Abstract
Purpose
This study determined and compared the distances from the maxillary root apices of posterior teeth to the floor of the maxillary sinus, or maxillary sinus distances (MSDs), and the distances from the mandibular root apices of the posterior teeth to the mandibular canal, or mandibular canal distances (MCDs), in Thai subjects with skeletal open bite and skeletal normal bite.
Materials and Methods
Pretreatment cone-beam computed tomography (CBCT) images were obtained from 30 Thai orthodontic patients (15 patients with skeletal normal bite and 15 with skeletal open bite) whose ages ranged from 14 to 28 years. The CBCT images of the patients were processed and measured using the Romexis Viewer program. The MSDs and MCDs from the root apices of the maxillary and mandibular second premolar, first molar, and second molar to the maxillary sinus floor or the mandibular canal were measured perpendicularly to the occlusal plane. The Student t test was used for comparisons between the 2 groups.
Results
The greatest mean MSDs were from the root apex of the second premolars in both groups, whereas the least mean MSDs were from the mesiobuccal root apex of the second molars. The greatest mean MCDs were from the mesial root apex of the first molars, whereas the least mean MCDs were from the distal root apex of the second molars.
The maxillary sinus is the largest of the paranasal sinuses and the first to develop. The growth of the maxillary sinus ends at approximately 20 years of age with the eruption of the third molars. The extension of the maxillary sinus in adults is variable. In half the population, the sinus floor extends between adjacent teeth or roots, causing elevations in the surface known as ‘hillocks’. The roots of the maxillary posterior teeth may project into the sinus and present various clinical implications in contexts including orthodontic treatment planning. The distance between the maxillary sinus floor and the roots of the maxillary posterior teeth plays a crucial role in treatment planning for orthodontic tooth movement. One treatment for patients with skeletal open bite is the intrusion of the molar teeth into their sockets to reduce the open bite, thereby reducing the vertical dimension of the face. However, intrusion or bodily movement of teeth through the sinus floor has been shown to cause a high degree of tipping and moderate apical root resorption.123 Therefore, knowledge of the topography between the inferior wall of the maxillary sinus and the root apices of the maxillary posterior teeth is important for diagnosis and treatment planning in orthodontics.4
The mandibular canals are bilateral anatomical structures extending from the mandibular foramen to the mental foramen, carrying the inferior alveolar nerves, arteries, and veins.5 The identification of the mandibular canal is important in treatment planning involving the posterior mandible. Several imaging techniques have been used to identify the mandibular canal, such as panoramic radiography, conventional radiography, computed tomography, and cone-beam computed tomography (CBCT). Compared to 2-dimensional techniques, CBCT has the advantage of eliminating the superimposition of adjacent structures and not involving image magnification. CBCT has the further advantages of a short scanning time, low radiation dose, and increasing availability in dental and radiological practices, and has been shown to be more effective than conventional radiography for the depiction of the mandibular canal.6
Information regarding the distances between the root apices and the maxillary sinus and mandibular canal in different skeletal types is still limited. Studies in the Thai population are needed to provide useful information for treatment planning. Therefore, the objective of this study was to determine the distances from the root apices of the maxillary posterior teeth to the maxillary sinus, and from the root apices of the mandibular posterior teeth to the mandibular canal, in Thai patients by using 3-dimensional CBCT imaging.
This study was approved by the Human Experimentation Committee (No 19/2015), Faculty of Dentistry, Chiang Mai University, Thailand. The patients were informed of the study procedure, and provided written informed consent before the CBCT images were obtained.
The patients included in this study were randomly selected. The selected patients met the following criteria: (1) anterior open bite, (2) full eruption of permanent dentition (except for the third molars), (3) no history of previous orthodontic treatment, (4) no missing posterior teeth (excluding the third molars), (5) no pathologic lesions or abnormalities of the maxillary sinus, (6) no pathologic lesions or abnormalities of the mandibular canal, (7) no severe craniofacial disorders, (8) no radiographic signs of periapical disease, (9) no severe crowding of the posterior teeth, (10) orthodontic treatment planning that required intrusion of the posterior teeth, (11) a class I skeletal pattern (A point, nasion, B point angle of 0°–4°) with either skeletal normal bite or skeletal open bite, and (12) orthodontic treatment planning that required mini-screw implant placement.
