Abstract
Mönckeberg sclerosis is a disease of unknown etiology, characterized by dystrophic calcification within the arterial tunica media of the lower extremities leading to reduced arterial compliance. Medial calcinosis does not obstruct the lumina of the arteries, and therefore does not lead to symptoms or signs of limb or organ ischemia. Mönckeberg sclerosis most commonly occurs in aged and diabetic individuals and in patients on dialysis. Mönckeberg arteriosclerosis is frequently observed in the visceral arteries, and it can occur in the head and neck region as well. This report describes a remarkable case of Mönckeberg arteriosclerosis in the head and neck region as detected on dental imaging studies. To the best of our knowledge, this is the first case that has been reported in which this condition presented in the facial vasculature. The aim of this report was to define the radiographic characteristics of Mönckeberg arteriosclerosis in an effort to assist health care providers in diagnosing and managing this condition.
Vascular calcification is a common consequence of aging and is more frequent in patients with diabetes, dyslipidemia, genetic diseases, and diseases involving disturbances of calcium metabolism.1 Vascular calcification is a result of the deposition of hydroxyapatite with a high degree of crystallization in the extracellular matrix and in cells of the media or intima of the arterial wall.2 Intimal calcification is associated with atherosclerosis, which is characterized by lipid accumulation, inflammation, fibrosis, and the development of focal plaques.34 Medial calcific deposits (Mönckeberg arteriosclerosis) were first described by Mönckeberg in 1903 as a calcification of the tunica media of the medium and small muscular arteries of the lower limbs and, less frequently, in the visceral arteries or coronary arteries. The asymptomatic form of Mönckeberg arteriosclerosis is a degenerative and apparently non-inflammatory disease and is not associated with narrowing of the lumen or intimal disruption.5678
The exact etiology of this condition is not well understood, although it has been found to be related to glucose intolerance, aging, male gender, autonomic neuropathy, osteoporosis, and chronic renal failure.6
This type of calcification is most common in diabetics.79 Autonomic dysfunction from diabetic neuropathy is assumed to be responsible for the occurrence of Mönckeberg arteriosclerosis in diabetic patients.10
Most patients with medial calcinosis are asymptomatic, and it is usually an incidental finding, identified either clinically or on panoramic or periapical radiographs. Clinically, the calcified vessel is described as a "pipe-stem" artery, which is visible on plain radiographs as "rail-tracking" of the vessel.511 It is important for the dental practitioner to recognize this feature, even when it appears subtly on a panoramic radiograph, in order to ensure prompt and appropriate follow-up.
Mönckeberg arteriosclerosis is most commonly found in the extremities.2 However, this condition can occur in the head and neck region. This report presents a case of Mönckeberg arteriosclerosis in the head and neck region as seen on panoramic and bitewing intraoral radiographs.
A 65-year-old man with a medical history of stage III nasopharyngeal cancer, end-stage renal disease treated with dialysis, hyperthyroidism, type 2 diabetes mellitus, hypertension, atrial fibrillation, and secondary hyperparathyroidism presented at the Oral Medicine Clinic of the College of Dentistry, University of Florida for dental evaluation prior to the start of radiotherapy. Intraoral radiographs were taken using a CS2000 intraoral X-ray system (Carestream Dental LLC, Atlanta, GA, USA) with #2 Soredex Optime (Soredex, Charlotte, NC, USA) photo-stimulable phosphor (PSP) sensors at 70 kVp, 7 mA, and a 0.142-second exposure time, using a standard bitewing technique. A panoramic image was obtained using an Orthopantomograph ® OP100 D digital panoramic X-ray unit (Instrumentarium Dental, Tuusula, Finland) with exposure factors of 70 kVp with 12 mA for 17.6 seconds. The images were interpreted by a board-certified oral and maxillofacial radiologist.
The panoramic and bitewing radiographs revealed multiple tortuous vascular calcifications in the soft tissue of the neck and cheek bilaterally, with a dense "rail track" pattern of linear calcifications within the facial artery. Based upon the radiographic presentation and the patient's known medical history, Mönckeberg arteriosclerosis was the initial impression. Multiple radiopaque entities were also noted in the soft tissue of the neck, more on the left than on the right, consistent with a diagnosis of carotid atherosclerosis (Figs. 1 and 2).
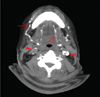
Positron emission tomography/computed tomography (PET/CT) scans were performed using a Philips Gemini GXL 16 PET/CT system with 5 mm thickness. The acquired data were reviewed by a medical radiologist, and "pipe-stem" calcifications were observed in the bilateral, lingual, and facial arteries (Fig. 3).
