Abstract
Purpose
This study was performed to quantify the repeat rate of imaging acquisitions based on different clinical examinations, and to assess the prevalence of error types in intraoral bitewing and periapical imaging using a digital complementary metal-oxide-semiconductor (CMOS) intraoral sensor.
Materials and Methods
A total of 8,030 intraoral images were retrospectively collected from 3 groups of undergraduate clinical dental students. The type of examination, stage of the procedure, and reasons for repetition were analysed and recorded. The repeat rate was calculated as the total number of repeated images divided by the total number of examinations. The weighted Cohen's kappa for inter- and intra-observer agreement was used after calibration and prior to image analysis.
Results
The overall repeat rate on intraoral periapical images was 34.4%. A total of 1,978 repeated periapical images were from endodontic assessment, which included working length estimation (WLE), trial gutta-percha (tGP), obturation, and removal of gutta-percha (rGP). In the endodontic imaging, the highest repeat rate was from WLE (51.9%) followed by tGP (48.5%), obturation (42.2%), and rGP (35.6%). In bitewing images, the repeat rate was 15.1% and poor angulation was identified as the most common cause of error. A substantial level of intra- and interobserver agreement was achieved.
Conclusion
The repeat rates in this study were relatively high, especially for certain clinical procedures, warranting training in optimization techniques and radiation protection. Repeat analysis should be performed from time to time to enhance quality assurance and hence deliver high-quality health services to patients.
Rejects, deletions, and the subsequent repeat taking of diagnostic X-ray images impose professional and ethical challenges within radiological imaging. Such activities take up additional, often unnecessary, processing and personnel resources,1234 waste medical resources for quality assurance of the institution,45 and indicate suboptimal quality management.678 Hence, decreasing the taking of repeat images is crucial to reduce patients' X-ray exposure and inconvenience.9
Repeat image analysis is one of the major quality improvement tools used in imaging departments, which is still carried out despite advances in technology.7 The repeat rate is frequently used as the indicator for repeat analysis, and is calculated as the ratio of the number of repeat images to the total number of images taken.10 It is usually up to the practitioners performing the examinations to decide which images to repeat.10 Repeat analysis involves the calculation of the number of repeat images and thus can only be conducted after the number of repeat images is confirmed.
In traditional film-based systems, the reject/deletion/repeat rate was reported to be within the range of 10–15%.1211 Following digitization of radiography, the reject/deletion/repeat rate of X-ray images can be expected to be reduced since the latitude of a direct sensor is usually wider than an X-ray film. A series of studies has found that the reject/deletion/repeat rate in digital systems is around 5%.56781213 However, some studies on digital radiography have still exhibited some degree of reject/deletion/repeat, with the rate ranging between 8% and 12%.359 A more recent study unveiled a significant reduction of the repeat rate from 4.89% to 3.57% 6 months after a list of guidelines was introduced.14
The use of digital sensors, such as complementary metal-oxide-semiconductors (CMOSs) or charge-coupled devices (CCDs), can substantially help in reducing the radiation dose absorbed by patients.15 Although the indirect type of digital sensor, such as the photostimulable phosphor (PSP), is an alternative in digital systems, it does not outperform CMOSs and CCDs in terms of percentage of correct assessment due to contrast and spatial resolution,1617 reliable images for root canal working length estimation,18 and its performance when coupled with automatic exposure compensation.19 However, PSPs are preferable in academic institutions, where the monitoring of image repetition is more vigorous compared to CMOS and CCD types.
Consistent analysis of the retaken images would aid in finding the factors causing the repeat taking, which would be useful for designing guidelines to reduce the repeat rate.14 In film-based radiography, the reason for repeat images often relates to an incorrect exposure due to the limited dynamic range of the screen/film systems;4 however, in digital systems, the most frequently observed factors are related to the lack of operator skills, particularly with regard to patient positioning and proper equipment operation.3469 In certain circumstances, the repeat rate can be difficult to control, such as in relation to patient variability, equipment quality, and workplace culture.4 Repeat radiographs are responsible for the majority of ‘unnecessary’ patient irradiation dosing, and repeating films for ‘avoidable reasons’ should therefore be minimized in order to encourage good radiographic practice.2021 This study was performed to quantify the repeat rate of imaging acquisitions based on different clinical examinations, and to assess the prevalence of error types in intraoral bitewing and periapical imaging using the digital CMOS intraoral sensor.
This current work was a retrospective cross-sectional case study collecting and assessing intraoral radiographic images from records archived within the Diagnostic Imaging Unit, Faculty of Dentistry, Universiti Teknologi MARA (UiTM) over a 6-month period from January 2016 until June 2016. All students had completed 49 (25 lecture and 24 practical session) hours of face-to-face comprehensive didactic module series on Oral and Maxillofacial Radiology. This involved topics ranging from radiation physics and protection to the techniques and interpretation of diagnostic images taught before and during the clinical years. Ethics approval was obtained from UiTM Research Ethics Committee under reference number 600-IRMI (5/1/6).
