Abstract
Purpose
The aim of this article is to review a group of lesions associated with periodontal ligament (PDL) widening.
Materials and Methods
An electronic search was performed using specialized databases such as Google Scholar, PubMed, PubMed Central, Science Direct, and Scopus to find relevant studies by using keywords such as “periodontium”, “periodontal ligament”, “periodontal ligament space”, “widened periodontal ligament”, and “periodontal ligament widening”.
Results
Out of nearly 200 articles, about 60 were broadly relevant to the topic. Ultimately, 47 articles closely related to the topic of interest were reviewed. When the relevant data were compiled, the following 10 entities were identified: occlusal/orthodontic trauma, periodontal disease/periodontitis, pulpo-periapical lesions, osteosarcoma, chondrosarcoma, non-Hodgkin lymphoma, progressive systemic sclerosis, radiation-induced bone defect, bisphosphonate-related osteonecrosis, and osteomyelitis.
The periodontal ligament, commonly known as the PDL, is a soft connective tissue between the inner wall of the alveolar socket and the roots of the teeth. It consists of collagen bands (mostly type I collagen) connecting the cementum of teeth to the gingivae and alveolar bone. Fibroblasts are the main cells in the PDL, which form, maintain, and repair the alveolar bone and cementum. In addition, sensors in the PDL provide proprioceptive input and detect pressure applied to the teeth.123 The morphology of the PDL varies in terms of tooth anatomy and even tooth surface. For example, it is thinner in the middle of the root and slightly wider near the root apex and alveolar crest, suggesting that the fulcrum of tooth physiologic movement is located in the thinnest area of the PDL.24 Radiographically, the PDL is seen as a radiolucent space between the lamina dura and the tooth root. The normal width of the PDL ranges from 0.15 mm to 0.21 mm, which may decrease with age.14 Widening of the PDL is one of the most important changes in the circumdental structures and may be related to different abnormalities.5 It is important to detect whether the widening is regular or irregular in shape and if the lamina dura is still present. For instance, orthodontic movement of teeth results in PDL widening, but the lamina dura remains intact. In contrast, malignant or locally aggressive lesions can quickly grow downwards into the ligament space, resulting in an irregular widening and destruction of the lamina dura.456 Radiography remains the primary mode of investigation for evaluating jaw lesions in routine dental practice.7 Although PDL widening may be encountered by many dentists during their routine daily procedures, some cases might be related to serious lesions or diseases. Therefore, the aim of this article was to review 10 entities of the greatest clinical importance that involve PDL widening in order to draw dental practitioners' attention to this imaging finding and to help dental practitioners make more accurate diagnoses and better treatment plans based on patients' radiographs.
In this review, general search engines and specialized databases including Google Scholar, PubMed, PubMed Central, Science Direct, and Scopus were consulted to find relevant studies by using the keywords “periodontium”, “periodontal ligament”, “periodontal ligament space”, “widened periodontal ligament”, and “periodontal ligament widening”. Nearly 200 articles were found, with about 60 being highly relevant to the topic. About 140 articles were excluded from the review process for the following reasons: They were written in languages other than English, their full text was unavailable, they were in the form of case reports with a small number of cases that only indicated the presence of the topic without demonstrating the frequency, or they mostly focused on changes in the jawbones rather than in the PDL. Out of 60 selected articles, newly published papers with non-repetitive subjects were studied, and 15 were omitted. We ultimately included 47 articles that were closely related to the topic of interest. When the relevant data were compiled, 10 entities were identified.
From a review of the literature, 10 entities associated with PDL widening were identified, as detailed below.
