Abstract
Purpose
The purpose of this study was to measure the buccal bone thickness and angulation of the maxillary incisors and to analyze the correlation between these parameters and the root position in the alveolar bone using cone-beam computed tomography (CBCT).
Materials and Methods
CBCT images of 398 maxillary central and lateral incisors from 199 patients were retrospectively reviewed. The root position in the alveolar bone was classified as buccal, middle, or palatal, and the buccal type was further classified into subtypes I, II, and III. In addition, the buccolingual inclination of the tooth and buccal bone thickness were evaluated.
Results
A majority of the maxillary incisors were positioned more buccally within the alveolar bone, and only 2 lateral incisors (0.5%) were positioned more palatally. The angulation of buccal subtype III was the greatest and that of the middle type was the lowest. Most of the maxillary incisors exhibited a thin facial bone wall, and the lateral incisors had a significantly thinner buccal bone than the central incisors. The buccal bone of buccal subtypes II and III was significantly thinner than that of buccal subtype I.
Conclusion
A majority of the maxillary incisor roots were positioned close to the buccal cortical plate and had a thin buccal bone wall. Significant relationships were observed between the root position in the alveolar bone, the angulation of the tooth in the alveolar bone, and buccal bone thickness. CBCT analyses of the buccal bone and sagittal root position are recommended for the selection of the appropriate treatment approach.
The implant position is one of the most important determinants of the long-term maintenance of implant esthetics and function.1 If an implant could be placed into the extraction socket at the same angulation as the that of the root inside the alveolar bone, the prosthetic crown would have an ideal position.23 Although the position of an implant should be based on future restoration plans, the placement of an implant axis in alignment with the crown is often limited by the morphology of the alveolar ridge.1
In addition to the root position in its alveolar socket, the thickness of the facial bone wall is also of crucial importance in selecting an appropriate treatment approach and determining the dimensions of the implant.45 In a previous study, the buccal bone wall of the anterior tooth was found to be very thin in most patients; therefore, the implant was positioned slightly on the palatal side to ensure sufficient buccal bone thickness.3 Especially in the esthetic zone, the facial bone wall is often thin and is predominantly composed of the bundle bone, such that its resorption results in a vertical reduction of the facial bony crest.6 Clinical guidelines suggest that a minimal buccal bone thickness of 1–2 mm is required to maintain the tissue architecture following tooth extraction and implant placement.7
The sagittal root position can have a significant impact on the occurrence of labial bone perforation, and cone-beam computed tomography (CBCT) images of the root position within the alveolar bone provide information that is useful for avoiding labial bone perforation.8 Therefore, preoperative diagnostic procedures are required to assess the risk factors for implant placement.49 Preoperative CBCT is now routine for implant placement, especially in the esthetic zone, both because of its accuracy and because of its convenience and low radiation dosage.10111213
The objective of this study was to measure the buccal bone thickness and angulation of the maxillary incisors and to analyze the correlation between these parameters and the root position in the alveolar bone using CBCT.
This study was approved by the Institutional Review Board of Pusan National University Dental Hospital. The subjects of this retrospective study were randomly selected from patients who visited Pusan National University Dental Hospital and underwent CBCT imaging between 2013 and 2014. Each image was examined to identify fully formed, intact, and healthy maxillary incisors for analysis. The CBCT data were excluded if any radiographically detectable caries, periapical pathology, alveolar bone loss of more than 4 mm from the cementoenamel junction, restoration, fracture, or history of orthodontic treatment was present. A total of 199 CBCT images met the inclusion criteria, resulting in a sample size of 398 maxillary central and lateral incisors. The patients comprised 100 males and 99 females, with a mean age of 28.3 years (range, 20–50 years).
All images used in this study were obtained using a PaX-Zenith 3D apparatus (Vatech Co., Hwaseong, Korea), with 5.7 mA, 110 kV, 24 s exposure time, 0.2 mm voxel size, and a field of view of 16×14 cm or 12×9 cm. CBCT data were saved in the Digital Imaging and Communications in Medicine format, and the images were analyzed using Ez3D Plus Professional CBCT software (Vatech Co., Hwaseong, Korea).
The arch form selector tool was centered at the middle of the arch in the axial plane. The root position, angulation, and buccal bone thickness were evaluated by viewing the cross-sectional images made at the midpoint of the tooth parallel to its long axis. The root position of the maxillary incisor in the alveolar bone was evaluated according to the position of the apex.14 The root position of the incisors was classified as follows: buccal type, the apical point of the incisor was within the buccal third of the alveolar bone and the root was closer to the buccal bone wall; middle type, the apical point of the incisor was within the middle third of the alveolar bone and the buccal and palatal bone walls were approximately equal in thickness; and palatal type, the apical point of the incisor was within the palatal third of the alveolar bone and the root was closer to the palatal bone wall (Fig. 1). The buccal type was further classified into subtypes I, II, and III. In subtype I, the incisor root was covered by the buccal bone wall and the bone thickness increased toward the apex. In subtype II, the incisor root was covered by a thinner buccal bone wall than found in subtype I and the bone thickness did not noticeably increase toward the apex that was covered by the bone tissue in the long axis of the tooth. In subtype III, the axis of the apex was angulated very buccally and the apex was not covered by the bone tissue in the long axis of the tooth (Fig. 2).
Furthermore, the angle between the long axis of the tooth and the long axis of the corresponding alveolar bone was determined. The long axis of the tooth was defined as the line through the lowest point of the crown to the highest point of the apex in the cross-sectional image (Fig. 3). The thickness of the buccal bone wall was assessed perpendicular to the long axis of the tooth at the following 5 locations: at the crest; 2, 4, and 6 mm apical to the crest; and at the root apex. If the root apex was located anterior to the natural contour of the maxillary alveolar buccal bone and the extremely thin bony wall belonged to buccal subtype III, a value of 0 mm was used to record the buccal bone thickness (Fig. 4).