The CMOS sensor (EzSensor, pixel size 35 µm, Vatech, Hwaseong, Korea) coupled to an intraoral machine (Satelec X-Mind AC/DC, Satelec ACTEON Tuusula, Finland) was used in this study. All digital radiographic examinations were automatically registered by the system. The acquisition was performed by the undergraduate clinical dental students. Only images acquired by the undergraduate clinical dental students were included in the sampling. The system prohibited image deletion and did not allow for any image manipulation except for modification of contrasts.
The images were collected and evaluated on EasyDent V4© viewer software version 4.1.4.5 (Vatech, Hwaseong, Korea) (Fig. 1). All periapical and bitewing images performed between January and June 2016 were retrieved from radiology workstations. The total numbers of repeat and non-repeat images were each summed. Repeat images were segregated from non-repeats by distinguishing repetition patterns that did not contribute to the diagnostic information nor to correcting faulty images. The total number of repeat images represented the numerator while the summation of the total images taken was used as the denominator to calculate the repeat rate. Multiple entry images were excluded for assessment in this study.
Prior the data collection, 2 raters were calibrated by an endodontist and dental pediatric specialist for image category and repetition decision. Thirty images were selected and projected from a computer to a 42-inch television screen in a room with fixed ambient lights. Both specialists and raters performed the calibration in the same setting but on separate occasions; 2 times separated by a 3-week interval. The inter- and intra-rater reliability were then determined.
The periapical and bitewing images were further clustered based on endodontic and caries/periodontal diagnoses, respectively. In the endodontic images, the percentage of repeated images was measured according to the stages of every procedure: working length estimation (WLE), trial gutta-percha (tGP), obturation, and removal of gutta-percha (rGP). In general, the reasons for repetition were determined prior to data collection as operator, technical/machine, and patient error. Improper angulation and evidence of removable artifacts were categorized as operator errors. Technical/machine errors were characterized by image blurring and the presence of artifacts that could not be explained by either operator or patient error. Should patients move during the radiographic acquisition, the resulting errors would be considered patient errors. This assessment was made with the understanding that the patients had been properly advised on pre-operative procedures by the operator prior to acquisition. In addition, the current study excluded radiographic images obtained from special needs patients, that is, those who presented any type of disability—physical, sensory-motor, or mental, as well as those who were medically compromised. These exclusions eliminated bias due to patient error, specifically from the inability part of the patient to properly bite on the bite block of the radiographic holder device. Any repetitions detected with no specific reasons were classified as unknown, for instance, in the case when the first obtained image was diagnostically acceptable or correct but the operator still repeated the radiographic acquisition.
The data and the implied reasons for the image repeats were recorded using Microsoft Excel 2010. The repeat rates were calculated using the following formula: Number of repeat images / Total number of images taken x 100%
The repeat rate for each reason for repetition was obtained by dividing the number of repeated images due to a given reason by the total number of images acquired. Both intra- and inter-rater reliability tests were performed by 2 dental students who had been calibrated to intraoral image examination and diagnosis. Prior to data collection and analysis, the examiners were calibrated with a field expert on the categories of repeat evidence of an image. A weighted Cohen’s kappa coefficient was used to measure the inter-rater agreement. Should the 2 raters not agree, the third rater was to be involved in the final consensus. Data were statistically analyzed using the χ2 test with Yates’s continuity correction to determine differences between 2 groups (Years 3 and 4). Year 5 was not compared due to its substantial difference with regard to module content. Significance was attributed to P values less than .05. The weighted Cohen’s kappa was calculated using R Studio version 1.0.136 (R Studio Inc. Boston MA, USA).
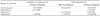
During the 6-month period, a total of 8,030 digital radiographic images were taken (Table 1). This included 5,746 periapical and 2,284 bitewing radiographs. There were 30 error images assumed to be due to multiple entry of the same image.
The overall repeat rate focusing on procedures involving intraoral periapical images was about 54.4%. Within this, WLE caused the highest repeat rate, which was 51.9%, followed by tGP (48.5%) and obturation (42.2%). The procedure of rGP had the lowest repeat rate of 35.6% (Fig. 2). In the bitewing images, the repeat rate was 15.1%. Operator error was the main cause of radiographic images taken repeatedly by students, accounting for about 56.7% of all errors. Upon closer scrutiny, positioning and angulation were identified as the most common reasons for repetition due to operator error. Among the origins of errors, technical/machine errors were least common, at only 1.5%.
