Abstract
Purpose
Obstructive and inflammatory disease often occurs in the major salivary glands, and no predictive treatment has yet been developed for this condition. The aim of this report was to introduce an intraductal irrigation procedure and to illustrate its application to practical patient cases.
Materials and Methods
Two patients complaining of pain and swelling in the parotid gland during meals who underwent sialography were diagnosed as having sialodochitis with sialadenitis. Intraductal irrigation was then performed on the parotid gland on the side of the complaint. The irrigation procedure was conducted in the same manner as the sialography procedure, except that saline was used as the filling solution. Symptom severity was evaluated with a numerical rating scale (NRS) at the initial visit and a month after the irrigation.
Pathologic conditions of the salivary gland may originate from various causes. In general, salivary gland pathology can be classified into the following 5 conditions: asymptomatic enlargement associated with systemic disease, obstructive diseases, inflammatory diseases, traumatic disorders, and neoplasms or cysts.1
Although the etiology of the obstructive and inflammatory disease of the major salivary glands is still unclear, the salivary gland obstruction can originate from a sialolith or a microlith. A sialolith can be observed and localized with occlusal radiography or cone-beam computed tomography.23 Bacterial debris, precipitation of salivary proteins, and foreign bodies may be invisible causes of obstruction and are referred to as microliths.4 They precipitate in ducts and intraglandular ductules, and may obstruct salivation, followed by inflammation in the duct and the gland. This inflammation can cause local stenosis of the ductal structure, increasing saliva retention. This situation worsens the internal inflammation of the gland and/or duct, and patients feel discomfort because of the frequent swelling of the gland area. When this condition moves into the chronic stage, duct deformation is observed because of an increase or decrease in the duct width; further, the gland parenchyma degenerates. These conditions of the salivary gland can be diagnosed with sialography.5
When a patient experiences discomfort because a duct is obstructed by a sialolith, surgical removal of the sialolith can immediately resolve the symptoms. However, when the patient experiences discomfort because of duct obstruction with plaque or microliths that are invisible in radiographic images or because of a permanent structural change with chronic inflammation, the symptoms are difficult to relieve. Microliths, which are invisible in radiographic imaging, are difficult to remove, and permanent structural changes, particularly constrictions, exacerbate the symptoms by preventing the saliva from flushing out the plaque and the microlith. Patients may take medication to control the symptoms until the gland completely atrophies, losing its function. When the discomfort is severe, the gland and the duct can be removed surgically.6 However, the surgical complication of neuropathy may occur because of damage to the facial nerve that passes between the internal lobe and the external lobe of the parotid gland. The submandibular gland is located deep in the mouth floor and is surrounded by vessels. Thus, surgical removal of this gland may cause hematoma, which is life-threatening if it obstructs the airway.7 For patients who do not want to undergo surgery, salivary gland and duct irrigation can be a safe, conservative treatment option.8910
Sialography is known as a tool for salivary gland diagnosis. Previously, several studies were conducted on its therapeutic effects and its utility as a diagnostic tool.511 Eisdenbud and Cranin5 reported that patients with obstructive sialadenitis in the parotid and submandibular glands showed a favorable response after sialography. Among patients with obstructive sialadenitis, 80% experienced reduced pain and swelling. Based on this outcome, some studies on the effect of intraglandular irrigation have been conducted.910 In a recent study of obstructive sialadenitis patients, intraglandular irrigation was reported to result in symptom improvement.10 However, recent studies were mostly performed under the guidance of sialoendoscopy. It is difficult to find in the literature a study that reports the effectiveness of this type of irrigation when performed without complex equipment. The procedure for intraductal irrigation with a saline solution is basically similar to that of sialography, which is frequently done in departments of oral and maxillofacial radiology. Thus, intraductal irrigation can be safely applied to cases of obstructive sialadenitis and sialodochitis without the aid of sialoendoscopy.
This report introduces a specific irrigation procedure for the parotid gland and discusses the indications for the procedure and the prognosis of the patients.
Figure 1 shows the devices used for intraductal irrigation. The procedure for intraductal irrigation is the same as that of sialography performed at Seoul National University Dental Hospital. Intraductal irrigation in our department is usually performed as follows, and each step can be omitted or repeated according to the patient's condition. Step 1 is orifice exploration, in which the orifice of the salivary gland is explored with a periodontal probe while inducing salivation by gently massaging the preauricular area. Step 2 is duct dilation, in which the duct is enlarged with adequately sized lacrimal probes ranging from #0000 to #0. Step 3 is the filling phase, in which the duct is first cannulated with a scalp vein set (23 G×13/4 in) (JMS Co. Ltd., Tokyo, Japan) after the needle tip is cut off and made blunt with dental Kelly forceps, and then normal saline is gradually added into the duct and the gland through a scalp needle using a 5-mL syringe. Step 4 is the evacuation phase. In this step, after removal of the scalp vein set, the gland area is massaged to discharge the saline. If the discharged saline includes whitish or yellowish plaque, the entire procedure is repeated.
A 50-year-old female patient came to the hospital complaining of pain in the preauricular to mandibular angle region when she ate sour or firm food. The initial symptom had been detected 10 years previously and the pain became intolerable 2 months prior. This subjective symptom was evaluated with the numeric rating scale (NRS) developed by Hawker et al.12 The NRS is a method for measuring pain in adult patients. The patient's medical record revealed only a history of fallopian tubal surgery. Sialography was performed on both parotid glands, and both glands were diagnosed as having sialodochitis with sialadenitis (Fig. 2). At the same time, oral antibiotics were prescribed to relieve the acute symptoms. After 2 months, intraductal irrigation of both parotid glands was performed. Irrigation was performed 3 times consecutively until the saline discharge had no whitish plaque. After a month, the symptoms were re-evaluated with NRS.
