Abstract
Plasma cell leukemia (PCL) is an aggressive form of multiple myeloma where there is hematogenous spread of abnormal plasma cells into the periphery. This is opposed to multiple myeloma, where the abnormal plasma cells stay in the bone marrow. PCL is more common in males than females, and is also more common in African-Americans than Caucasians. Signs and symptoms of PCL include, but are not limited to, renal insufficiency, hypercalcemia, anemia, lytic bone lesions, thrombocytopenia, hepatomegaly, and splenomegaly. Here, we discussed a case of a 71-year-old Caucasian female recently diagnosed with primary PCL with radiographic features of this disease throughout the body, with an emphasis on the maxillofacial skeleton and relevance from a dental standpoint.
Plasma cell leukemia (PCL) is considered a symptomatic version of multiple myeloma, where more than 2,000 plasma cells/µL are found in the circulatory system, plasma cells constitute more than 20% of the differential white count, and there is frequent extramedullary involvement. Symptoms include, but are not limited to, osteolytic lesions, bone pain, hypercalcemia, anemia, and renal insufficiency. PCL can either be primary, where the disease manifests without a prior diagnosis of multiple myeloma, or secondary, where the disease progresses naturally from a previous diagnosis of multiple myeloma.1234567
The causes of PCL are similar to those of multiple myeloma. A series of genetic alterations during the development of a plasma cell may lead to the uncontrolled growth of the cell. However, what induces these alterations is not fully known. Risk factors, such as age and exposure to industrial and environmental elements, are thought to play important roles. On a molecular level, PCL can be differentiated from multiple myeloma by fluorescent in situ hybridization (FISH) analysis looking for IgH translocations and chromosome 13q deletions.4
The prognosis of primary and secondary PCL is reported to be poor, with a median survival of 6-8 months. This poor prognosis is most likely a result of the biologically aggressive nature of the disease and the sequelae of multiple myeloma treatments in patients with secondary PCL.8
Magnetic resonance imaging is advised if neurologic symptoms exist, to evaluate for spinal cord compression.91011 Leptomeningeal enhancement is the most common feature seen. In the case of extramedullary myelomas, like PCL, epidural soft tissue masses are reported to be homogenously hypointense on T1-weighted images and hyperintense on T2-weighted images. Other reports of radiographic features of PCL include multi-detector computed tomography (CT) of the abdominal region exhibiting masses attached the chest wall12 or focal lesions of metastatic infiltration to the liver. Positron emission tomography/CT (PET/CT) imaging features have also been reported with increased glucose uptake in the vertebrae, ribs, and pelvis.10 However, our literature review did not reveal any exclusive studies about the oral and maxillofacial manifestations of plasma cell leukemia using common dental imaging techniques.
A 71-year-old female presented to her primary care physician in late 2014 complaining of fatigue, generalized weakness, and dyspnea upon minimal exertion. Routine laboratory values of major significance revealed hemoglobin levels of about 5.4 g/dL (reference 11-16) and her platelets count at 85,000/mL (reference 150,000-450,000/mL).
The patient was referred to the emergency department at the University of Florida Health, Shands Hospital for bone marrow biopsy and a hematology consult. Upon admission, it was noted that her serum calcium levels were elevated to 11.2 mg/dL (reference 8.5-10.2) and IgG levels were elevated to 2638 mg/dL (reference 620-1400) with a kappa:lambda ratio of 1047 : 27 (reference 3 : 1). A peripheral blood smear revealed abnormal plasma cells and a 41% distribution of lymphocytes, with 20% being plasma cells.
A radiographic bone survey also revealed degenerative changes in the spine (Fig. 1), heterogeneity in the osseous pattern of the long bones, particularly, the humeri and femurs (Fig. 2), and multiple punched-out lesions in a lateral skull view (Fig. 3). Also noteworthy is a normal right maxillary sinus with its intact borders (Fig. 4). Due to the lytic bony lesions, the patient was prescribed zoledronic acid (Zometa) and continued to receive monthly injections over a year before being switched to denosumab.
Results of the bone marrow biopsy revealed a 60% to 70% hyper cellular marrow and 50% plasma cells positive for CD138. Additionally, her FISH results revealed a loss of 13q and IgH translocations. Given all of the above information, a definitive diagnosis of plasma cell leukemia was made. The patient remained stable after multiple chemotherapy protocols over the next year and a half.
