraction, the alveoli were visually inspected with the aid of magnifying lenses to confirm the integrity of the cortical bone (alveolar bone proper). In this stage, teeth that presented root or bone plate fracture during extraction and those in which the inner cortical bone was not 100% complete were excluded from the study.
After extraction and visual inspection, teeth were carefully repositioned in the alveolar process and a new CBCT scan was taken to confirm that the teeth were completely adapted to the alveoli. Teeth that could not be properly repositioned and showed a radiolucent gap between the apex and the cortical bone were also excluded from the study.
Of a total of 40 teeth that were initially scanned, 11 were included in the experimental stage of the study. The final sample consisted of 6 maxillary teeth (3 incisors, 1 first premolar, 1 second premolar, and 1 first molar) and 5 mandibular teeth (1 incisor, 1 canine, 1 premolar, and 2 molars).
Baseline imaging evaluation
After the teeth suitable for inclusion in the study were selected, the experimental phase started with the acquisition of baseline images. A digital periapical radiograph and CBCT scan of each tooth were taken before artificially creating the periapical lesions according to the protocols described below.
Digital periapical radiographs
Digital periapical radiographs were obtained using the Express™ imaging plate system (Instrumentarium Dental, Tuusula, Finland) and a digital X-ray equipment with 70 kVp and 8 mA (XDent X70, XDent Dental Equipment, Ribeirão Preto, São Paulo, Brazil). Digital periapical radiographs were taken using the paralleling technique with the aid of a positioning tool designed to hold the digital sensor (XPC instruments RINN®, RINN Corporation, Elgin, Illinois, USA).
To allow the reproducibility of the sensor position and also the parallel incidence of X-rays, stabilization guides were manufactured using impression material (Zetaplus™, Zhermack SpA, Badia Polesine, Rome, Italy).
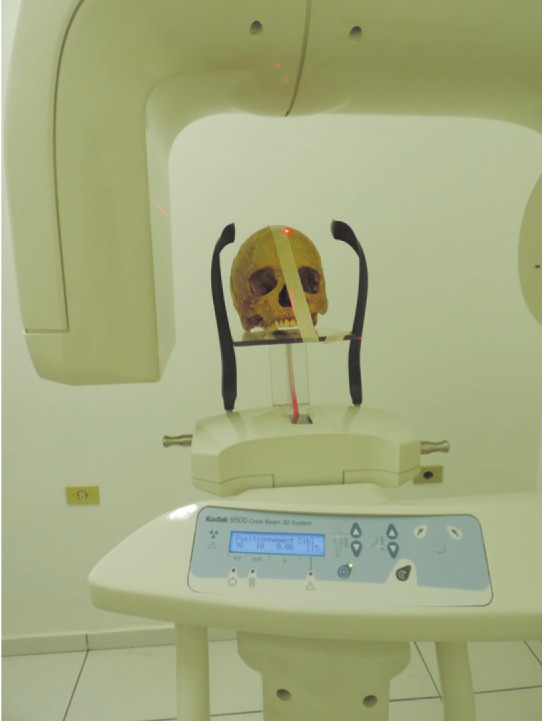
Figure 1 shows the stabilization guides, positioning tools, X-ray cylinder, and the skull in position, ready to have the image captured.
 | Fig. 1Stabilization guides, positioning tools, X-ray cylinder, and the skull in position for capturing the image.