Pretreatment CBCT images were analyzed from 30 Thai orthodontic patients, comprising 15 patients with anterior open bite and 15 with skeletal normal bite according to their cephalometric measurements using the criteria set by Cangialosi.7 The mean cephalometric values for the skeletal normal bite and skeletal open bite groups are shown in Table 1, together with the values from the study of Cangialosi in 1984.
All CBCT images were obtained in the Oral and Maxillofacial Radiology Clinic, Dental Hospital, Faculty of Dentistry, Chiang Mai University, using a ProMax 3D (Planmeca OY, Helsinki, Finland) CBCT machine, at 84 kVp, 10 mA, and an 8-×8-cm field of view with a voxel size of 0.16 mm. Each patient was positioned in the device with the occlusal plane parallel to the floor.
The Planmeca Romexis Viewer 2.3.1.R program (Planmeca OY, Helsinki, Finland) was used for orthogonal tomographic image reconstruction and measurement. A slice thickness of 0.32 mm was set for the measurements. The distances between the apices of the maxillary posterior teeth (second premolar, first and second molars) and the maxillary sinus floor, or maxillary sinus distances (MSDs), and the distances between the apices of the mandibular posterior teeth (second premolar, first and second molars) and the mandibular canal, or mandibular canal distances (MCDs) in both the skeletal normal bite group and the skeletal open bite group were examined. Twelve periapical areas on each side (left and right) were surveyed in each subject. The vertical distances from each root apex of the second premolars and first and second molars to the maxillary sinus floor and to the mandibular canal were measured perpendicularly to the occlusal plane.
In the coronal and sagittal slice images (Fig. 1A and B), the CBCT images were adjusted until the horizontal blue lines were parallel to the occlusal plane. The sagittal CBCT images (Fig. 1B) were adjusted until the vertical red line in the coronal slice images (Fig. 1A) was perpendicular to the occlusal plane and passed through the root apex to be measured. The coronal CBCT images (Fig. 1A) were adjusted until the vertical green line in the sagittal slice image was perpendicular to the occlusal plane and passed through the root apex to be measured.
In the coronal slice, the distance from the apex of each root of the maxillary posterior teeth (second premolar, first and second molars) to the maxillary sinus floor (Fig. 2) and the mandibular canal (Fig. 3) were measured perpendicularly to the occlusal plane. The apices extending below the floor of the sinus were assigned positive values, whereas the apices above the sinus floor were assigned negative values.
The measurements were performed twice, with a 4-week interval. The examiner was one of the authors (WK), a third-year graduate student in the orthodontics program who had been trained by an experienced oral and maxillofacial radiologist. Intra-examiner reliability was assessed using the paired t test (P<.05). The unpaired t test was used to analyze differences between measurements on the right and the left sides. Descriptive statistics were used to describe the means and standard deviations of the measurements. The independent t test was used to compare the mean of all the studied measurements between the 2 groups of patients (skeletal normal bite group and skeletal open bite group); P values <.05 were considered to indicate statistical significance.
No statistically significant differences were found between the measurements from the right and left sides. The measurements of the MSDs and MCDs from both the right and left sides were pooled to facilitate the determination of central trend measurements.
The distances between the apices of the maxillary posterior teeth (second premolar, first and second molars) and the maxillary sinus floor in patients with skeletal normal bite and those with skeletal open bite are shown in Table 2. The mean MSDs for the maxillary second premolars, first molars, and second molars in the skeletal normal bite group ranged from 0.19±1.82 mm to 2.44±3.15 mm. The greatest mean MSD was from the root apices of the second premolars, whereas the least mean MSD was from the mesiobuccal root apices of the second molars. The mean MSD from the palatal root apices was greater than the mean MSDs from the mesiodistal and distobuccal root apices in both the first molars and second molars. The mean MSDs for the maxillary second premolars, first molars, and second molars in the skeletal open bite group ranged from 0.35±1.01 mm to 1.92±2.21 mm. The greatest mean MSD was from the root apices of the second premolars, whereas the least mean MSD was from the mesiobuccal root apices of the second molars. The mean MSD from the palatal root apices was greater than the mean MSDs from the mesiodistal and distobuccal root apices in both the first molars and second molars. There were no statistically significant differences between the mean MSDs for the root apices of the maxillary second premolar, the mesiobuccal, distobuccal, or palatal root apices of the maxillary first molar, or the mesiobuccal, distobuccal, or palatal root apices of the maxillary second molar in either the skeletal normal bite group or the skeletal open bite group.