Calcifications may occur in several locations in the cardiovascular system, including the intima and media of vessels. Intimal arterial calcification is associated with atherosclerosis, and vascular plaques form within the intima of the involved vessel.3 However, in Mönckeberg arteriosclerosis, the calcific deposits are located entirely within the medial layer of the arterial wall and both the internal and external elastic membranes are spared.712 In a recent study, the prevalence of Mönckeberg arteriosclerosis in the population was found to be 13.3% for males and 6.9% for females, and it is a well-recognized age-related phenomenon.1112
Medial artery calcification can lead to vascular stiffness, resulting in increased vascular resistance, reduced compliance of the artery, and an inability to properly vasodilate in the setting of increased stress.13 Medial calcinosis contributes to significant adverse cardiovascular outcomes in patients with chronic kidney disease and diabetes, where higher levels of medial artery calcification are a risk factor for amputation.14 The affected artery may not demonstrate evidence of a pulse.
The exact pathogenic mechanism of medial calcinosis is not well understood. However, degenerative processes leading to the apoptosis or necrosis of medial smooth muscle cells and osteogenic processes leading to formation of bone-like structures are two distinct pathologic mechanisms that have been suggested for Mönckeberg arteriosclerosis.15 Meema et al.8 have suggested the possibility that two clinically and histologically different types of medial calcifications may exist. The first type is a benign, slowly progressive, essentially asymptomatic form with thin medial calcifications and little or no narrowing of the arterial lumen. This condition does not lead to symptoms or signs of limb or organ ischemia. In contrast, the second type is defined as a malignant, rapidly progressive form, in which massive and extensive medial calcifications may displace the internal elastica toward the lumen, causing luminal narrowing.78
Mönckeberg initially described medial calcinosis as primarily affecting the arteries of the lower limbs, and occasionally affecting the peripheral arteries of the upper extremities. However, the process rarely affects the intraabdominal arteries, with the exception of the renal and splenic arteries.7 Some reports in the literature have described Mönckeberg arteriosclerosis. In 1977, Lachman et al.7 described the involvement of coronary, peripheral, and visceral arteries with Mönckeberg calcification. A case of Mönckeberg arteriosclerosis involving the aorta, pelvic, and lower limb arteries was reported by Lanzer in 1998.16 The nonvascular involvement of soft tissue (pharynx and larynx) with Mönckeberg sclerosis was reported by Couri et al.6
In this report, we described a diabetic patient with end-stage renal disease on dialysis, who had advanced and previously undiagnosed Mönckeberg medial calcinosis of the facial and lingual arteries.
Knowledge of the radiographic appearance of this calcification is clinically useful in developing a differential diagnosis. The proper interpretation of radiographic images presupposes a thorough knowledge of the anatomy, distribution, number, size, and shape of the calcifications.
Mönckeberg medial calcinosis is usually discovered incidentally upon imaging of the maxillofacial region. The calcified vessel appears as a parallel pair of thin, radiopaque lines that may have a straight course or a tortuous path, showing a pattern of blood vessels that looks like railroad tracks.511 Carotid artery calcifications and phleboliths are calcifications that can be seen in the same location on a panoramic radiograph. Carotid artery calcifications radiographically appear as curvilinear irregular parallel radiopacities in the soft tissues of the neck at or below the third and fourth cervical vertebrae, and inferior and lateral to the hyoid bone.1718 Phleboliths can be seen on a panoramic radiograph as round or oval in shape with a homogeneously radiopaque center, giving phleboliths a "target" appearance.19
Mönckeberg sclerosis is listed among the primary diseases of vessels that can be visualized on panoramic radiographs. To the best of our knowledge, our report describes the first known case of medial calcification in the facial artery on the panoramic radiograph of a diabetic patient with end-stage renal disease.
Soft tissue calcifications in the maxillofacial area are relatively common and can occur as the result of physiologic or pathologic mineralization, and generally correspond to radiographic findings in routine examinations, such as panoramic radiographs. A comprehensive review and thorough interpretation of all conventional and routine dental radiographs, especially beyond the region of interest, is necessary, and dental practitioners should be aware of the various calcified structures seen on panoramic radiographs, especially those associated with systemic diseases. A proper knowledge of radiographic features, however subtle they may be, assists the clinician in following up and further managing the patient, including appropriate referrals.
Figures and Tables
Fig. 1
A. A bitewing radiograph on the right premolar area shows Mönckeberg arteriosclerosis of facial artery. Railroad track pattern calcification within the blood vessel is noted. B. A bitewing radiograph on the left premolar shows Mönckeberg arteriosclerosis of facial artery. Railroad track pattern calcification within the blood vessel is noted.