|
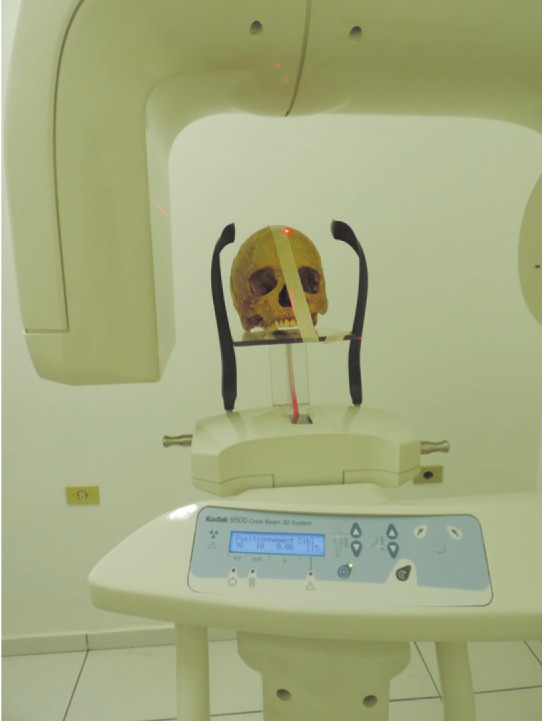
Cone-beam computed tomography
CBCT scans were taken using the following settings: 90 kVp, 10 mA, and a scanning time of 24 seconds. A large FOV (18.4 cm×20.6 cm) was selected with a voxel size of 0.3 mm, because a smaller FOV with smaller voxels would not allow a complete image of the skull and mandible to be obtained simultaneously. An acrylic platform properly designed to hold the anatomical specimen was used to stabilize the skulls and mandibles during scanning (
Fig. 2).
 | Fig. 2Acrylic device designed to position the anatomical pieces during cone-beam computed tomography scanning.
|
Artificially created bone defects
Spherical carbide burs (KG Sorensen, São Paulo, SP, Brazil) were used with a low-speed handpiece to create artificial bone defects, simulating AP at the most apical area of each socket. The diameter of the tip of the burs was gradually increased, starting with a #1/2 bur (0.6 mm), followed by #2 (1.0 mm), #4 (1.4 mm), and #6 (1.8 mm) burs. The defects were drilled until the tip of the bur completely passed through the lamina dura. To ensure that the tip of the burs did not go beyond the predetermined working length (alveolus length plus the diameter of the tip), the alveoli were measured with the aid of periodontal probes and a drilling template was used for each alveolus. These bone defects were categorized as 0 (no defect), 1 (0.6 mm), 2 (1.0 mm), 3 (1.4 mm), and 4 (1.8 mm).
After each artificial defect was simulated, the tooth was repositioned, and CBCT and DPR were repeated according to the previously described protocol. This sequence was followed until all the burs were used in each alveolus, and each artificially created bone defect measured approximately 1.8 mm in diameter.
Image analysis
The whole set of images acquired from CBCT scans and DPR was evaluated by an experienced radiologist and considered suitable for inclusion in the study. Digital periapical radiographs were viewed using Cliniview (Instrumentarium Dental, Tuusula, Finland) and CBCT scans were viewed with CS 3D imaging software (Carestream Health, Rochester, NY, USA).
The CBCT images for each tooth were selected by a team formed by an experienced board-certified endodontist and an experienced board-certified radiologist with expertise in CBCT. Only 1 parasagittal image was selected for each tooth. The image selected was the one that allowed the clearest visualization of the periapical region according to both examiners. In cases when there was a disagreement between examiners, a third examiner (an experienced implantologist/periodontist) was consulted and the issue was discussed until all parties agreed.
After the images were selected, a Powerpoint® (Microsoft, Redmond, WA, USA) presentation was prepared with a total of 110 images, each randomly allocated to a single slide. Ten previously contacted board-certified endodontists who had agreed to participate in the study analyzed the presentation and, after analyzing each slide, responded in a form if they considered each tooth to have a periapical lesion or not. The form allowed only 1 answer for each slide, and the participants selected among 3 possible answers: definitely present, definitely absent, or not sure (
Fig. 3). Each examiner was trained in endodontics in a different university, and at the time of the study, all of them were enrolled in master's or PhD postgraduate programs at Estácio de Sá University (Rio de Janeiro, Brazil).
 | Fig. 3Example of a template with cone-beam computed tomography and digital periapical images evaluated by the examiners.