The distances between the apices of the mandibular posterior teeth (second premolar, first and second molars) and the mandibular canal in the patients with skeletal normal bite and in those with skeletal open bite are shown in Table 3. The mean MCDs for the mandibular second premolars, first molars, and second molars in the skeletal normal bite group ranged from 1.84±1.38 mm to 4.43±2.17 mm. The greatest mean MCD was from the mesial root apices of the first molars, whereas the least mean MCD was from the distal root apices of the second molars. The mean MCD from the mesial root apices was greater than the mean MCD from the distal root apices in both the first molars and second molars. The mean MCDs for the mandibular second premolars, first molars, and second molars in the skeletal open bite group ranged from 1.83±1.17 mm to 3.71±1.86 mm. The greatest mean MCD was from the mesial root apices of the first molars, whereas the least mean MCD was from the distal root apices of the second molars. The mean MCD from the mesial root apices was greater than the mean MCD from the distal root apices in both the first molars and second molars. There were no statistically significant differences between the mean MCDs of the root apices of the mandibular second premolar, the mesial or distal root apices of the mandibular first molar, or the mesial or distal root apices of the mandibular second molar in either the skeletal normal bite group or the skeletal open bite group. There were no significant differences between the repeated measurements.
CBCT measurements are now considered to have clinically acceptable accuracy in the study of the maxillary sinus and mandibular canal.89 Howe et al.8 studied first molar radicular bone near the maxillary sinus using CBCT measurements compared to gross anatomic dissections and found an acceptable accuracy of CBCT for valid measurements of the maxillary bone in this area. Kim et al.9 compared the distances from the apices of the second premolar and first and second molars to the superior-most of the mandibular canal using 2 different methods. The results showed no statistically significant differences between the CBCT imaging software measurements and the direct measurement of 12 human hemi-mandible specimens. Both methods were highly reproducible and predictable, and were closely correlated to each other.
Sharan and Madjar3 used panoramic radiography and cross-sectional CT to study the correlation between the maxillary sinus floor and the related root position of the maxillary posterior teeth. Their results showed a 2.1-times longer root projection into the sinus cavity on the panoramic radiographs than on CT images. Hassan10 also demonstrated that neither periapical radiographs nor panoramic radiographs were reliable for determining the exact relationship between the maxillary sinus floor and the apex of the maxillary teeth, although periapical radiographs were slightly more reliable than panoramic radiographs.
One of the orthodontic treatment options for open bite is posterior tooth intrusion. Daimaruya et al.11 used a skeletal anchorage system as intraoral rigid anchors for open bite correction by intrusion of the mandibular molars in dogs. The results showed an average of 3.4 mm of molar intrusion in 7 months, without inferior alveolar neurovascular damage. Repositioning of the inferior alveolar neurovascular bundles was found, together with remodeling of the inner surface of the cortical bone to enlarge the marrow spaces to avoid severe destruction of nerves and blood vessels. Root resorption, repaired with new cementum, was observed in the study with no serious iatrogenic problems. However, further investigation in humans is needed to clarify the possible effects of molar intrusion. The distances between the apices of the roots and the floor of the maxillary sinus or the upper rim of the mandibular canal are crucial factors for treatment planning before performing intrusion of the posterior teeth.
Various authors have studied the distances between posterior tooth roots and the maxillary sinus.24891213 Our findings are similar to those of some of these studies (Table 4). Kilic et al.2 studied CBCT images from 92 patients, measuring the distances between the deepest point of the maxillary sinus floor and the root tips of the maxillary posterior teeth, and found that the distance was longest for the first premolar root tip and shortest for the second premolar distobuccal root tip. No statistically significant differences were found between the left and right sides, or between male and female patients. Eberhardt et al.14 collected CT data from 38 human adult patients and 12 autopsy specimens, and found that the average distance from the maxillary posterior teeth to the floor of the maxillary sinus ranged from 0.83 mm for the