The percentage repeat rate of images by students' year in school (Fig. 2) revealed that the highest repeat rate (28.2%) was attributed to year 3 clinical students, followed by 20.7% for year 5 and 12.9% for year 4. The difference between year 3 and year 4 was statistically significant (P<.05). Year 3 clinical students had the highest repeat rate and year 4 students the lowest.
Thirty images were used to test the inter-rater agreement between 2 raters in determining the number of images repeated and type of X-ray images taken. Using a weighted Cohen's kappa coefficient, the level of agreement was almost perfect, with the κ value ranging from 0.89 to 0.98. Calibration done with field experts also revealed an almost perfect level of agreement with a κ value of 0.98, except in determining the number of images repeated, which exhibited a moderate level of agreement with a κ value of 0.54. These reliability values were derived from CMOS produced images.
There is an extensive literature reporting on repeat/reject analysis in medical imaging performed by trained radiographers and/or radiologists, in which the repeat rate has typically ranged between 5% and 12%.3567913 However in our study, the focus group was undergraduate students still undergoing their training, with a particular focus on dental imaging. Therefore, the high rate of repeats, such as 51.9% in working length estimation during endodontic procedures, warrants careful scrutiny and interpretation. This high incidence of repeats could be due to a lack of radiation protection knowledge as well as limited technical skills among the undergraduates at this early stage of their training. Although these observations are commonly identified as a cause of concern amongst undergraduate students, these issues may be remedied by exposure to the necessary knowledge and experience throughout the progress of clinical practice. Furthermore, radiographic working length estimation required a special technique to visualize at least 2 parallel roots using the horizontal tube shift technique, commonly referred to as Clark's technique.22 This technique employed the principle of parallax using the same-lingual opposite-buccal (SLOB) rule to delineate the spatial relationships of an object. In our study, we found that the repeat rate was reduced with an increase in experience of the personnel taking the intraoral radiographs. This was evident where within a stint of one year, there was an improved repeat rate (from year 3 to 4). The clinical requirements for year 4 were similar to its predecessor, where the only difference was an increased number of cases. The highest repeat rate (28.2%) was seen with third-year clinical students, followed by fifth-year (20.7%) and fourth-year (12.9%) students. The slight increment of value in year 5 was likely due to the introduction of a molar endodontic module in the course taken. This was also a reason why we did not statistically compare the fifth-year student group to the other groups.
The repeat rate with the use of CMOS sensors is thought to be primarily caused by insufficient knowledge of radiation protection among the supervisors from different specialties. Although the exposure from dental X-rays is considered negligible in terms of risk, it is not best practice to allow multiple radiographic examinations to be performed on the same person. This is in line with the ALARA (as low as reasonably achievable) concept for producing diagnostic images with minimal radiation exposure. According to the linear-no-threshold model, even the smallest radiation dose may initiate carcinogenesis.2324 Further exploration is recommended to survey the knowledge and attitudes of local dental practitioners towards quality care in radiography and radiation protection.
This analysis has provided the department with valuable insights into why the students encounter difficulty when performing radiography for certain examinations. As described in other studies,1125 the repeat rate is specific to the examination type. From our study, it was notable that the students may have retaken a considerable number of X-rays without adequate justification. Upon unofficial interviews with some students, it was revealed that the students likely had problems in performing digital radiography in terms of choosing the right holder device, or deciding whether to use the holder or not and/or difficulty in properly placing the sensor inside the patient’s mouth.
Positioning errors have been recognized as the main reason for the taking of repeats in both endodontic examination and caries diagnosis (Table 2). Published studies of the reject/retake/repeat process in medical digital imaging reported this particular type of error as the main reason.369142627 For instance, in caries diagnosis, students appeared to encounter difficulties in positioning the sensor for both periapical and bitewing examinations. Various established studies have stated that the rejection rate is known to depend on the patient selection, the type of examination performed, the equipment used, how the rejects are registered, and the skills of the person performing the radiography.467121328 In our study, positioning errors were the main reason for the repetition during endodontic examinations and taking bitewings. This outcome was largely anticipated since students often have trouble using the specialized radiographic techniques in endodontic procedures, such as the use of the EndoRay® holder while taking an X-ray. Furthermore, this study hints that the students lacked a full appreciation and understanding of oral cavity morphology needed to be able to place the digital sensor properly. This finding suggests highlighting oral anatomy and the hands-on practical components of X-ray taking in the dental school teaching syllabus. With digital radiography, errors such as scratches on films, whether poorly developed or fixed, were completely eliminated.7