A 53-year-old female patient visited Seoul National University Dental Hospital complaining of pain in the left preauricular region during a meal. She had no systemic disease other than hypertension. The onset of this symptom was 3 years ago, and sialography on the left parotid gland was performed at that time. Based on sialography, sialodochitis with sialadenitis on the left parotid gland was diagnosed (Fig. 3). The patient reported symptom relief upon the use of antibiotics and anti-inflammatory medication. However, recently, she frequently experienced pain and swelling in the left preauricular area. The symptoms were evaluated with NRS. Based on the previous sialography image, intraductal irrigation was performed on the left parotid gland. The irrigation was performed 4 times at 1-month intervals.
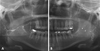
Patient 1 showed an abnormal Stensen duct on both sides. The right parotid gland showed intraglandular ductal dilatation, while the left side showed ductal dilatation as well as punctated acinar fillings. Numerous small radiolucent filling defects were observed on the wall of both Stensen ducts (Fig. 3). The initial NRS was 10 before sialography. A month after sialography, the patient noticed that the symptom severity had decreased and the NRS was reduced to 6; she then underwent irrigation of both parotid glands. A month after this irrigation, she reported that the frequency of swelling had substantially reduced and the discomfort had disappeared. The NRS decreased to 0 at that point.
The sialography of patient 2 revealed that the diameter of the duct was not even, with local dilatation and stricture (Fig. 2). Her initial symptom of parotid gland swelling with an NRS value of 4-5 gradually improved to an NRS of 1 at her fourth visit. A month after the first irrigation, the patient reported reduced discomfort and a reduced frequency of swelling. A month after the second irrigation, pain was relieved but the preauricular area still bothered her at times. Then, 4 months after the initial irrigation, she stated that her salivation had improved.
The present report introduced an intraductal irrigation procedure to treat parotid glands in a chronic inflammatory state with a mucus plug, strictures, or stenosis. This condition can be confirmed with sialography. In this study, the patients showed an abnormal change in the duct structure, the so-called sausage-string shape. Further, 1 patient showed radiolucent foci on the ductal wall, which were thought to be microliths or plaque. For patients with obstructive and inflammatory disease of a major salivary gland, removal of intraluminal causes such as microliths or the mucosal plug can be an effective treatment option.13 For this procedure, endoscopy is the common method of choice. With an endoscope, dilatation of the constricted duct using the angioplasty balloon procedure has also been performed.131415 There are several practical challenges with using an endoscope. Mainly, the orifice and the duct of the salivary gland should be at least 1.2-1.3 mm for the endoscope to be inserted safely.16 However, the size of the orifice, particularly for the submandibular gland, may be smaller than 1.2 mm within the range of normal anatomic variations. In order to introduce an endoscope into the duct, the ostium is usually surgically widened.1415 Further, for a patient with chronic sialodochitis, the thickness of the constricted duct may be less than 1.2 mm. Initial failure when introducing an endoscope into the duct or late intraoperative failure has been observed in approximately 18% of salivary gland endoscopies.14 Complications of the endoscopic approach to the salivary glands include avulsion of the duct, minor ductal tears, and superficial mucosal necrosis at the injection site.15 The high equipment cost also adversely affects the potential widespread use of this procedure by clinicians.
A previous study has reported several explanations for the therapeutic effect of intraglandular irrigation with saline.10 Due to the increased protein concentration in the duct, proteins may coagulate and obstruct the small intraglandular ductules. This increases the inflammatory response in the gland. The precipitated protein also contributes to bacterial proliferation ascending from the intraoral cavity, which could cause chronic sialadenitis and sialodochitis. Intraglandular irrigation of the salivary gland may reduce the concentration of these proteins and microbes.10 In the present study, patient 2 showed a discharge of whitish plaque, different from mucopus, which is thought to be caused by proteins and bacterial debris. Further, ductal cannulation with a lacrimal probe as well as a saline flush may help to widen the strictures of the duct and the ductules, as in the case of endoscopic dilation with an angioplastic balloon.1314 This may help the microliths and the mucus plug to discharge freely.10
In this paper, the method of irrigation with normal saline was introduced with practical examples of real-world cases. In both patients, the subjective severity of the symptoms diminished after irrigation. The procedure was performed conservatively, without damaging the anatomical structures. Moreover, no post-treatment complications were detected. The procedure was simple and mostly the same as that of sialography. It is a simple and safe treatment option for patients with obstructive and inflammatory disease of the salivary gland.
A major limitation of this report is that patients took medication at their initial visit, and this may have contributed to symptom alleviation. Further, the number of patients considered is small and the follow-up period was short. A further study of intraductal irrigation of the salivary gland is required, with a large pool of patients undergoing long-term follow-up.
In conclusion, intraductal irrigation is a simple and safe treatment option for patients with obstructive and inflammatory disease of the salivary gland, and can be performed as an interventional treatment in departments of oral and maxillofacial radiology. It is a conservative treatment option with fewer complications than surgical resection of the gland, and is cost-effective compared to sialendoscopy. Further research with more clinical cases should be evaluated to ascertain the effectiveness of this treatment.
Figures and Tables
Fig. 1
Instruments used for salivary duct and gland irrigation. From the right, a dental mirror, a periodontal probe, a scalp vein set connected to a 5-mL syringe, and a lacrimal probe (size: #0000 to #0).

