Abstract
Purpose
This study was designed to evaluate differences in the required visibility of anatomic structures according to the diagnostic tasks of implant planning and periapical diagnosis.
Materials and Methods
Images of a real skull phantom were acquired under 24 combinations of different exposure conditions in a cone-beam computed tomography scanner (60, 70, 80, 90, 100, and 110 kV and 4, 6, 8, and 10 mA). Five radiologists evaluated the visibility of anatomic structures and the image quality for diagnostic tasks using a 6-point scale.
Results
The visibility of the periodontal ligament space showed the closest association with the ability to use an image for periapical diagnosis in both jaws. The visibility of the sinus floor and canal wall showed the closest association with the ability to use an image for implant planning. Variations in tube voltage were associated with significant differences in image quality for all diagnostic tasks. However, tube current did not show significant associations with the ability to use an image for implant planning.
Conclusion
The required visibility of anatomic structures varied depending on the diagnostic task. Tube voltage was a more important exposure parameter for image quality than tube current. Different settings should be used for optimization and image quality evaluation depending on the diagnostic task.
Cone-beam computed tomography (CBCT) provides 3-dimensional images of the anatomic structures of the head and neck area. CBCT allows higher spatial resolution, lower radiation exposure, and a lower cost than multi-detector computed tomography (MDCT).1
Due to these advantages, CBCT scanners have been widely used for many indications in dento-maxillofacial imaging, and radiation dose concerns have increased proportionally. Therefore, the optimization of CBCT images is crucial, and it is necessary to minimize the radiation dose while maintaining the clinical image quality.
Image quality can also be assessed by the subjective evaluation and quantitative measurement of physical factors.2 Many studies have investigated the technical image quality parameters of CBCT devices, but they used different phantoms, CBCT scanners, exposure parameters, and diagnostic tasks.345678 These differences among studies make it difficult to compare the previous results directly, and no quantitative image quality criteria or standardized evaluation method has yet been developed to assess CBCT image quality.
At this point, subjective evaluation is used as the gold standard to assess image quality for certain diagnostic tasks.391011 Standardization of subjective evaluation is difficult due to its subjectivity and differences in the methodologies of previous studies.391011 Subjective evaluations usually involve the identification of anatomic structures by a radiologist.2391011 Many anatomic structures are present in the maxillofacial region, and the importance of specific landmarks may differ according to the diagnostic task.91112 However, insufficient research has addressed the relative importance of anatomic structures in relation to diagnostic tasks. This study was designed to evaluate differences in the required visibility of anatomic structures in the diagnostic tasks of implant planning and periapical diagnosis.
The CBCT images were obtained by a Dinnova3 CBCT scanner (HDXwill Inc., Seoul, Korea). The Dinnova3 scanner has an amorphous silicon flat-panel detector. The voxel size was 0.3 mm×0.3 mm×0.3 mm. A pulsed X-ray beam was rotated 360° around the phantom, and the exposure time was 12 s (scan time: 24 s). A total filtration of 2.8-mm aluminum was used. The computed tomography dose index value was 3.183 mGy (120 kV, 120 mAs, field of view [FOV]: 200 mm×190 mm). An FOV of 200 mm×190 mm was used to obtain the complete image of a real skull phantom with a soft-tissue replica (X-ray phantom, head; product number 7280, Erler Zimmer Co., Lauf, Germany) (Fig. 1).
To obtain CBCT images with different image qualities, 24 combinations of 6 different tube voltages and 4 different tube currents were used (60, 70, 80, 90, 100, and 110 kV and 4, 6, 8, and 10 mA). Images were saved in the Digital Imaging and Communications in Medicine format. All 24 sets of images were reconstructed into 3 planes (axial, coronal, and sagittal) with a slice thickness of 0.3 mm.
All reconstructed images were presented to 5 radiologists for a subjective evaluation of the image quality. Three 20.8-inch monochrome monitors (ME315L, Totoku Electric Co., Tokyo, Japan) with a resolution of 2048×1536 pixels were used, and the images of each plane were displayed on a different monitor.
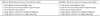
All observers had a trial session before evaluation, and the evaluation was performed individually in a random, irreversible order. The observers were not informed of the exposure conditions, and they were allowed to adjust the brightness and the contrast of the images. Each observer evaluated the left maxillary first molar area first and the right mandibular first molar area second. Observers were asked about the visibility of 3 anatomic structures in each jaw and the image quality for the diagnostic tasks of periapical diagnosis and implant planning (Table 1). The following 6-point scale was used to answer 5 items: strongly agree (6), agree (5), slightly agree (4), slightly disagree (3), disagree (2), and strongly disagree (1). The evaluation was repeated after an interval of 2 weeks to calculate intraobserver reliability.
We classified the visibility of anatomic structures as visible or invisible, and also classified the image quality for each diagnostic task as acceptable or unacceptable by using consensus criteria. In the consensus criteria, only images that obtained a score of more than 4 from all observers were defined as visible and acceptable.
The intraobserver and interobserver reliabilities of the subjective evaluations were calculated using the weighted kappa in Microsoft Office Excel 2007 (Microsoft Corp., Redmond, WA, USA). The Fisher exact test was used to evaluate the relationship between the visibility of 3 anatomic structures and image quality for 2 diagnostic tasks in SPSS version 21 (IBM Corp., Armonk, NY, USA).