|
The images were presented to the examiners using the full screen presentation format on a desktop monitor (15 inches) in a dark room, and participants were asked to select and click the answer they considered to be correct according to the following guidelines: 1) The tooth presented in each slide must be evaluated for the presence of a periapical lesion. For each slide, you must select only 1 answer: definitely present, definitely absent, or not sure. 2) In the slides showing periapical radiographs, the tooth to be analyzed is the one shown in red, while in the slides showing a tomographic image, only the tooth to be analyzed is shown. 3) You should preferably select the answer directly in the slide and send us back the file after you complete the analysis. 4) You can take as long as you need to evaluate each image, and we ask that after you select your answer you do not return to the same slide again. 5) Slides and images must not be digitally altered.
Statistical analysis
The accuracy of each of the diagnostic methods was evaluated. Comparison between DPR and CBCT was performed using the chi-square test. All statistical tests were performed using SPSS version 19.0 (IBM Corp., Armonk, NY, USA). The level of significance was set at 5%.
Go to :

Results
After scanning 6 anatomical specimens (3 mandibles and 3 maxillae), 11 teeth satisfied the inclusion criteria and were included in the study: 6 from the maxilla (1 central incisor, 2 lateral incisors, 1 first premolar, 1 second premolar, and 1 second molar) and 5 from the mandible (1 lateral incisor, 1 canine, 1 second premolar, and 2 second molars).
110 images were obtained (DPR, 55; CBCT, 55). Six examiners returned the presentation form fully and adequately answered. Thus, a total of 660 answers were included in the analysis, with a total of 60 answers per tooth.
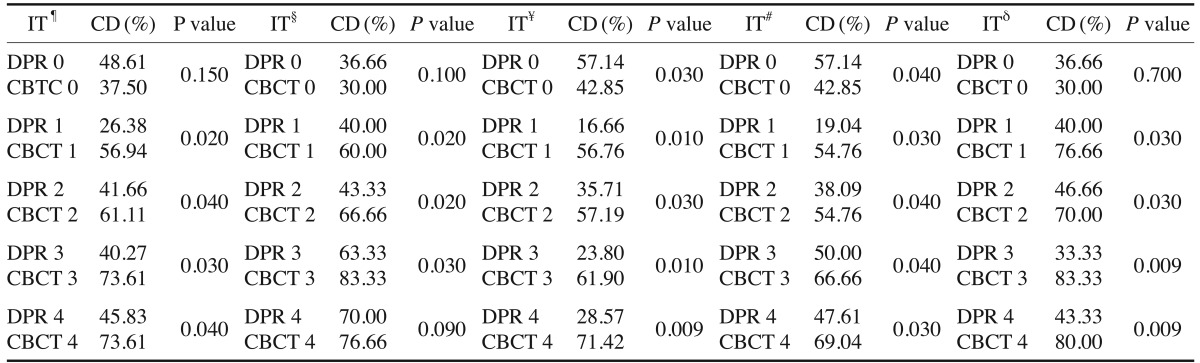
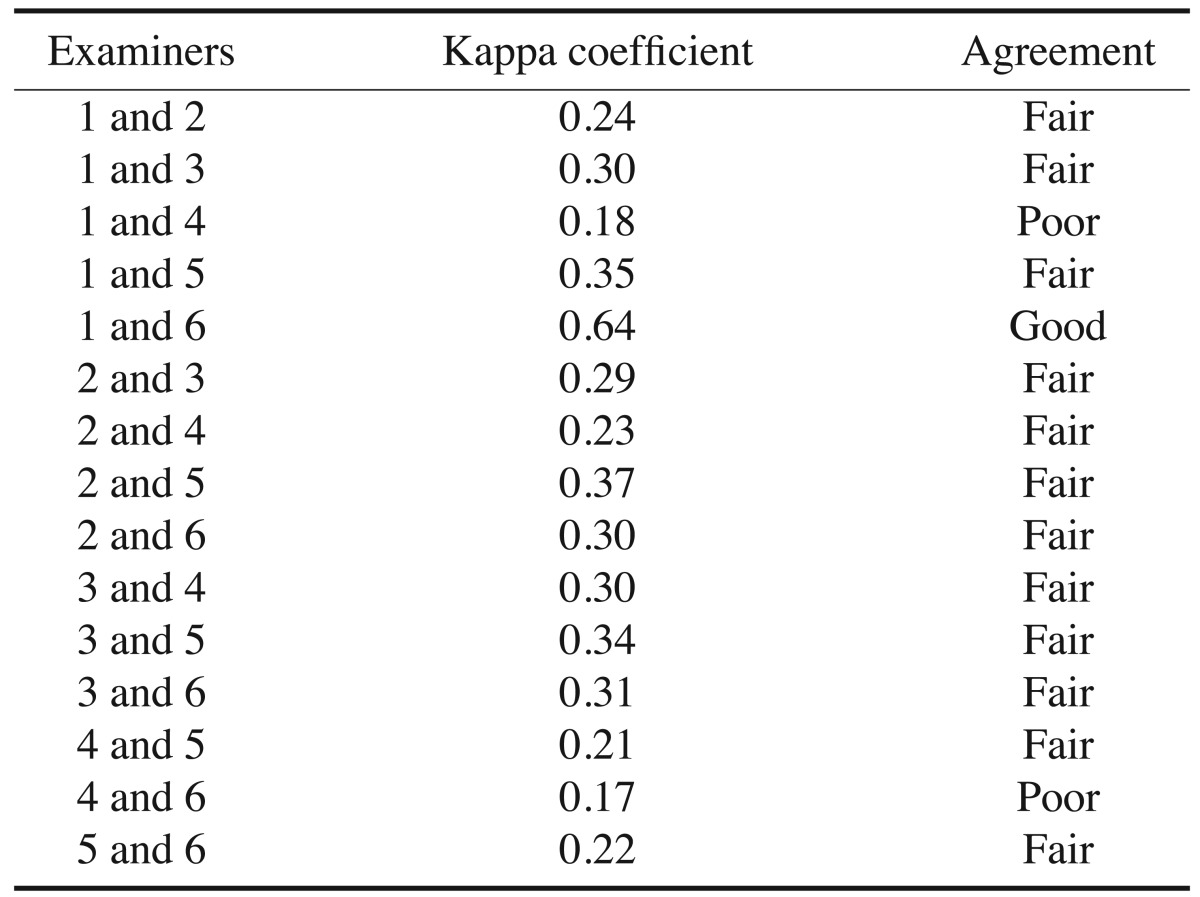
The analysis of the kappa coefficient showed fair concordance among the participants (range, 0.17-0.64) (
Table 1). CBCT was almost twice as sensitive as DPR (0.829 vs. 0.434,
P=.019).
