Abstract
Fusion is an abnormality of tooth development defined as the union of two developing dental germs, resulting in a single large dental structure. This irregular tooth morphology is associated with a high predisposition to dental caries and periodontal diseases. As a result of recurring inflammatory periodontal processes, disorders such as periodontal pocket, pericoronitis, and paradental cysts may develop. A rare mandibular anatomic variation is the retromolar canal, which is very significant for surgical procedures. The fusion of a paramolar and mandibular third molar associated with a paradental cyst co-occurring with the presence of a retromolar canal is rare, and the aim of the present study is to describe the evaluation of this anatomical configuration using cone-beam computed tomography.
Fusion is defined as the union of two contiguous dental germs occurring in any stage of odontogenesis.1 This union may develop at the crown level (enamel) or at the crown and root level (enamel and dentin).2 Nonetheless, the pulp chambers and the pulp canals are either unified or separated.1 This anatomic irregularity is commonly observed in the primary dentition, particularly in the anterior region of the mouth.3 It is usually seen in the maxillary arch, and rarely occurs in the posterior mandible.4 The etiology of fusion is still unclear; however, it has been suggested that the pressure or physical forces that provide close contact between two adjacent dental follicles may cause the follicles to fuse before calcification.5 The main periodontal problem in cases of fusion is the presence of deep fissures or grooves that extend subgingivally on the union between the teeth involved. These fissures may allow the accumulation of bacterial plaque, leading to dental caries and periodontal diseases in this area.1
Due to recurrent periodontal problems, the jaws may exhibit cysts, such as paradental cysts. This type of cyst has been described as an inflammatory cyst that develops on the cervical margin of a vital tooth due to an inflammatory process in the periodontal pocket.6 The etiology of these cysts has been proposed to involve the inflammatory proliferation of the epithelial cell rests of Malassez or reduced enamel epithelium.5
An unusual morphological variation of the mandible is the retromolar canal, which permits the passage of the vascular and nerve bundles of the pulp and periodontium of mandibular molar teeth.7 This canal branches off from the mandibular canal behind the last molar tooth and passes through the retromolar fossa via the retromolar foramen. 8 However, the content of retromolar canals has not been conclusively established.7 The lack of information on this subject may be related to complications involving local anesthesia9 and surgical nerve damage during third molar surgery in the retromolar region.8
Panoramic radiography plays a fundamental role in providing data on the oral and maxillofacial region.10 Nevertheless, panoramic radiographs and other two-dimensional radiographs fail to show the buccolingual aspect and cross-sectional slices, which are important for presurgical assessments.11 Cone-beam computed tomography (CBCT) provides high-contrast three-dimensional images of maxillofacial structures that help to identify the definitive diagnosis and develop a treatment plan based on images in all specialties within dentistry.12
The aim of the present report was to describe the use of CBCT to visualize the fusion of the mandibular third molar and a supernumerary tooth in relation to a paradental cyst and in the presence of a retromolar canal in the same region.
A 27-year-old male patient with an unremarkable medical history was referred to the Department of Oral and Maxillofacial Radiology with a complaint of pain in the region of the lower right molar teeth.
An intraoral examination revealed irregular morphology of the mandibular permanent third molar. This morphology suggested the presence of the union of an extra cusp on the lingual aspect of a wisdom tooth. This union led to the development of a groove formation that caused periodontal problems. The gingiva around the right mandibular third molar appeared to be reddish in color, with loss of stippling and an inflamed appearance (Fig. 1A).
A panoramic radiograph indicated the fusion of a supernumerary tooth with the permanent third molar and the presence of a dilated follicular space associated with this abnormal formation. This irregular enlargement exhibited a sharply delineated area of radiolucency around the fused supernumerary tooth (Fig. 1B). However, the panoramic radiograph was not sufficient to visualize this dental formation and its surrounding tissues because it only provided information in the mesiodistal plane. With the consent of the patient, a CBCT image was taken to observe the abovementioned teeth, the periradicular lesion, and the relationship thereof with the peripheral structures.
The CBCT scans of the right side of the mandible in all orthogonal planes showed a fused supernumerary molar on the lingual aspect of the third molar (Fig. 2). Around the periradicular region of these malformed teeth, a cystic lesion was identified in the axial, coronal, and sagittal planes (Figs. 2A-D). Additionally, an axial section revealed perforations of this cystic lesion on the buccal and lingual borders of the compact bone (Fig. 2E). Furthermore, the presence of a retromolar canal was incidentally identified on a sagittal CBCT image (Fig. 2F).
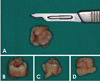
A treatment plan was developed, including the extraction of the fused teeth and the cystic lesion. The fused teeth were extracted with an inferior alveolar nerve block (Fig. 3); subsequently, the cystic lesion was curetted and sent to the Department of Pathology for a definitive diagnosis. Based on pathological and histological examinations, it was identified as a paradental cyst (Fig. 4).