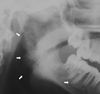
Traumatic occlusion or occlusal trauma is defined as an excessive force or pressure on 1 tooth or on the teeth leading to either an increased alveolar support or a breaking down of supporting tissues.8 Traumatic occlusion can cause degenerative changes in response to pressures greater than the physiologic tolerance of tooth-supporting tissues. In addition to clinical signs and symptoms such as tooth mobility, wear facets, pain, unusual response to percussion, and a history of para-functions, there are some radiographic features, including PDL widening, thickening of the lamina dura, bone loss, and increased number and size of trabeculae.49 The PDL, which lies between the cementum and alveolar bone, acts as a cushion to withstand mechanical forces applied to teeth, and responds by remodeling. When a continuous force is applied on the crown of a tooth, it causes tooth movement that is marked initially by narrowing of the periodontal membrane. However, in the secondary period of tooth movement, direct bone resorption takes place, and the PDL is considerably widened (Fig. 1). It has been shown that PDL cells, under mechanical stress, may induce secretion of osteoclasts via PGE2 synthesis during orthodontic tooth movement.10
Kundapur et al.,11 in a study on 300 patients with traumatic occlusion seeking periodontal consultation, found that PDL widening alone was seen in 8.7%, PDL widening with bone loss was observed in 2.7%, and PDL widening accompanied by bone loss and lamina dura thickening was noticed in 0.7% of cases.
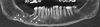
Other sequelae of traumatic occlusion are hypercementosis and root fracture. Traumatic occlusion alone does not lead to periodontal disease, but bone loss might be accelerated in the presence of preexisting periodontitis. As clinical examination might be insufficient for the diagnosis of this entity, radiographic evaluation was highly recommended.4 Orthodontic forces can cause PDL widening while also sparing the lamina dura (Fig. 2).456
Periodontal disease, including gingivitis and periodontitis, is a chronic immune inflammatory response associated with genetic and environmental factors.12 Periodontitis is characterized by an inflammatory destruction of the supporting apparatus of the tooth (periodontal ligament, cementum, and alveolar bone), which results in gradual loosening of the teeth.13 Radiography plays a key role in the assessment of this entity. Similar to all inflammatory lesions of the jawbone, periodontal disease/periodontitis usually is a combination of bone loss (mostly in the early acute phase) and bone formation or even sclerosis (mostly in the chronic phase). Early periodontitis causes blunting of the alveolar crest and decreasing alveolar bone height in the anterior portions of the jaws. Loss of a normally sharp angle between the lamina dura and the alveolar crest might also be noticed in the posterior regions.4 In chronic cases, horizontal and vertical bone loss can be seen. A vertical bone defect develops when bone loss progresses down the root of the teeth in association with a deep periodontal pocket. In its early stage, this phenomenon appears as abnormal PDL widening (Fig. 3). Bone loss in buccal or lingual cortical plates and osseous deformities in the furcations of multi-rooted teeth can occur in sustained cases. Widening of the PDL at the apex or inter-radicular area is an important piece of evidence for periodontal disease.4 Early detection of periodontal disease and correct management of bony defects are essential for better diagnosis, treatment, and prognosis of this entity.13
These groups of lesions are considered to be the most common entities associated with pulpitis or improper root canal therapy.14 Marmary and Kutiner15 demonstrated that periapical defects could be seen in 34% of deep caries, and that a relationship existed between carious lesions and periapical bony changes. In another study, the prevalence of apical lesions in association with root-filled teeth has been reported to be as much as 64%, and PDL widening was the first sign in radiographs.13 In the study of Dayal et al.,16 54.2% of teeth with pulpitis had radiographic changes mostly in the form of chronic pulpitis and pulp polyp. In addition, PDL widening was the most common finding in the majority of cases (46.1%) (Fig. 4) followed by discontinuity of the lamina dura (20.2%), thickening of the lamina dura (18%), and condensing osteitis (12.3%). Widened PDL was also reported in teeth with sub-acute pulpitis, acute pulpitis, and pulp hyperemia. It was noted that PDL widening in root apices was usually the characteristic feature of inflammatory lesions with an endodontic origin.17