In certain circumstances, factors due to patients might be the main cause of repetition, such as a patient with a shallow floor of the mouth, a low palatal vault, severe gag reflex, or young age. In this study, the students exhibited the highest repeat rate when taking bitewings. This may be due to the stiffness and solid state of the CMOS sensor and the limited number of sizes available to provide sufficient choice of sensor based on the patient's oral condition. In a study of bitewing examinations comparing sensors and films, 76% of patients reported that the sensor was more unpleasant than the film, while 15% reported that they were similar.29 In a questionnaire study, pediatric dentists reported that the sensors were less accepted by young children compared to a phosphor plate.30
Repeat/rejects are not eliminated with the introduction of digital radiography, but their causes change significantly.4 For instance, to obtain the conventional film in most dental schools, students need to request it from the clinical supervisor and its issuance is recorded. Digital radiography, on the other hand, is within the operator's scope of control and, therefore, subject to their own personal judgment. Repeat X-rays have been perceived as reckless behavior that lead to unnecessary radiation dosage for patients and operators. One study has reported that with advances in digital radiography technology, students need to be cautious not to develop a complacent attitude or become overconfident.7
Reject/repeat analysis has been an important quality indicator for many years in assessing good practice in radiology.4671213252728 It is well accepted as an important tool in localizing the areas where optimization is required, and can be used as a basis for training and education.3 Nevertheless, these quantitative analyses provide no information on the diagnostic quality of the rejected images. In conclusion, after analyzing the repeat image rate, deficiencies in the X-ray taking skills of students were identified as the main factor causing the high repeat rate. Students mostly exhibited difficulties in performing periapical radiographs specifically for the parallax technique. Positioning errors (including the patient, films, and cone-beam angulation) accounted for 22.6% of all repetitions. These results offer great insights for management, training, education, and quality improvement. Possible solutions for reducing the taking of repeat images are to provide training courses for the less experienced with an aim to increase their professional knowledge and communication skills, as well as to better analyze the operation workflow.3132 Future studies should propose protocol guidelines in the radiology unit for reducing the image retake rate.
We have observed many direct benefits of implementing digital radiography in our institution, such as a reduction in film cost, which provides economic benefits and an improved workflow, as well as improved working time management within the students' clinical performance and patient management. In addition, the capability for more rapid retrieval of X-ray images has improved communication between the students and lecturers. This finding is supported by focus group studies of dental students, where it was determined that they saved more time when using a CCD sensor over a PSP plate system in connection with root canal treatment.33 A study by pediatric dentists also reported that an image could be obtained faster with sensors compared to a phosphor plate.30 One systematic review concluded that a reasonable amount of working time could be saved when switching from film to digital imaging in dental practice.34 On the other hand, few studies have reported that dentists working with digital receptors took more images and or more retakes than dentists working with film.3536
The findings of this study have allowed us to develop some recommendations that could be implemented within the teaching system, namely: 1) Since digital systems are becoming more convenient and require less monitoring, students should be encouraged to show radiographic image(s) to their clinical supervisors for comments prior to deciding alone on the value of the image that has been taken; 2) The clinical supervisors should do random checks on unverified images at the student's workstations to ensure minimal repeats are performed. This would avoid the students developing a complacent attitude and becoming overconfident from the use of such advanced technology;7 3) It would be useful to introduce reject/repeat tracking software in the digital radiography system, in which the student would need to specify the reason for the rejection/repetition before proceeding to another retake of an image. In conclusion, repeat analysis offers a method of quality assurance which can help in assessing the quality of the image, optimize examination protocols, identify students' education and training needs, and track patient radiation exposure. The moderately high repeat rate observed in this study warrants revisiting the fundamental training in techniques and radiation protection among undergraduate dental students. Students need to understand the radiation dosage delivered to the patient while taking into consideration the extent of repetition of X-ray images that have been taken. Repeat analysis also provides a valuable tool for calculating the radiation dosage delivered to patients.
Figures and Tables
Fig. 1
A. Images taken on first examination. B. Repeat due to inadequate clearance of periapical lesion on endodontically-treated tooth.