Fusion is a developmental dental anomaly caused by the union of two normal dental germs or the germ of a supernumerary tooth with that of a normal tooth.13 The incidence of fusion is similar in males and females,14 and it is more frequently observed in the deciduous dentition, especially in the anterior region of the jaws. However, supernumerary paramolars are rare abnormalities of the maxillofacial structures that are more common in the maxilla than in the mandible.15 Therefore, fusion of the molars or the involvement of a mandibular paramolar, as in the present case, is uncommon.3
The affected teeth are unaesthetic due to their abnormal morphology.1 This malformation is also related to complex tooth morphology and pulpal anatomy, and the tooth position can additionally cause difficulty in rubber dam placement.4 For these reasons, surgical therapy may be preferable to endodontic treatment in most cases.14 Fused teeth may also have deep fissures or grooves that may lead to caries and periodontal diseases, such as pericoronitis and paradental cysts.1617
Paradental cysts were first described as an "inflammatory collateral cyst" by Main.18 The pathogenesis of inflammatory paradental cysts remains unclear. However, it has been suggested by Craig19 that chronic inflammation in the superficial part of the periodontium of an erupting tooth stimulates the odontogenic epithelium in the region to proliferate. The differential diagnosis includes radicular cysts, lateral periodontal cysts, dental follicles, and dentigerous cysts.20 The frequency of such lesions has been reported to range from 3% to 5%.21 The occurrence of a paradental cyst along with a supernumerary tooth, as in our case, is extremely rare. Moreover, we were not able to find any previous reports describing the presence of a retromolar canal together with a paradental cyst with fused teeth, as was observed in our case.
The retromolar canal is a rare anatomic variation found in the retromolar triangle, a small triangular region posterior to the third molar tooth in the mandible.22 The neurovascular content of the retromolar canal is very important for surgical procedures involving the retromolar area.7 Knowledge of this anatomical variation may prevent complications in anesthesia and surgical procedures in this area and serve as an anatomical landmark for ethnic identification.8
Ossenberg23 stated that the retromolar canal is an anatomic variant that normally arises from the mandibular canal behind the third molar and travels anterosuperiorly to the retromolar foramen, which is located in the retromolar fossa. Carter and Keen24 demonstrated that a neural branch to the mandibular molars arises from the inferior alveolar nerve or from the retromolar branch that travels through the retromolar canal. However, Jablonski et al.25 have shown an aberrant buccal nerve originating from the inferior alveolar nerve within the ramus of the mandible, traversing through the retromolar canal, emerging through the retromolar foramen, and then passing forward and upward to penetrate the buccinator muscle.
The incidence of retromolar canals has been found to range from 6.1% to 72% in CBCT studies among different populations.723262728 Naitoh et al.29 investigated the retromolar canal as a subtype of the bifid mandibular canal using clinical CBCT images (voxel size, 0.155 mm) and observed the retromolar canal at a frequency of 25.4% per mandible and 13.5% per side. Patil et al.30 found an incidence of 65%, which was higher than the incidence rates reported in previous CBCT studies.83132 Von Arx et al.8 studied 121 sides in 100 patients (100 unilateral and 21 bilateral cases). A total of 31 retromolar canals were identified with CBCT (25.6%). Only seven of these canals were also seen on the corresponding panoramic radiographs. Therefore, retromolar canals are more visible in CBCT images than in panoramic radiographs. Patil et al.30 reported no differences in the occurrence of retromolar canals according to sex and the side of the mandible.
CBCT technology has made a substantial impact on maxillofacial imaging and has been used in several areas of dentistry because it shows three-dimensional images of dental structures in addition to providing clear structural images with high resolution.12 It has enabled the better visualization of the morphology of malformations and anatomic structures.29 Recently, CBCT helped us to detect the presence of a retromolar canal and a paradental cyst with fused teeth. When three-dimensional images are required for diagnosis or treatment planning, two-dimensional conventional radiographs may be unsatisfactory. Moreover, in comparison with conventional computed tomography, CBCT has the advantage of lower radiation exposure.33 Additionally, CBCT is more useful in the accurate identification of anatomical variations.34 Additionally, CBCT machines are convenient for routine investigations in the dental office.
In conclusion, fusion of the teeth is rarely seen in the mandibular molars, and to the best of our knowledge, this case report is the first in the literature to describe fusion between a mandibular third molar and a paramolar associated with a paradental cyst and the presence of a retromolar canal. An accurate assessment of these morphological and pathological formations was carried out using CBCT.
Figures and Tables
Fig. 1
An intraoral examination shows an extra cusp on the lingual aspect of the third molar tooth and inflamed gingiva around the abnormal tooth formation. B. A cropped panoramic radiograph exhibits an extra tooth in close association with the mandibular third molar and a sharply delineated radiolucent lesion around the apical area in relation to the same molar.
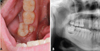
Fig. 2
Cone-beam tomographic images of the right mandibular third molar region demonstrate the fusion of a supernumerary molar on the lingual aspect of the third molar on the axial (A and B), coronal (C), and sagittal (D) planes. B-D. A cystic lesion can be identified around the fused teeth (arrows). E. The axial image shows the lesion in relation to the fused teeth. F. The retromolar canal is observed behind the fused teeth in the sagittal view (arrow).