Osteomyelitis is a bone infection. This entity has 2 phases: acute or chronic. The acute phase of the disease can affect patients of all ages, with a strong male predilection.4 It is much more common in the mandible than maxilla, possibly because of the poorer mandibular vascular supply.1819 The symptoms of the chronic form are sustained and generally less severe. In patients with extensive lesions, the disease may spread to the mandibular condyle and into the joints, resulting in a septic arthritis. It also may develop a draining fistula, which may appear as a well-defined break in the outer cortex or in the periosteal new bone (Fig. 5).4 Radiography has a key role in the diagnosis and follow-up of the disease. A slight decrease in the density of the affected bone may be noted. However, acute osteomyelitis can stimulate either bone resorption or bone formation. Sequestra serve as a radiographic finding in the advanced stage of the acute disease.181920 Chronic osteomyelitis usually stimulates the formation of periosteal new bone similar to an “onion skin” pattern. Meanwhile, teeth may undergo external root resorption, the lamina dura blends with the peripheral granular sclerotic bone and becomes less apparent, and the PDL space is widened in the apical region.4 According to Gupta,18 a widened periodontal ligament space or a defect of the lamina dura might be an initial radiographic indicator for osteomyelitis. Destruction of bone initially proceeded within cancellous bone. The cortical plate was secondarily involved by progressive bone resorption and increasing pressure exerted by the inflammation.181920
After multiple myeloma, osteosarcoma is the most frequent primary malignant bone tumor at an estimated incidence of 2 or 3 per 100,000 persons.21 However, osteosarcoma of the jaws is a rare entity, constituting 5% to 13% of all cases of osteosarcoma.22 More than 80% of cases occurred between 5 and 25 years, but a second, lower peak incidence has been reported in the fifth and sixth decades. No sex or race predilection has been observed, and the mandible is more commonly affected than the maxilla.21 Osteosarcoma clinically presents as a firm swelling with increasing size over months. It can be accompanied by paresthesia, pain, distortion of facial bones, tooth mobility, and toothache leading to ill-advised extraction.21 Early detection is the most critical factor for improving prognosis. In most cases, the average elapsed time between initial symptoms and final diagnosis is 3 to 5 months.2123 The diagnosis of osteosarcoma is typically suspected by the radiographic changes in the affected bone. According to Garrington et al.,24 early osteosarcoma of the jaws showed a symmetrically widened PDL of 1 or more teeth on a periapical dental radiograph, apparently before showing any other radiographic features. In addition, it was mentioned that widening of the PDL could occur asymmetrically (Fig. 6).21 In a case series by Givol et al.,23 PDL widening was detected in 28% of jawbone osteosarcomas, and it was pointed out that symmetrical widening of the PDL was a prominent feature of osteosarcoma. Other radiographic findings were mixed radiolucent/radiopaque lesions, radiopaque masses with a moth-eaten pattern, a Codman triangle, and a sun-burst appearance.21
After multiple myeloma and osteosarcoma, chondrosarcoma is the third most common primary malignant tumor of the jawbone.25 Only 5% to 10% of chondrosarcomas occur in the head and neck. It may present at any age; however, most cases are found between the third and sixth decades of life.2627 Males are more frequently affected than females, and the maxilla is involved more than the mandible.25 Clinically, the tumor manifests as a painless swelling or mass associated with loosening of the involved tooth.26 Pain may be a late symptom, and regional lymphadenopathy is rare.27 Although it may mimic the appearance of osteosarcoma on radiographs,25 no pathognomonic image finding has been found for this lesion. Solitary or multiple radiolucencies with ill-defined borders, bone destruction associated with calcifications, ground-glass or sun-ray/sun-burst appearance, and uniform widening of the PDL may occasionally be present.27 In tooth-bearing areas, a widened PDL (a Garrington sign) may be noticed as an early sign of chondrosarcoma.28 If the lesion occurs near the teeth, tooth displacement and root resorption may also be seen.4
Lymphoma is a malignant lympho-proliferative disorder divided into 2 types: Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL).29 Primary NHL is found outside of nodal tissues in 24% to 45% of cases, with the commonly affected sites being the gastrointestinal tract and skin. Bone involvement is rare and represents only 5% of all extra-nodal lymphomas. NHL of the jaws affects adults in the fourth and fifth decades of life, with a male predilection (male to female ratio of 3:2).30 When occurring in tooth-bearing areas, NHL typically appears as a dental pathology, which makes it difficult to establish a timely diagnosis. On average, more than 2 months between initial presentation and final diagnosis of NHL elapse.31 Clinically, it presents as a bony swelling, tooth mobility, a mass in an extraction socket, pain, pathologic fracture, and anesthesia or paresthesia in the pathway of the inferior alveolar nerve.30 With respect to imaging, no pathognomonic feature has been detected for NHL; however, it usually appears as a poorly defined radiolucency similar to many common odontogenic pathologies such as chronic apical periodontitis.3032 Yapes et al.33 reported a case of NHL that was misdiagnosed as a periodontal abscess. Other radiographic features of NHL include loss of cortical definition, widening of the mandibular canal, widening of the mental foramen, loss of lamina dura, and widening of the PDL.30 Irregular and diffuse widening of the PDL was reported as a radiographic finding of NHL involving the maxilla by Buchanan et al.32 The same findings were reported by Imaizumi et al.34 in the mandible.