During a routine visit in early 2016, the patient presented with a mild sinus pain due to springtime allergies. The condition was treated as such. However, a month later, she presented with facial cellulitis in the right maxillary region and a “tooth fracture”. The patient was referred to oral oncology. Before her appointment, the patient had a dental visit where she was prescribed a course of amoxicillin and clavulanate potassium (Augmentin) and the facial swelling resolved. During the visit with oral oncology, a panoramic radiograph was acquired where a relative radiolucency was noted apical to the right maxillary second premolar and first molar (Fig. 5). A panoramic radiograph was also elicited from 2014 to compare findings; however, due to a technical error, the region apical to the right maxillary premolars and the floor of the maxillary sinus in that area were obscured by superimposition of the hard palate. The patient was cleared by oral oncology for endodontic treatment and referred to the Graduate Endodontics Department at the University of Florida, College of Dentistry.
Upon clinical examination, all the present teeth in the right maxillary quadrant were positive to percussion, tender to palpation, and negative to cold. Additionally, the right maxillary premolars exhibited class III mobility and the right maxillary second premolar tested non-vital to an electronic pulp test. A definitive diagnosis of pulpal necrosis and symptomatic apical periodontitis was determined for right maxillary premolars. The pre-operative periapical radiograph revealed suspected calcification of the root canal and periapical radiolucencies of the right maxillary premolars, further confirming the diagnosis (Fig. 6). Root canal treatment was started; however, the canals were inaccessible. As a result, a high-resolution non-contrast cone beam CT using a Kodak CS9300 (Carestream Dental LLC, Atlanta, GA, USA) was ordered. The volume was limited to entirety of the right maxillary sinus, the right half of the nasal fossa, the right maxillary lateral incisor at its most anterior of the dental arch, and the right maxillary first molar at its most posterior aspect of the dental arch. After acquisition, the volume was referred to the department of Oral and Maxillofacial Diagnostic Sciences for assessing the canal morphology.
The study revealed that the canals of those teeth were partially calcified. However, there were a number of incidental findings. Most notably, there was an ill-defined lytic lesion in the apical region of the right maxillary premolars causing disruptions in the floor of the right maxillary sinus and the buccal/palatal cortical plates (Fig. 7). A large mucosal thickening was also present in the sinus and the altered trabeculation in the area was consistent with the radiographic manifestations of leukemia (Fig. 8). In the absence of a medical history, these imaging features could also represent other malignant lesions such as squamous cell carcinoma, or an inflammatory process like a medication-induced osteonecrosis. However, these disease processes are not mutually exclusive and a histopathological examination and an immediate oncology consultation were recommended.
Temporary restorations were placed and the patient agreed that the questionable teeth would be extracted if they cause any further problems. An incisional biopsy from the right maxilla approximately 1.5 cm apical to the premolars with no identifiable bone was submitted to the Division of Oral Pathology for histopathologic examination. Under further analysis, a malignant neoplastic proliferation of atypical lymphocytes was found exhibiting abnormal mitosis, pleomorphism, and anaplasia. These cells were forming cords, sheets, and clusters with normal nuclei and an eosinophilic cytoplasm (Fig. 9). There was also evidence of perineural and lymphovascular spread with a sclerotic fibrous connective tissue present in the background. Overall, the histomorphology was deemed to be compatible with the patient's history of plasma cell leukemia and no additional stains were needed. The patient was referred to the Hematology-Oncology Department in the College of Medicine for hematopathologic workup.
Although osseous changes of the jawbones in leukemia are rare, the practitioner must keep them in consideration, especially in patients with a history of the disease. It is frequently localized around the periapical region of teeth and can mimic the signs and symptoms of rarefying osteitis. There may also be generalized ill-defined radiolucent lesions due to the enlarged marrow spaces and, if left untreated, these areas may start to coalesce to form one lesion. In addition, internal foci of leukemic cells (chloromas) can rarely form and behave like a localized malignant tumor13, similar to how the patient first presented to the Department of Oral and Maxillofacial Diagnostic Sciences.
However, without a thorough medical and dental history, it is hard to discern when the lesion started to form. Even though there were prior radiographs, technical errors prevented a proper comparison and evaluation of the right maxilla. This further substantiates the notion that not only is routine dental and medical care important to find early manifestations of chronic disease, but also the quality of the radiographs and choice of the imaging modality plays a pivotal role in correct diagnosis and management.