References
1. Nunes E, de Moraes IG, de Novaes PM, de Sousa SM. Bilateral fusion of mandibular second molars with supernumerary teeth: case report. Braz Dent J. 2002; 13:137–141.

2. Neves AA, Neves ML, Farinhas JA. Bilateral connation of permanent mandibular incisors: a case report. Int J Paediatr Dent. 2002; 12:61–65.

3. Levitas TC. Gemination, fusion, twinning and concrescence. ASDC J Dent Child. 1965; 32:93–100.
4. Muthukumar RS, Arunkumar S, Sadasiva K. Bilateral fusion of mandibular second premolar and supernumerary tooth: a rare case report. J Oral Maxillofac Pathol. 2012; 16:128–130.

5. Prakash AR, Reddy PS, Rajanikanth M. Paradental cyst associated with supernumerary tooth fused with third molar: a rare case report. J Oral Maxillofac Pathol. 2012; 16:131–133.

6. Mufeed A, Chatra L, Shenai P. Diagnostic features of the paradental cyst and report of a case. Dentomaxillofac Radiol. 2009; 38:125–126.

7. Bilecenoglu B, Tuncer N. Clinical and anatomical study of retromolar foramen and canal. J Oral Maxillofac Surg. 2006; 64:1493–1497.

8. von Arx T, Hänni A, Sendi P, Buser D, Bornstein MM. Radiographic study of the mandibular retromolar canal: an anatomic structure with clinical importance. J Endod. 2011; 37:1630–1635.

9. Rossi AC, Freire AR, Prado GB, Prado FB, Botacin PR, Caria PH. Incidence of retromolar foramen in human mandibles: ethnic and clinical aspects. Int J Morphol. 2012; 30:1074–1078.

10. Pires CA, Bissada NF, Becker JJ, Kanawati A, Landers MA. Mandibular incisive canal: cone beam computed tomography. Clin Implant Dent Relat Res. 2012; 14:67–73.