Progressive systemic sclerosis is a generalized connective tissue disease that leads to excessive collagen deposition and hardening of the skin and other tissues. It is a disease of middle age (30 to 50 years), and is 3 times more frequent in women than men.4 Oral manifestations of progressive systemic sclerosis include limitation in mouth opening, xerostomia, periodontal disease, increase in the width of the PDL, and mandibular bone resorption.35 The most common oral radiographic finding of progressive systemic sclerosis is an increase in the width of the PDL occurring in about two-thirds of patients. The affected PDL space usually is at least twice as thick as normal, and both anterior and posterior teeth are involved.4 The incidence of PDL widening in patients with progressive systemic sclerosis varied from 7% by Stafne to 100% by Marmary et al.3637 In a recent study, Anbiaee and Tafakhori35 argued that progressive systemic sclerosis should be considered in the differential diagnosis in patients with PDL widening and intact lamina dura, especially in posterior immobile teeth when widened PDL is found in more than 1 quadrant (Fig. 7). Moreover, two-thirds of patients with progressive systemic sclerosis present with widening of the PDL.38 In a case series by Baron et al.,1 erosion of the mandible and widening of the PDL have been mentioned as the major radiographic features that differentiate progressive systemic sclerosis from the normal condition. Baron et al.1 also demonstrated that disease severity was significantly related to the number of teeth with widened PDL. The main reasons for PDL widening are not well understood. Auluk39 suggested that this change is caused by involvement of the masticatory muscle, which becomes more bulky, and exerts an increased occlusal force resulting in primary trauma from occlusion. However, this mechanism has been rejected by Mehra.40 Considering the high fibroblast and collagen content of the PDL, it is not surprising that widening of the PDL in these patients is caused by excess deposition of collagen and oxytalan fibers with subsequent resorption of the alveolar crest surrounding the root.141
Radiation injury to the jaws is one of the serious complications following radiotherapy of orofacial malignant lesions.42 The type and maturity of bone and the dose of radiation are crucial factors determining how the bone responds to this injury. When immature bone is irradiated, growth retardation occurs. Radiation damage to mature bone is likely dose-dependent, and can affect osteoblasts (decrease in matrix formation) and osteoclasts (increase in bone resorption). The most frequent regions affected by radiotherapy are the posterior aspect of the mandible, followed by the posterior maxilla. In order to minimize the adverse effects of radiotherapy, early detection of bone injuries is important. In general, radiographic changes are of little use in the early diagnosis of radiation bone defects.442 However, in the alveolar process of the jaws, an irregular widening of the PDL around the involved teeth is the most common radiographic feature after radiation (Fig. 8).4 In a study by Fujita et al.,42 PDL widening was mentioned as an early radiographic change observed in orofacial radiotherapy. The same findings were also reported by other researchers in 2 animal studies.4344 Recently, it has been demonstrated that more than 50% of patients under therapeutic radiation therapy exhibited PDL widening, and most cases were not detected until 2 years after radiation. The PDL widening was also more severe when the mandibular dose exceeded 45 Gy.4 As a possible pathogenesis, it has been proposed that the diminished vascularity of the PDL membrane and edema increase the volume of the periodontal ligament, leading to resorbing of the tooth socket wall, which might be accelerated within the devitalized irradiated bone.445 Other radiographic changes were similar to periodontal disease bone loss.4