Table 1
Kappa coefficients between examiners
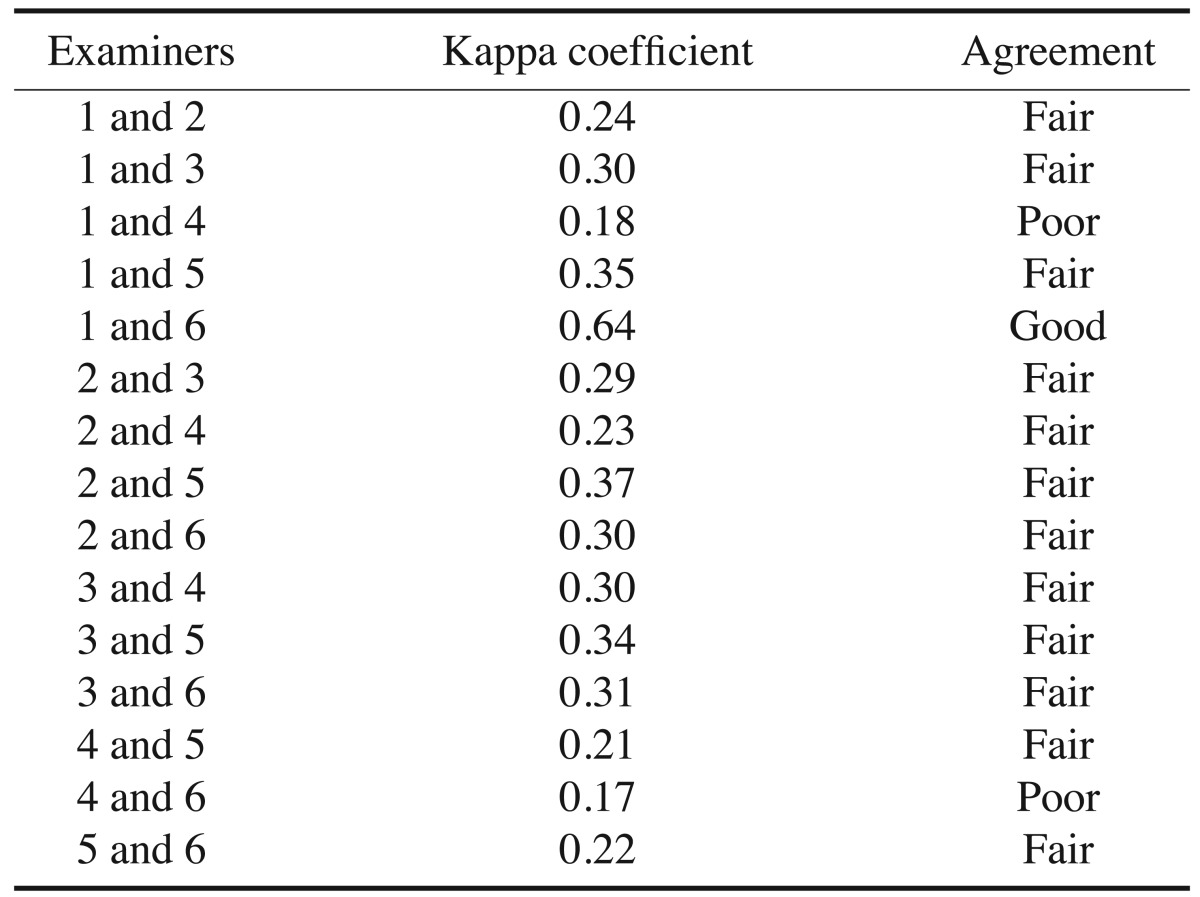

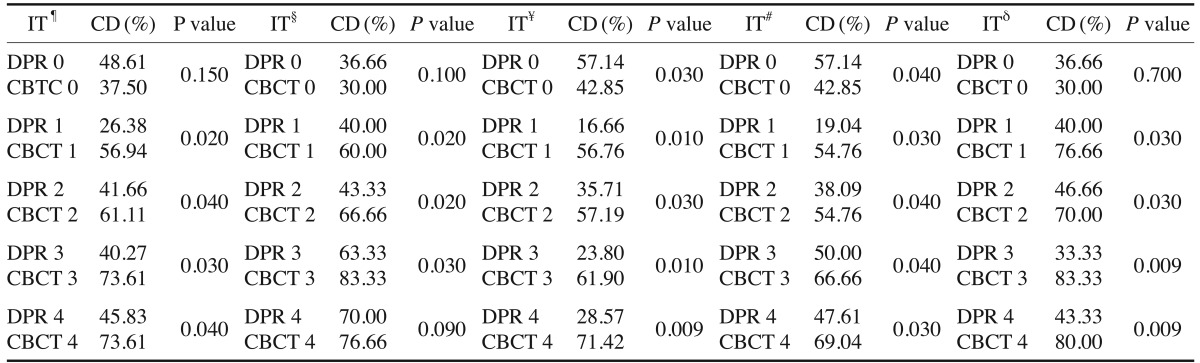
Table 2 shows a comparison between the percentage of correct answers for each method tested with different groups of teeth. No significant difference was found between methods regarding the negative controls (teeth without periapical lesions) (
P=.15). However, CBCT showed better results in the detection of artificially created periapical lesions, regardless of the size of the lesions (
P<.05).