11. Watson RM, Davis DM, Forman GH, Coward T. Considerations in design and fabrication of maxillary implant-supported prostheses. Int J Prosthodont. 1991; 4:232–239.
12. Neves FS, Souza TC, Almeida SM, Haiter-Neto F, Freitas DQ, Bóscolo FN. Correlation of panoramic radiography and cone beam CT findings in the assessment of the relationship between impacted mandibular third molars and the mandibular canal. Dentomaxillofac Radiol. 2012; 41:553–557.

13. Chen HS, Huang YL. Fusion of third and fourth mandibular molars? Oral Surg Oral Med Oral Pathol. 1992; 73:767.

14. Järvinen S, Lehtinen L. Supernumerary and congenitally missing primary teeth in Finnish children. An epidemiologic study. Acta Odontol Scand. 1980; 39:83–86.
15. Parolia A, Kundabala M, Dahal M, Mohan M, Thomas MS. Management of supernumerary teeth. J Conserv Dent. 2011; 14:221–224.

16. Ghoddusi J, Zarei M, Jafarzadeh H. Endodontic treatment of a supernumerary tooth fused to a mandibular second molar: a case report. J Oral Sci. 2006; 48:39–41.

17. Indra R, Srinivasan MR, Farzana H, Karthikeyan K. Endodontic management of a fused maxillary lateral incisor with a supernumerary tooth: a case report. J Endod. 2006; 32:1217–1219.

18. Main DM. Epithelial jaw cysts: a clinicopathological reappraisal. Br J Oral Surg. 1970; 8:114–125.

19. Craig GT. The paradental cyst. A specific inflammatory odontogenic cyst. Br Dent J. 1976; 141:9–14.

20. de Sousa SO, Corrêa L, Deboni MC, de Araújo VC. Clinicopathologic features of 54 cases of paradental cyst. Quintessence Int. 2001; 32:737–741.
21. Ackermann G, Cohen MA, Altini M. The paradental cyst: a clinicopathologic study of 50 cases. Oral Surg Oral Med Oral Pathol. 1987; 64:308–312.

22. Gadbail AR, Mankar Gadbail MP, Hande A, Chaudhary MS, Gondivkar SM, Korde S, et al. Tumor angiogenesis: role in locally aggressive biological behavior of ameloblastoma and keratocystic odontogenic tumor. Head Neck. 2013; 35:329–334.

24. Carter RB, Keen EN. The intramandibular course of the inferior alveolar nerve. J Anat. 1971; 108:433–440.
25. Jablonski NG, Cheng CM, Cheng LC, Cheung HM. Unusual origins of the buccal and mylohyoid nerves. Oral Surg Oral Med Oral Pathol. 1985; 60:487–488.

26. Ikeda K, Ho KC, Nowicki BH, Haughton VM. Multiplanar MR and anatomic study of the mandibular canal. AJNR Am J Neuroradiol. 1996; 17:579–584.
27. Pyle MA, Jasinevicius TR, Lalumandier JA, Kohrs KJ, Sawyer DR. Prevalence and implications of accessory retromolar foramina in clinical dentistry. Gen Dent. 1999; 47:500–505.
28. Sawyer DR, Kiely ML. Retromolar foramen: a mandibular variant important to dentistry. Ann Dent. 1991; 50:16–18.
29. Naitoh M, Hiraiwa Y, Aimiya H, Ariji E. Observation of bifid mandibular canal using cone-beam computerized tomography. Int J Oral Maxillofac Implants. 2009; 24:155–159.
30. Patil S, Matsuda Y, Nakajima K, Araki K, Okano T. Retromolar canals as observed on cone-beam computed tomography: their incidence, course, and characteristics. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013; 115:692–699.

31. Kawai T, Asaumi R, Sato I, Kumazawa Y, Yosue T. Observation of the retromolar foramen and canal of the mandible: a CBCT and macroscopic study. Oral Radiol. 2012; 28:10–14.

32. Lizio G, Pelliccioni GA, Ghigi G, Fanelli A, Marchetti C. Radiographic assessment of the mandibular retromolar canal using cone-beam computed tomography. Acta Odontol Scand. 2013; 71:650–655.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download