Fig. 2
Panoramic radiograph displays Mönckeberg arteriosclerosis of facial artery. Extensive tortuous railroad track-type calcification in the facial artery is noted in the soft tissue of the neck and cheek bilaterally (arrows). Bilateral calcifications associated with the carotid arteries superimposed on the soft tissue of the neck (circles).

Acknowledgements
Dr. Pamela Sandow, Oral Medicine; Drs. Manik Bedi, Franci Stavropoulos, and James Ruskin, Oral and Maxillofacial Surgery, for requesting appropriate imaging studies and providing dental care to the patient.
References
1. Amann K. Media calcification and intima calcification are distinct entities in chronic kidney disease. Clin J Am Soc Nephrol. 2008; 3:1599–1605.
2. Lanzer P, Boehm M, Sorribas V, Thiriet M, Janzen J, Zeller T, et al. Medial vascular calcification revisited: review and perspectives. Eur Heart J. 2014; 35:1515–1525.

3. O'Neill WC, Lomashvili KA. Recent progress in the treatment of vascular calcification. Kidney Int. 2010; 78:1232–1239.
4. Mackey RH, Venkitachalam L, Sutton-Tyrrell K. Calcifications, arterial stiffness and atherosclerosis. Adv Cardiol. 2007; 44:234–244.

5. Castling B, Bhatia S, Ahsan F. Mönckeberg's arteriosclerosis: vascular calcification complicating microvascular surgery. Int J Oral Maxillofac Surg. 2015; 44:34–36.

6. Couri CE, Da Silva GA, Martinez JA, Pereira Fde A, de Paula FJ. Mönckeberg's sclerosis - is the artery the only target of calcification? BMC Cardiovasc Disord. 2005; 5:34.

7. Lachman AS, Spray TL, Kerwin DM, Shugoll GI, Roberts WC. Medial calcinosis of Mönckeberg. A review of the problem and a description of a patient with involvement of peripheral, visceral and coronary arteries. Am J Med. 1977; 63:615–622.
8. Meema HE, Oreopoulos DG, Rapoport A. Serum magnesium level and arterial calcification in end-stage renal disease. Kidney Int. 1987; 32:388–394.

9. Lichtenfels E, Frankini AD, Becker AS, Pires VC. Mönckeberg's arteriosclerosis as a cause of lower limb critical ischemia: case report. J Vasc Bras. 2007; 6:97–100.
10. Gentile S, Bizzarro A, Marmo R, de Bellis A, Orlando C. Medial arterial calcification and diabetic neuropathy. Acta Diabetol Lat. 1990; 27:243–253.

11. Kröger K, Stang A, Kondratieva J, Moebus S, Beck E, Schmermund A, et al. Prevalence of peripheral arterial disease - results of the Heinz Nixdorf recall study. Eur J Epidemiol. 2006; 21:279–285.

12. Micheletti RG, Fishbein GA, Currier JS, Fishbein MC. Mönckeberg sclerosis revisited: a clarification of the histologic definition of Mönckeberg sclerosis. Arch Pathol Lab Med. 2008; 132:43–47.

13. Srija M, Brahmbhatt BK, Lakshminarayana G, Mathew A, Rajesh R, Kurian G, et al. Extensive vascular calcification in end stage renal disease. Amrita J Med. 2012; 8:1–44.
14. Johnson RC, Leopold JA, Loscalzo J. Vascular calcification: pathobiological mechanisms and clinical implications. Circ Res. 2006; 99:1044–1059.
15. Shioi A, Taniwaki H, Jono S, Okuno Y, Koyama H, Mori K, et al. Mönckeberg's medial sclerosis and inorganic phosphate in uremia. Am J Kidney Dis. 2001; 38:4 suppl 1. S47–S49.

16. Lanzer P. Mönckeberg media calcinosis. Z Kardiol. 1998; 87:586–593.
17. Friedlander A, Lande A. Panoramic radiographic identification of carotid arterial plaques. Oral Surg Oral Med Oral Pathol. 1981; 52:102–104.

18. Carter LC. Discrimination between calcified triticeous cartilage and calcified carotid atheroma on panoramic radiography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000; 90:108–110.

19. Kato H, Ota Y, Sasaki M, Arai T, Sekido Y, Tsukinoki K. A phlebolith in the anterior portion of the masseter muscle. Tokai J Exp Clin Med. 2012; 37:25–29.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download