The Mann-Whitney U test was used to evaluate differences in the tube voltage and currents between the visible/invisible groups and acceptable/unacceptable image quality groups in SPSS version 21. When differences in the exposure parameters were found between the acceptable and unacceptable image quality groups, cut-off values and the area under receiver operating characteristic (ROC) curves were calculated using SPSS version 21. The statistical significance level of P<.05 was used.
In the subjective evaluation, the average weighted kappa value was 0.63 (range, 0.14-1) for intraobserver reliability and 0.51 (range, 0.36-0.66) for interobserver reliability, corresponding to moderate agreement.
The agreement results between the visibility of 3 anatomic structures and image quality for 2 diagnostic tasks are presented in Table 2. The visibility of the periodontal ligament space showed a closer association with the ability to use an image for periapical diagnosis than other structures in both jaws. No statistical significance was found between the visibility of the sinus border and the usability of an image for periapical diagnosis of the maxillary first molar. Additionally, visibility of the mandibular canal wall did not show any significant relationship with the ability for an image to be used for periapical diagnosis of the mandibular first molar.
For implant planning in the maxilla, the visibility of all 3 anatomic structures showed statistically significant associations with image quality, and all kappa values showed moderate agreement. However, in the mandible, visibility of the canal wall showed the highest agreement, and the visibility of periodontal space ligament did not show a statistically significant relationship with image quality.
The differences in tube voltage and current between the visible/invisible groups and the acceptable/unacceptable groups are shown in Table 3 and Table 4. For all anatomic structures, the tube voltage of the visible images was significantly higher than in the invisible images (Table 3). However, no significant differences were found between visible and invisible images regarding the sinus border and canal wall. For all diagnostic tasks, the tube voltage of the acceptable images was significantly higher than that of the unacceptable images (Table 4). However, the tube currents in acceptable images did not show statistically significant differences from the unacceptable images for the diagnostic task of implant planning. This result implies that tube current does not have a major influence on the visibility of the sinus border and canal wall or on image quality, especially for the diagnostic task of implant planning.
The cut-off values of tube voltage for the acceptable-quality images were calculated. In all groups, the areas under the ROC curves were high, suggesting that the cut-off values were reliable (Table 5). To obtain acceptable images for the periapical diagnosis of the mandible, a tube voltage of 85 kV was required, which was 10 kV higher than needed for other diagnostic tasks.
This study investigated the relationships among the visibility of anatomic structures and image quality for 2 diagnostic tasks. The evaluation was performed using a single CBCT device and a real skull phantom. This study demonstrated that the priority of anatomic structures varied depending on the diagnostic task. For periapical diagnosis, visibility of the periodontal ligament space was most important, but the sinus border and canal wall were less important structures. In contrast, the sinus border and canal wall were the most critical anatomic structures for assessing image quality for implant planning. These results imply that different evaluation methods may be needed for different diagnostic tasks.
Many studies have been conducted on CBCT image quality, but insufficient information has been published on the assessment of the relationship between image quality and the visibility of anatomic structures corresponding to specific diagnostic tasks.2 Only 3 studies have evaluated 2 or more diagnostic tasks.3911 All 3 studies reported that the required image quality varied according to the diagnostic task. Lofthag-Hansen et al. and Choi et al. reported that a higher image quality was required for periapical diagnosis than for implant planning.911 These results correspond with the results of this study. The results of Pauwels et al. also showed that image quality was related to diagnostic tasks, but they reported that image quality was device-dependent and that it was difficult to set a reference value.3
Changes in tube voltage showed a significant effect on the visibility of all anatomic structures and image quality for the 2 diagnostic tasks. Especially for periapical diagnosis of the mandible, a higher tube voltage was required. In contrary, adjusting the tube current did not lead to significant differences in the visibility of the sinus border and canal wall or in image quality for implant planning. These results support the proposal that by reducing tube current, it is possible to reduce radiation dosage without image quality degradation for implant planning. These results are in agreement with those of previous studies.21314 However, reducing the tube current deteriorated the image quality for periapical diagnosis. Periapical diagnosis may require better image quality than implant planning because the periodontal ligament space (PDL) is an important structure for periapical diagnosis. However, it is a fine structure and is susceptible to small amounts of noise. Earlier studies have demonstrated that the PDL space and lamina dura are less visible structures than other anatomical structures using several protocols with different CBCT devices.315 Therefore, optimization by lowering the tube current is considered to be difficult for periapical diagnosis, and other strategies would be needed.
In conclusion, the required visibility of anatomic structures varied depending on the diagnostic task. Tube voltage was a more important exposure parameter for image quality than tube current. Different protocols should be used for optimization and image quality evaluation depending on the diagnostic task, and these results can be a starting point for future research into the evaluation of the image quality of CBCT devices.
Figures and Tables
Table 2
Agreements between visibility of three anatomic structures and image quality for diagnostic tasks