mesiobuccal root of the second molar to 7.05 mm for the lingual root of the first premolar. Kwak et al.4 used CT images from 21 sides of the maxillae of hemi-sectioned Korean heads to study the topography of a dental infection spreading into the maxillary sinus by measuring the distances between each root apex and the inferior wall of the maxillary sinus, and found the longest distance in the first premolar area and the shortest distance in the second molar area. Jung and Cho12 assessed the vertical relationship of each root with the maxillary sinus in the CBCT images of 83 patients and found that protrusion into the maxillary sinus occurred most frequently with the buccal roots of the maxillary molars. Lateral projection into the maxillary sinus cavity occurred most frequently with the palatal roots of the maxillary first molars, and the closest roots to the maxillary sinus were the mesiobuccal roots of the maxillary second molar. No reports have evaluated the effects of different skeletal patterns on the distance from the maxillary sinus floor to the roots of the posterior teeth.
Studies of the inferior alveolar nerve canal are limited. Oliveira-Santos et al.6 reported difficult visibility of the mandibular canal in different regions. In CBCT images of 58 patients, the mandibular canal was clearly visible in 53% of hemi-mandibles, whereas 25% were difficult to see and 23% were very difficult. de Oliveira-Santos et al.5 also found unpredictability related to anatomical variations in the inferior alveolar canal, such as corticalization of the mandibular canal, an association of bifid mandibular canals with additional mental foramina, and anterior loops. Yamada et al.15 investigated the course of the inferior alveolar nerve and its branches using CBCT, and reported 155 branches in the mandibular third molar region in 106 cases.
However, few studies have been conducted of the distances from the mandibular canal to the adjacent root apices of the posterior teeth.1617 The results of our study are similar to those of previous studies (Table 5). Kovisto et al.16 evaluated the proximity of the mandibular canal to the root apices of the mandibular second premolar and the first and second molar teeth in 139 patients, grouped by age and sex. The results in all groups showed the root apices of the mandibular second molar to be the closest to the mandibular canal. The mesial root of the second molar in females was closer to the canal than in males, and the root apices in younger patients were generally closer to the canal than in older patients. Therefore, age and gender may affect the mandibular canal position. An individualized assessment of the distance between the root apices of the mandibular posterior teeth and the mandibular canal is crucial when attempting invasive treatment in this area. Sato et al.17 evaluated the presence of the mandibular canal and measured the mandibular molar areas of panoramic radiographs of 75 mandibles from Japanese cadavers. The results showed that the shortest mean distance to the mandibular canal was from the distal root of the second molar (0.70 mm), and that the longest mean distance to the mandibular canal was from the mesial root of the first molar (1.06 mm).
In summary, we found that the maxillary sinus distances were shortest in the area of the buccal roots of the maxillary second molars. In both the first and second maxillary molars, the buccal root apices were closer to the maxillary sinus floor than the palatal root apices. The mandibular canal distances were shortest in the area of the distal roots of the mandibular second molars. The distances tended to increase anteriorly, except for the second premolar area, where the mandibular canal extends upward to open at the mental foramen, resulting in a slight shortening of the mandibular canal distances. The results were the same in subjects with skeletal normal bite and those with skeletal open bite.
It is essential for clinicians to be aware of the very close anatomical relationships between the root apices of the posterior teeth and the maxillary sinus and the mandibular canal. Dental treatments in these areas should be performed with caution. Future studies should address the limitations of this study, such as the small sample size and the limited field of view of the CBCT imaging system.
Figures and Tables
Fig. 1
Screen capture shows the orientation of the cone-beam computed tomography images of the right maxillary first molar for the measurements. A. Coronal view. B. Sagittal view. C. Axial view.
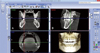
Fig. 2
Screen capture shows the distance between the root apex of the maxillary posterior teeth and maxillary sinus floor (white line).
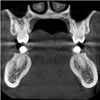
Fig. 3
Screen capture shows the distance (white line) between the root apex of the mandibular posterior teeth and mandibular canal (dotted white circle).
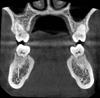
Table 1
Cephalometric values of the skeletal normal bite and skeletal open bite groups according to the criteria set by Cangiolosi7