All measurements were performed by a single examiner. The Kolmogorov-Smirnov test was used to determine the normality of the data. To estimate the intraexaminer deviations in the measurements, assessments of the maxillary incisors of 30 patients were performed twice. Two sets of measurements were carried out at different times on the same CBCT scans. The Wilcoxon signed-rank test was used to compare the numeric values of the duplicate measurements, and no significant differences were noted between the 2 sets of measurements. Moreover, no significant differences were observed between the measurements on the right and left sides. The Wilcoxon signed-rank test was used to compare the angulation and buccal bone thickness between the central and lateral incisors because the samples did not follow a normal distribution. The buccal bone thickness was presented as mean±standard deviation. In addition, the buccal bone thickness was grouped into the following categories for descriptive analysis: missing bone wall, bone thickness <1 mm, and bone thickness ≥1 mm. The Kruskal-Wallis test was conducted to compare the buccal bone thickness and angulation according to the root position. P values <.05 were considered to indicate statistical significance. The statistical analyses were performed using SPSS version 23.0 (IBM Corp., Armonk, NY, USA).
In this study, the root position within the alveolar bone was examined. A majority of the maxillary incisors were positioned more buccally within the alveolar bone. Among the buccal-type incisors, 64.3% of the central incisors were classified as subtype I and 67.6% of the lateral incisors were classified as subtype II. Only 2 lateral incisors (0.5%) were positioned more palatally (Table 1).
Furthermore, the angulation of the maxillary incisor within the alveolar bone was determined. The angulation of the maxillary lateral incisor was significantly greater than that of the central incisor (P<.05). The angulation of buccal subtype III was the greatest and that of the middle type was the lowest. A significant relationship between the root position within the alveolar bone and the angulation in the alveolar bone was found (P<.05; Table 2).
The mean thickness of the facial bone wall was 0.92 mm at the central incisors and 0.57 mm at the lateral incisors. The maxillary lateral incisors demonstrated a significantly thinner buccal bone thickness than the central incisors (P<.05). In the lateral incisors, the lowest bone thickness was observed 6 mm apical to the crest (Table 3).
A majority of the maxillary incisors exhibited a thin buccal bone wall (<1 mm). In addition, a thick buccal bone wall (≥1 mm) was found in 41.7% of the central incisors and 15.7% of the lateral incisors. The lowest percentage (4.5%) of thick walls was found 6 mm apical to the crest of the lateral incisors. At the root apex, the buccal bone was missing in 3.8% of the central incisors and 18.3% of the lateral incisors (Table 4).
Table 5 shows the buccal bone thickness of the maxillary incisors according to sagittal root position. The buccal bone thickness of buccal subtypes II and III was significantly thinner than that of buccal subtype I at 4 mm, 6 mm, and the root apex of the central incisors and at 2 mm, 4 mm, 6 mm, and the root apex of the lateral incisors, respectively (P<.05). The buccal bone thickness gradually decreased apically at 2, 4, and 6 mm in buccal subtypes II and III.
In this study, we investigated the root position in the alveolar bone, the sagittal angulation between the long axes of the teeth and their respective alveolar bone, and the buccal bone thickness of the maxillary incisors on CBCT images. Several studies have investigated the root position of the maxillary central incisors in the alveolar bone and have reported that the buccal type was the predominant incisor root position.25141516 In our study, the buccal type of root position was identified in more than 90% of cases and the palatal type was found in only 2 cases (5%) of the lateral incisors, similar to the results of previous reports.51416
We further classified the buccal type into 3 subtypes based on the thickness of the buccal bone wall at different root levels and the presence of an apical bone wall. Patients with buccal subtype I had an adequate buccal bone thickness and bone wall around the root. During immediate placement, the direction of placement more or less coincided with the long axis of the tooth.1417 In our study, buccal subtype I accounted for 64.3% of the central incisors and 8.0% of the lateral incisors. The buccal subtype II incisors had a thinner buccal bone wall than buccal subtype I, and immediate placement was more challenging than in patients with subtype I in such cases.14 The buccal subtype III teeth not only had a very thin buccal plate, but the axis of the root apex was also angulated very buccally, passing anterior to the natural contour of the maxillary alveolar bone.2 Therefore, patients with a subtype III root position may not be suitable for immediate placement.214 In this study, subtypes II and III were more frequent in the lateral incisors than in the central incisors.
The buccolingual inclination of the tooth was critical in determining the appropriate dental implant treatment approach and implant size.3 In this study, the angle between the long axis of the tooth and the long axis of the corresponding alveolar bone was less than 10° in buccal subtype I and the middle type. It may be relatively easy to insert implants into this kind of extraction socket. In our results, the angulation of buccal subtype III was the greatest, to the point that the implant position might be compromised.23
Numerous studies have revealed that a thin facial alveolar bone wall is usually present in the anterior maxilla.41518192021 Hence, in most situations, adjunctive bone augmentation has been recommended for immediate or early implant placement in the anterior esthetic zone.182223 The vertical resorption of the buccal crest was 3 times greater at sites with a thin buccal bone (<1 mm) than at sites with a thick buccal bone (≥1 mm).24 In this study, the buccal bone was thin (<1 mm) in 58.3% of the central incisors and 84.3% of the lateral incisors. Moreover, a statistically significant association was noted between the root position in its socket and the buccal bone thickness, and the buccal bone was significantly thinner in buccal subtypes II and III than in buccal subtype I. The buccal bone of the middle type was significantly thicker than that of buccal subtype I in the central incisors. However, there was no significant difference in buccal bone thickness between buccal subtype I and the middle type in the lateral incisors because the lateral incisors had thinner alveolar bones than the central incisors.
In conclusion, a majority of the maxillary incisors were positioned close to the buccal cortical plate and had a thin buccal bone wall. Significant relationships were noted between the root position in the alveolar bone, angulation in the alveolar bone, and buccal bone thickness. CBCT analyses of the buccal bone and sagittal root position are recommended for the selection of an appropriate treatment approach.
Figures and Tables
Fig. 1
The root position of the incisors in the alveolar bone is classified as the buccal, middle, or palatal type. A. Buccal type: the apical point of the incisor is within the buccal third of the alveolar bone and the root is closer to the buccal bone wall. B. Middle type: the apical point of the incisor is within the middle third of the alveolar bone and the buccal and palatal bone walls are approximately equal in thickness. C. Palatal type: the apical point of the incisor is within the palatal third of the alveolar bone and the root is closer to the palatal bone wall.