References
1. Ludlow JB, Ivanovic M. Comparative dosimetry of dental CBCT devices and 64-slice CT for oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 106:106–114.

2. Goulston R, Davies J, Horner K, Murphy F. Dose optimization by altering the operating potential and tube current exposure time product in dental cone beam CT: a systematic review. Dentomaxillofac Radiol. 2016; 45:20150254.

3. Pauwels R, Seynaeve L, Henriques JC, de Oliveira-Santos C, Souza PC, Westphalen FH, et al. Optimization of dental CBCT exposures through mAs reduction. Dentomaxillofac Radiol. 2015; 44:20150108.

4. Pauwels R, Beinsberger J, Stamatakis H, Tsiklakis K, Walker A, Bosmans H, et al. Comparison of spatial and contrast resolution for cone-beam computed tomography scanners. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012; 114:127–135.

5. Bamba J, Araki K, Endo A, Okano T. Image quality assessment of three cone beam CT machines using the SEDENTEXCT CT phantom. Dentomaxillofac Radiol. 2013; 42:20120445.

6. Watanabe H, Honda E, Kurabayashi T. Modulation transfer function evaluation of cone beam computed tomography for dental use with the oversampling method. Dentomaxillofac Radiol. 2010; 39:28–32.

7. Xu J, Reh DD, Carey JP, Mahesh M, Siewerdsen JH. Technical assessment of a cone-beam CT scanner for otolaryngology imaging: image quality, dose, and technique protocols. Med Phys. 2012; 39:4932–4942.

8. Ozaki Y, Watanabe H, Nomura Y, Honda E, Sumi Y, Kurabayashi T. Location dependency of the spatial resolution of cone beam computed tomography for dental use. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013; 116:648–655.

9. Lofthag-Hansen S, Thilander-Klang A, Grondahl K. Evaluation of subjective image quality in relation to diagnostic task for cone beam computed tomography with different fields of view. Eur J Radiol. 2011; 80:483–488.

10. Tapiovaara M. Review of relationships between physical measurements and user evaluation of image quality. Radiat Prot Dosimetry. 2008; 129:244–248.

11. Choi JW, Lee SS, Choi SC, Heo MS, Huh KH, Yi WJ, et al. Relationship between physical factors and subjective image quality of cone-beam computed tomography images according to diagnostic task. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015; 119:357–365.

12. De Cock J, Zanca F, Canning J, Pauwels R, Hermans R. A comparative study for image quality and radiation dose of a cone beam computed tomography scanner and a multislice computed tomography scanner for paranasal sinus imaging. Eur Radiol. 2015; 25:1891–1900.

13. Dawood A, Brown J, Sauret-Jackson V, Purkayastha S. Optimization of cone beam CT exposure for pre-surgical evaluation of the implant site. Dentomaxillofac Radiol. 2012; 41:70–74.

14. Sur J, Seki K, Koizumi H, Nakajima K, Okano T. Effects of tube current on cone-beam computerized tomography image quality for presurgical implant planning in vitro. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 110:e29–e33.

15. Liang X, Jacobs R, Hassan B, Li L, Pauwels R, Corpas L, et al. A comparative evaluation of Cone Beam Computed Tomography (CBCT) and Multi-Slice CT (MSCT) Part I. On subjective image quality. Eur J Radiol. 2010; 75:265–269.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download