Fig. 2
Percentages of repeat rates of intraoral images according to procedure and student year in dental school.

Acknowledgements
The authors would like to thank all the radiographers of the Diagnostic Imaging Unit, Faculty of Dentistry, Universiti Teknologi MARA for their help in acquiring the images in this study. No conflict of interest is declared in this work.
References
1. Pitcher EM, Wells PN. Quality assurance and radiologic audit. Curr Opin Radiol. 1992; 4:9–14.
2. McKinney WE. Repeat exposures: our little secret. Radiol Technol. 1994; 65:319–320.
3. Andersen ER, Jorde J, Taoussi N, Yaqoob SH, Konst B, Seierstad T. Reject analysis in direct digital radiography. Acta Radiol. 2012; 53:174–178.

4. Waaler D, Hofmann B. Image rejects/retakes - radiographic challenges. Radiat Prot Dosimetry. 2010; 139:375–379.
5. Jones AK, Polman R, Willis CE, Shepard SJ. One year’s results from a server-based system for performing reject analysis and exposure analysis in computed radiography. J Digit Imaging. 2011; 24:243–255.

6. Foos DH, Sehnert WJ, Reiner B, Siegel EL, Segal A, Waldman DL. Digital radiography reject analysis: data collection methodology, results, and recommendations from an in-depth investigation at two hospitals. J Digit Imaging. 2009; 22:89–98.

7. Nol J, Isouard G, Mirecki J. Digital repeat analysis; setup and operation. J Digit Imaging. 2006; 19:159–166.

8. Peer S, Peer R, Giacomuzzi SM, Jaschke W. Comparative reject analysis in conventional film-screen and digital storage phosphor radiography. Radiat Prot Dosimetry. 2001; 94:69–71.

9. Hofmann B, Rosanowsky TB, Jensen C, Wah KH. Image rejects in general direct digital radiography. Acta Radiol Open. 2015; 4:2058460115604339.

10. Rogers KD, Matthews IP, Roberts CJ. Variation in repeat rates between 18 radiology departments. Br J Radiol. 1987; 60:463–468.

11. Watkinson S, Moores BM, Hill SJ. Reject analysis: its role in quality assurance. Radiography. 1984; 50:189–194.
12. Honea R, Elissa Blado M, Ma Y. Is reject analysis necessary after converting to computed radiography? J Digit Imaging. 2002; 15:Suppl 1. 41–52.