Fig. 2
The buccal type is further classified as follows. A. Subtype I: the incisor root is covered by the buccal bone wall, and the bone thickness increases toward the apex. B. Subtype II: the incisor root is covered by a thinner buccal bone wall than in subtype I and the bone thickness does not noticeably increase toward the apex that is covered by the bone tissue in the long axis of the tooth. C. Subtype III: the axis of the apex is angulated very buccally and the apex is not covered by the bone tissue in the long axis of the tooth.

Fig. 3
The angle between the long axis of the tooth and the long axis of the corresponding alveolar bone is measured.

Fig. 4
The thickness of the buccal bone is measured at the alveolar crest; 2, 4, and 6 mm apical to the alveolar crest; and at the root apex.
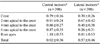
Table 2
Angulation of the maxillary incisors with reference to the alveolar bone according to the root position (unit: degrees)

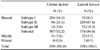
Table 3
Buccal bone thickness measurements at the alveolar crest; 2, 4, and 6 mm apical to the alveolar crest; and at the root apex for the maxillary incisors (unit: mm)
References
1. Chan HL, Garaicoa-Pazmino C, Suarez F, Monje A, Benavides E, Oh TJ, et al. Incidence of implant buccal plate fenestration in the esthetic zone: a cone beam computed tomography study. Int J Oral Maxillofac Implants. 2014; 29:171–177.

2. Lau SL, Chow J, Li W, Chow LK. Classification of maxillary central incisors-implications for immediate implant in the esthetic zone. J Oral Maxillofac Surg. 2011; 69:142–153.