Due to the lack of a dental history, it is possible that the radiographic features presented in this case could be the result of an odontogenic infection in this area superimposed over the lymphocytic infiltration in addition to the osseous changes from long-term bisphosphonate use. As dental practitioners, we must remember to consider the patient's entire background and medical history while arriving at a differential diagnosis, as well as the existence of any comorbid conditions. Overall, the radiographic features discussed throughout this article may mimic a number of different pathologies, such as medication-induced osteonecrosis of the jaw (MIONJ). In this case, the patient is at risk due to her long-term bisphosphonate usage. Common imaging features seen in this case are osteolytic lesions that extend to the sinus floor and an altered trabecular pattern, which can also be consistent with stage 3 MIONJ. However, a hallmark of MIONJ past stage 1 is the presence of clinically exposed bone, of which none was noted. The lack of any necrotic bone in the histopathology report also rules this out. However, the case could be classified as stage 0 MIONJ due to patient's risk factors, as well as exhibiting non-specific signs and symptoms of jaw pain.14
Squamous cell carcinoma originating in the bone or in the maxillary sinus can also present with similar imaging features. Common imaging features to note would be the presence of a soft tissue mass as well as an ill-defined osteolytic process.14 Metastatic diseases from either the breast, kidney, or lung do not have hallmark pathognomic features; thus, they must be included in the differential whenever the patient has a history of carcinoma and an ill-defined osteolytic lesion.15 The radiographic features of PCL may also mimic other aggressive cancers. The possibility of concomitant pathology is also an important feature to take into consideration. The diagnosis of PCL cannot be based on radiographs alone; the clinical information, patient history, and histopathological exam must all be weighed equally when forming a differential diagnosis.
Figures and Tables
 | Fig. 1Lateral skull radiograph (Aug. 2014) depicting osseous changes in the jaws, degenerative changes in the cervical spine, and a loss of intervertebral disc space between C5 and C6. |
 | Fig. 2Conventional plain film radiographs (Aug. 2014) of the left humerus (A) and left femur (B) depicting osseous changes associated with plasma cell leukemia. |
 | Fig. 3Lateral skull radiograph (Aug. 2014) depicting multiple punched-out radiolucent lesions consistent with a myeloproliferative disorder. |
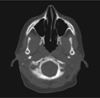 | Fig. 4Paraxial slice from a multidetector computed tomography study (Nov. 2014) depicts an intact right maxillary sinus free of gross disease. |
 | Fig. 5Dental panoramic radiograph acquired in April 2016 exhibits a relative radiolucency and loss of trabeculation apical to the maxillary right premolars. |
 | Fig. 6Periapical radiograph (Apr. 2016). Note the characteristic widening of the periodontal ligament spaces and sparse trabeculation in the periapical region surrounding the premolars. |
 | Fig. 7Paraxial slice from a cone beam computed tomography study (Apr. 2016) reveals the loss of the buccal and lingual cortical borders in the region of the premolars. |
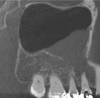 | Fig. 8Parasagittal slice from a cone beam computed tomography study (Apr. 2016) shows the altered trabeculation in the periapical region of the premolars, an oroantral communication, and the reactive mucositis of the right maxillary sinus. |
 | Fig. 9Photomicrographs exhibit a histopathological appearance of the known myeloproliferative disorder. Note the malignant neoplastic proliferation of atypical monomorphic lymphocytes forming cords, sheets, and clusters with normal nuclei and an eosinophilic cytoplasm typical of a myeloproliferative disorder (H&E stain, A. ×10, B. ×20). |
Acknowledgements
The authors would like to thank Dr. John Hiemenz from the University of Florida, College of Medicine, Department of Oncology; Dr. Joseph Katz from the University of Florida, College of Dentistry, Department of Oral Medicine; Drs. Hope Johnson, Craig Nixon, Ernest Rillman, John Zongker from the University of Florida, College of Dentistry, Department of Endodontics; Drs. Matthew Holman, Melvin Dolwick, and Benjamin Schlott from the University of Florida, College of Dentistry, Department of Oral Surgery; and Dr. Indraneel Bhattacharyya from the University of Florida, College of Dentistry, Department of Oral and Maxillofacial Diagnostic Sciences for their contributions and care provided to the patient.
References
1. Jimenez-Zepeda VH, Dominguez VJ. Plasma cell leukemia: a rare condition. Ann Hematol. 2006; 85:263–267.