13. Weatherburn GC, Bryan S, West M. A comparison of image reject rates when using film, hard copy computed radiography and soft copy images on picture archiving and communication systems (PACS) workstations. Br J Radiol. 1999; 72:653–660.

14. Lin CS, Chan PC, Huang KH, Lu CF, Chen YF, Chen YO. Guidelines for reducing image retakes of general digital radiography. Adv Mech Eng. 2016; 8:1687814016644127.

15. Shi XQ, Benchimol D, Näsström K. Comparison of psychophysical properties of two intraoral digital sensors on low-contrast perceptibility. Dentomaxillofac Radiol. 2013; 42:20130249.

16. Farman AG, Farman TT. A comparison of 18 different x-ray detectors currently used in dentistry. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005; 99:485–489.

17. Mesgarani A, Haghanifar S, Ehsani M, Yaghub SD, Bijani A. Accuracy of conventional and digital radiography in detecting external root resorption. Iran Endod J. 2014; 9:241–245.
18. Anas A, Asaad J, Tarboush K. A comparison of intra-oral digital imaging modalities: charged couple device versus storage phosphor plate. Int J Health Sci (Qassim). 2010; 4:156–167.
19. Dashpuntsag O, Yoshida M, Kasai R, Maeda N, Hosoki H, Honda E. Numerical evaluation of image contrast for thicker and thinner objects among current intraoral digital imaging systems. Biomed Res Int. 2017; 2017:5215413.

20. Culmer PJ. Chesneys' care of patient in diagnostic radiography. 7th Ed. Oxford: Blackwell Science;1995.
21. Moores BM. Practical guide to quality assurance in medical imaging. Chichectser: Wiley;1987.
22. Clark CA. A method of ascertaining the relative position of unerupted teeth by means of film radiographs. Proc R Soc Med. 1910; 3:87–90.

23. Berrington de González A, Darby S. Risk of cancer from diagnostic X-rays: estimates for the UK and 14 other countries. Lancet. 2004; 363:345–351.
24. Brenner DJ, Hall EJ. Computed tomography - an increasing source of radiation exposure. N Engl J Med. 2007; 357:2277–2284.

25. Dunn MA, Rogers AT. X-ray film reject analysis as a quality indicator. Radiography (Lond). 1998; 4:29–31.

26. Lau SL, Mak AS, Lam WT, Chau CK, Lau KY. Reject analysis: a comparison of conventional film-screen radiography and computed radiography with PACS. Radiography (Lond). 2004; 10:183–187.

27. Peer S, Peer R, Walcher M, Pohl M, Jaschke W. Comparative reject analysis in conventional film-screen and digital storage phosphor radiography. Eur Radiol. 1999; 9:1693–1696.

28. Prieto C, Vano E, Ten JI, Fernandez JM, Iniguez AI, Arevalo N, et al. Image retake analysis in digital radiography using DICOM header information. J Digit Imaging. 2009; 22:393–399.

29. Bin-Shuwaish M, Dennison JB, Yaman P, Neiva G. Estimation of clinical axial extension of Class II caries lesions with ultraspeed and digital radiographs: an in-vivo study. Oper Dent. 2008; 33:613–621.

30. Russo JM, Russo JA, Guelmann M. Digital radiography: a survey of pediatric dentists. J Dent Child (Chic). 2006; 73:132–135.
31. Fintelmann F, Pulli B, Abedi-Tari F, Trombley M, Shore MT, Shepard JA, et al. Repeat rates in digital chest radiography and strategies for improvement. J Thorac Imaging. 2012; 27:148–151.

32. Tzeng WS, Kuo KM, Liu CF, Yao HC, Chen CY, Lin HW. Managing repeat digital radiography images - a systematic approach and improvement. J Med Syst. 2012; 36:2697–2704.
33. Wenzel A, Kirkevang LL. Students' attitudes to digital radiography and measurement accuracy of two digital systems in connection with root canal treatment. Eur J Dent Edu. 2004; 8:167–171.

34. Wenzel A, Møystad A. Work flow with digital intraoral radiography: a systemic review. Acta Odontol Scand. 2010; 68:106–114.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download