3. Wang HM, Shen JW, Yu MF, Chen XY, Jiang QH, He FM. Analysis of facial bone wall dimensions and sagittal root position in the maxillary esthetic zone: a retrospective study using cone beam computed tomography. Int J Oral Maxillofac Implants. 2014; 29:1123–1129.

4. Braut V, Bornstein MM, Belser U, Buser D. Thickness of the anterior maxillary facial bone wall-a retrospective radiographic study using cone beam computed tomography. Int J Periodontics Restorative Dent. 2011; 31:125–131.
5. Kan JY, Roe P, Rungcharassaeng K, Patel RD, Waki T, Lozada JL, et al. Classification of sagittal root position in relation to the anterior maxillary osseous housing for immediate implant placement: a cone beam computed tomography study. Int J Oral Maxillofac Implants. 2011; 26:873–876.
6. Araújo MG, Lindhe J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol. 2005; 32:212–218.

7. Grunder U, Gracis S, Capelli M. Influence of the 3-D bone-to-implant relationship on esthetics. Int J Periodontics Restorative Dent. 2005; 25:113–119.
8. Sung CE, Cochran DL, Cheng WC, Mau LP, Huang PH, Fan WH, et al. Preoperative assessment of labial bone perforation for virtual immediate implant surgery in the maxillary esthetic zone: a computer simulation study. J Am Dent Assoc. 2015; 146:808–819.
9. El Nahass H, Naiem SN. Analysis of the dimensions of the labial bone wall in the anterior maxilla: a cone-beam computed tomography study. Clin Oral Implants Res. 2015; 26:e57–e61.

10. Rugani P, Kirnbauer B, Arnetzl GV, Jakse N. Cone beam computerized tomography: basics for digital planning in oral surgery and implantology. Int J Comput Dent. 2009; 12:131–145.
12. Mandelaris GA, Rosenfeld AL. The expanding influence of computed tomography and the application of computer-guided implantology. Pract Proced Aesthet Dent. 2008; 20:297–305.
13. Guerrero ME, Noriega J, Jacobs R. Preoperative implant planning considering alveolar bone grafting needs and complication prediction using panoramic versus CBCT images. Imaging Sci Dent. 2014; 44:213–220.

14. Xu D, Wang Z, Sun L, Lin Z, Wan L, Li Y, et al. Classification of the root position of the maxillary central incisors and its clinical significance in immediate implant placement. Implant Dent. 2016; 25:520–524.

15. Khoury J, Ghosn N, Mokbel N, Naaman N. Buccal bone thickness overlying maxillary anterior teeth: a clinical and radiographic prospective human study. Implant Dent. 2016; 25:525–531.
16. Chung SH, Park YS, Chung SH, Shon WJ. Determination of implant position for immediate implant placement in maxillary central incisors using palatal soft tissue landmarks. Int J Oral Maxillofac Implants. 2014; 29:627–633.

17. Vera C, De Kok IJ, Reinhold D, Limpiphipatanakorn P, Yap AK, Tyndall D, et al. Evaluation of buccal alveolar bone dimension of maxillary anterior and premolar teeth: a cone beam computed tomography investigation. Int J Oral Maxillofac Implants. 2012; 27:1514–1519.
18. Huynh-Ba G, Pjetursson BE, Sanz M, Cecchinato D, Ferrus J, Lindhe J, et al. Analysis of the socket bone wall dimensions in the upper maxilla in relation to immediate implant placement. Clin Oral Implants Res. 2010; 21:37–42.

19. Nowzari H, Molayem S, Chiu CH, Rich SK. Cone beam computed tomographic measurement of maxillary central incisors to determine prevalence of facial alveolar bone width ≥2 mm. Clin Implant Dent Relat Res. 2012; 14:595–602.
20. Januário AL, Duarte WR, Barriviera M, Mesti JC, Araújo MG, Lindhe J. Dimension of the facial bone wall in the anterior maxilla: a cone-beam computed tomography study. Clin Oral Implants Res. 2011; 22:1168–1171.

21. Zekry A, Wang R, Chau AC, Lang NP. Facial alveolar bone wall width - a cone-beam computed tomography study in Asians. Clin Oral Implants Res. 2014; 25:194–206.

22. Miyamoto Y, Obama T. Dental cone beam computed tomography analyses of postoperative labial bone thickness in maxillary anterior implants: comparing immediate and delayed implant placement. Int J Periodontics Restorative Dent. 2011; 31:215–225.
23. Buser D, Chen ST, Weber HP, Belser UC. Early implant placement following single-tooth extraction in the esthetic zone: biologic rationale and surgical procedures. Int J Periodontics Restorative Dent. 2008; 28:441–451.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download