Table 2
Comparisons between the imaging techniques

The percentage of correct diagnoses (true positives) was higher for larger lesions in both methods. No difference was found in the percentage of correct diagnoses when CBCT was used to detect larger lesions (1.4-1.8 mm in diameter). In both cases, the percentage of correct diagnoses was 73.61%. Digital periapical radiographs had a higher percentage of correct diagnoses when no lesion was present. In other words, CBCT produced more false positives than DPR, but this difference was not statistically significant. However, DPR had a low percentage of correct diagnoses (<50%), even for the largest lesions (1.8 mm in diameter).
The diagnostic accuracy of both methods in the detection of artificially created periapical lesions in the mandible is also shown in
Table 2. Although there was no significant difference between techniques for the teeth without a periapical lesion (
P=.10), CBCT had significantly better results for the smaller lesions (
P<.05), whereas no significant difference between methods was found for the lesions measuring 1.8 mm in the mandible (
P=.09).
The analysis of the images from the maxilla yielded results significantly favoring CBCT, with 2.5 times more correct diagnoses than were obtained using DPR (P<.05). Even in the largest lesions with a diameter of 1.8 mm, the percentage of correct answers was 29% for DPR against 71% for CBCT (P<.01).
Table 2 also shows a comparison between methods for single-rooted teeth. In this case, DPR was more accurate for detecting the absence of periapical lesions (
P=.04). CBCT showed more false-positive results, but was almost twice as precise in the detection of lesions in multi-rooted teeth (
P<.05). No difference was found between the methods when analyzing multi-rooted negative controls (
P=.70).
Go to :

Discussion
DPR and CBCT were used to detect periapical lesions artificially created in an ex vivo model using anatomical specimens. DPR was used because periapical radiography is the imaging technique most commonly used in endodontics. However, digital systems are preferred since they eliminate possible errors arising from processing techniques,
16 hence being possibly more accurate than conventional periapical radiographs.
5 CBCT was compared to DPR due to the well-documented advantages of the technique, most notably lower radiation and a smaller field of vision that provides clearer images.
3
The kappa coefficient yielded low agreement among examiners, especially when DPR was analyzed. This might be partially explained by the fact that lesions limited within the cancellous bone are harder to visualize on periapical X-rays.
7 The highest agreement level was found between examiners 1 and 6 (kappa=0.64), who, coincidentally, had the highest percentage of correct answers. The percentage of agreement between examiners was even lower when only CBCT was analyzed. Our hypothesis to explain this result was that probably even experienced board-certified endodontists might not be familiar with CBCT and might have difficulties interpreting the exams. In order to minimize the effects of this possible unfamiliarity of the examiners with the technique, the images sent for evaluation were selected by an experienced radiologist together with a board-certified endodontist and showed the clearest image obtained for each tooth. The images were selected to represent, as closely as possible, the kind of image that would be sent to a dentist if a CBCT scan was requested from a radiology clinic with the purpose of detecting periapical lesions in a real patient.
In images with artificially created periapical lesions, the image selected and sent to the examiners was the one that both the radiologist and endodontist agreed was the clearest in showing the lack of continuity of the lamina dura. Examiners did not receive the CBCT visualization software to make sure they would not be able to analyze different areas, thereby leading to non-standardized images.
It has been well documented that a periapical lesion may be present but invisible to X-rays. However, 3-dimensional images obtained with CBCT are able to overcome this limitation of 2-dimensional imaging techniques, representing a significant advance in terms of diagnostic tools in endodontics.