Table 2
Maxillary sinus distances (MSDs) of the maxillary second premolars, first molars, and second molars in patients with skeletal normal bite and skeletal open bite (units: mm)

Table 3
Mandibular canal distances (MCDs) of the mandibular second premolars, first molars, and second molars in patients with skeletal normal bite and skeletal open bite (units: mm)

Acknowledgements
The authors are grateful to Dr. Thanapat Sastraruji, Dentistry Research Center, Faculty of Dentistry, Chiang Mai University, for his knowledge and suggestions in the statistical analysis of the data. The authors also would like to thank Dr. M. Kevin O Carroll, Professor Emeritus of the University of Mississippi School of Dentistry, USA and Faculty Consultant, Faculty of Dentistry, Chiang Mai University, Thailand, for his help with the manuscript preparation.
References
1. Fuhrmann R, Bucker A, Diedrich P. Radiological assessment of artificial bone defects in the floor of the maxillary sinus. Dentomaxillofac Radiol. 1997; 26:112–116.

2. Kilic C, Kamburoglu K, Yuksel SP, Ozen T. An assessment of the relationship between the maxillary sinus floor and the maxillary posterior teeth root tips using dental cone-beam computerized tomography. Eur J Dent. 2010; 4:462–467.

3. Sharan A, Madjar D. Correlation between maxillary sinus floor topography and related root position of posterior teeth using panoramic and cross-sectional computed tomography imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 102:375–381.

4. Kwak HH, Park HD, Yoon HR, Kang MK, Koh KS, Kim HJ. Topographic anatomy of the inferior wall of the maxillary sinus in Koreans. Int J Oral Maxillofac Surg. 2004; 33:382–388.

5. de Oliveira-Santos C, Souza PH, de Azambuja Berti-Couto S, Stinkens L, Moyaert K, Rubira-Bullen IR, et al. Assessment of variations of the mandibular canal through cone beam computed tomography. Clin Oral Investig. 2012; 16:387–393.

6. Oliveira-Santos C, Capelozza AL, Dezzoti MS, Fischer CM, Poleti ML, Rubira-Bullen IR. Visibility of the mandibular canal on CBCT cross-sectional images. J Appl Oral Sci. 2011; 19:240–243.

8. Howe RB. First molar radicular bone near the maxillary sinus: a comparison of CBCT analysis and gross anatomic dissection for small bony measurement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 108:264–269.

9. Kim TS, Caruso JM, Christensen H, Torabinejad M. A comparison of cone-beam computed tomography and direct measurement in the examination of the mandibular canal and adjacent structures. J Endod. 2010; 36:1191–1194.

10. Hassan BA. Reliability of periapical radiographs and orthopantomograms in detection of tooth root protrusion in the maxillary sinus: correlation results with cone beam computed tomography. J Oral Maxillofac Res. 2010; 1:e6.

11. Daimaruya T, Nagasaka H, Umemori M, Sugawara J, Mitani H. The influences of molar intrusion on the inferior alveolar neurovascular bundle and root using the skeletal anchorage system in dogs. Angle Orthod. 2001; 71:60–70.
12. Jung YH, Cho BH. Assessment of the relationship between the maxillary molars and adjacent structures using cone beam computed tomography. Imaging Sci Dent. 2012; 42:219–224.

13. Ariji Y, Obayashi N, Goto M, Izumi M, Naitoh M, Kurita K, et al. Roots of the maxillary first and second molars in horizontal relation to the alveolar cortical plates and maxillary sinus: computed tomography assessment for infection spread. Clin Oral Investig. 2006; 10:35–41.
14. Eberhardt JA, Torabinejad M, Christiansen EL. A computed tomographic study of the distances between the maxillary sinus floor and the apices of the maxillary posterior teeth. Oral Surg Oral Med Oral Pathol. 1992; 73:345–346.

15. Yamada T, Ishihama K, Yasuda K, Hasumi-Nakayama Y, Ito K, Yamaoka M, et al. Inferior alveolar nerve canal and branches detected with dental cone beam computed tomography in lower third molar region. J Oral Maxillofac Surg. 2011; 69:1278–1282.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download