2. Yamamoto JF, Goodman MT. Patterns of leukemia incidence in the United States by subtype and demographic characteristics, 1997-2002. Cancer Causes Control. 2008; 19:379–390.

3. Tiedemann RE, Gonzalez-Paz N, Kyle RA, Santana-Davila R, Price-Troska T, Van Wier SA, et al. Genetic aberrations and survival in plasma cell leukemia. Leukemia. 2008; 22:1044–1052.

5. Sher T, Miller KC, Deeb G, Lee K, Chanan-Khan A. Plasma cell leukaemia and other aggressive plasma cell malignancies. Br J Haematol. 2010; 150:418–427.

6. Han X, Kilfoy B, Zheng T, Holford TR, Zhu C, Zhu Y, et al. Lymphoma survival patterns by WHO subtype in the United States, 1973-2003. Cancer Causes Control. 2008; 19:841–858.

7. Campo E, Swerdlow SH, Harris NL, Pileri S, Stein H, Jaffe ES. The 2008 WHO classification of lymphoid neoplasms and beyond: evolving concepts and practical applications. Blood. 2011; 117:5019–5032.

9. Keraliya AR, Krajewski KM, Giardino AA, Tirumani SH, Shinagare AB, Ramaiya NH, et al. Imaging of nervous system involvement in hematologic malignancies: what radiologists need to know. AJR Am J Roentgenol. 2015; 205:604–617.

10. Fernandez de Larrea C, Kyle RA, Durie BG, Ludwig H, Usmani S, Vesole DH, et al. Plasma cell leukemia: consensus statement on diagnostic requirements, response criteria and treatment recommendations by the International Myeloma Working Group. Leukemia. 2013; 27:780–791.

11. Moulopoulos LA, Dimopoulos MA. Magnetic resonance imaging of the bone marrow in hematologic malignancies. Blood. 1997; 90:2127–2147.

12. Ali A, Paul Y, Nwabudike SM, Ogbonna O, Grantham M, Taddesse-Heath L. Plasma cell leukemia presenting as a chest wall mass: a case report. Case Rep Oncol. 2016; 9:338–343.

13. Epstein JB, Voss NJ, Stevenson-Moore P. Maxillofacial manifestations of multiple myeloma. An unusual case and review of the literature. Oral Surg Oral Med Oral Pathol. 1984; 57:267–271.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download