Fig. 2
Sialography of both parotid glands of patient 1 shows sialodochitis with sialadenitis of both glands. A. The right Stensen duct and intraglandular ductule show local dilatation with constriction. B. The hilum of the left parotid gland is enlarged, and punctated acinar fillings are observed. Tiny filling defects in the main duct of both sides were observed and assumed to be microliths (arrowheads).
References
1. Epker BN. Obstructive and inflammatory diseases of the major salivary glands. Oral Surg Oral Med Oral Pathol. 1972; 33:2–27.

2. Kim JH, Aoki EM, Cortes AR, Abdala-Júnior R, Asaumi J, Arita ES. Comparison of the diagnostic performance of panoramic and occlusal radiographs in detecting submandibular sialoliths. Imaging Sci Dent. 2016; 46:87–92.

3. Abdel-Wahed N, Amer ME, Abo-Taleb NS. Assessment of the role of cone beam computed sialography in diagnosing salivary gland lesions. Imaging Sci Dent. 2013; 43:17–23.

4. Triantafyllou A, Harrison JD, Garrett JR. Analytical ultrastructural investigation of microliths in salivary glands of cat. Histochem J. 1993; 25:183–190.

5. Eisenbud L, Cranin N. The role of sialography in the diagnosis and therapy of chronic obstructive sialadenitis. Oral Surg Oral Med Oral Pathol. 1963; 16:1181–1199.

6. Bates D, O'Brien CJ, Tikaram K, Painter DM. Parotid and submandibular sialadenitis treated by salivary gland excision. Aust N Z J Surg. 1998; 68:120–124.

7. Hsu AK, Kutler DI. Indications, techniques and complications of major salivary gland extirpation. Oral Maxillofac Surg Clin North Am. 2009; 21:313–321.

8. Izumi M, Eguchi K, Nakamura H, Takagi Y, Kawabe Y, Nakamura T. Corticosteroid irrigation of parotid gland for treatment of xerostomia in patients with Sjögren's syndrome. Ann Rheum Dis. 1998; 57:464–469.
9. Antoniades D, Harrison JD, Epivatianos A, Papanayotou P. Treatment of chronic sialadenitis by intraductal penicillin or saline. J Oral Maxillofac Surg. 2004; 62:431–434.

10. Pace CG, Hwang KG, Papadaki M, Troulis MJ. Interventional sialoendoscopy for treatment of obstructive sialadenitis. J Oral Maxillofac Surg. 2014; 72:2157–2166.

11. Drage NA, Brown JE, Wilson RF. Pain and swelling after sialography: is it a significant problem? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000; 90:385–388.

12. Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken). 2011; 63:Suppl 11. S240–S252.
13. Buckenham TM, Page JE, Jeddy T. Technical report: interventional sialography - balloon dilatation of a Stensen's duct stricture using digital subtraction sialography. Clin Radiol. 1992; 45:34.

14. Choi JS, Lim JY, Kim YM. Sialendoscopy. Korean J Otorhinolaryngol-Head Neck Surg. 2011; 54:819–827.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download