6 This was in accordance with our findings that CBCT had a higher sensitivity than DPR. CBCT was almost twice as sensitive as DPR (0.829 vs. 0.434). In other words, CBCT was twice as capable of detecting periapical lesions when these lesions were truly present than was DPR.
Another finding from our study was, as expected, that larger lesions were associated with higher percentages of correct diagnoses for both techniques. In this regard, our findings were in agreement with those described by Tsai et al.,
13 who observed that even CBCT scans were not highly reliable in detecting defects smaller than 0.8 mm.
Both techniques were equally accurate and showed similar results in detecting the absence of periapical lesions. However, in general, CBCT was significantly better than DPR in detecting the presence of periapical lesions, regardless of the size of the defects. Similar findings have previously been described in the literature and reinforce the importance of CBCT in the early detection of primary and secondary apical lesions.
91317
When only the larger-diameter lesions (1.4 mm and 1.8 mm) were analyzed in the CBCT scans, no significant difference was found regarding the correct detection of artificially created lesions. These results are in accordance with the data published by Tsai et al.,
13 who affirmed that the accuracy of CBCT for the detection of lesions ≥1.4 mm was excellent. However, an interesting finding regarding CBCT was the fact that this technique showed a higher number of false positives, although this tendency was not statistically significant. One possible explanation for this finding might be the fact that the endodontists taking part in the study were not necessarily familiar with CBCT, despite using the technique in their daily practice. Difficulties in interpreting CBCT might be due to a learning curve. In fact, although it is a very useful tool, CBCT is still underutilized as part of the daily routine of many endodontists.
3
When only lesions in the mandible were studied, CBCT was significantly better than DPR in the detection of lesions created with smaller burs (0.6 mm, 1.0 mm, and 1.4 mm). No significant difference was observed for lesions 1.8 mm in diameter. These results are supported by data from previously published studies suggesting that in compact/cortical bone, defects can only be detected by X-ray after the complete resorption of the cortical bone.
1117 In contrast, in the maxilla, CBCT was 2.5 times more accurate than DPR, even for 1.8-mm lesions. The anatomical properties of more cancellous bone are probably the reason why DPR failed to detect small lesions.
913
Another clear advantage of CBCT was noted in multirooted teeth. The 3-dimensional image allows the evaluation of each root separately and eliminates the possible diagnostic limitations of superimposed images. In fact, our findings suggest that when it comes to the evaluation of periapical lesions, multi-rooted teeth in the maxilla seem to benefit the most from CBCT in endodontics.
A recently published systematic review and meta-analysis of the diagnostic accuracy of CBCT and both conventional radiography and DPR reported that periapical radiographs (conventional and digital) showed good diagnostic accuracy regarding the discrimination of artificially created periapical lesions from the absence of lesions, whereas CBCT imaging showed excellent accuracy.
18 These findings are in accordance with those of the present study and also with data from Kanagasingam et al.,
19 who, using histopathological findings as a reference standard, concluded that CBCT had significantly higher diagnostic accuracy.
To the best of our knowledge, our study was the first to compare these different imaging techniques for the detection of periapical lesions in the maxilla. Previously published data only referred to defects in the mandible.
11141820 One possible explanation for the absence of experimental studies in the maxilla may be the difficulty of obtaining teeth that could be extracted while maintaining the inner cortical bone of the alveolar process (lamina dura). Anatomical features, especially the proximity of the roots of molars with the maxillary sinus, are also a limitation in these models. However, since the advantages of CBCT seem to be more noticeable in multi-rooted maxillary teeth with incipient periapical lesions, it is of greater relevance that researchers conduct ex vivo and in vivo studies aiming to evaluate CBCT and other diagnostic tools in the maxilla.
Within the limitations of the present study, we were able to conclude that CBCT was more reliable than DPR in the detection of periapical lesions artificially created in the mandible and maxilla in an ex vivo model independently of the size of the lesion. This advantage was more evident in the maxilla, especially in multi-rooted teeth.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download