Bisphosphonates are medications used in the management or treatment of osteoporosis, osseous metastases, osteogenesis imperfecta, rheumatoid arteritis, thalassemia major, multiple myeloma, and malignancy-related hypercalcemia.46 In 2003, the relationship between osteonecrosis of the jaws and bisphosphonates was first described.47 The clinical feature is variable, in a way that some patients may be asymptomatic while others present with painful bone exposure, mobile teeth, soft tissue inflammation, non-healing extraction socket, and sinus tract and neurosensory disorders.4648 Diagnosis may be delayed, because it has no specific radiographic characteristics. Common radiographic findings are sclerosis of the alveolar margin and thickening of the lamina dura, narrowing of the inferior alveolar canal, periosteal reaction, sequestra, PDL widening, and periapical radiolucency.464849 In a study by Fleisher et al.,48 PDL widening was the most common finding in patients with bisphosphonate-related osteonecrosis. It was found in 83% of cases who used bisphosphonates intravenously or orally, and 88% of cases who consumed bisphosphonates only via a parenteral route. It was also demonstrated that the presence of PDL widening may be a more sensitive indicator than CTX testing (type I collagen carboxy-terminal telopeptide) in predicting the risk of bone necrosis. In another study by Moeini et al.,46 thickening of the lamina dura, poorly healed or non-healed sockets, widening of the PDL, and sclerotic changes in the mandibular canal were found in 58%, 41.6%, 33.3%, and 25% of children taking bisphosphonates.
This review revealed that widening of the PDL might be due to 10 relatively common entities, which could be categorized into 4 groups: traumatic, infectious, neoplastic, or systemic causes.
Traumatic causes of PDL widening are occlusal/orthodontic trauma and radiation-induced bone defect. Traumatic occlusion is caused by developmental abnormalities of the jaws or inappropriate restorative, prosthetic, or even orthodontic procedures that eventually lead to PDL widening in 1 tooth or multiple teeth.8910 Because of its impacts on bony tissues, radiotherapy can be regarded as a traumatic cause of PDL widening as well.44243
Periodontal disease/periodontitis, pulpo-periapical lesions, and osteomyelitis are among the infectious causes of PDL widening. Periodontal pathogens or the spread of dental abscess promotes widening of the periodontal ligament.413 Some reports demonstrated that pulpitis, pulpo-periapical pathologies, or even vital pulps with minimal hyperemic involvement resulted in widened PDL via an infectious pathway.141617 On the other hand, pain, fever, swelling of the adjacent soft tissues, lymphadenopathy, and leukocytosis should prompt the clinician toward osteomyelitis.418
Widening of the PDL can also be induced by neoplastic lesions of the jawbones, such as osteosarcoma, chondrosarcoma, and NHL. Widening of the PDL, especially with an asymmetrical distribution accompanied by a bony mass in the jaws with a progressive pattern of growth, must prompt the dental clinician to consider osteosarcoma and chondrosarcoma in the differential diagnosis and to undertake more elaborated diagnostic procedures.232628 On the other hand, the first manifestation of NHL can be widening of the PDL or jaw lesions mimicking periodontal disease.3233
Meanwhile, periapical lesions refractory to root canal therapy might be diagnosed as lymphoma, according to some reports.29 It has been generally accepted that a majority of neoplasms have a better prognosis if detected in earlier stages; however, PDL widening is a less-addressed sign of oral lymphoma in dental academic courses.
Progressive systemic sclerosis and bisphosphonate-related osteonecrosis are 2 systemic conditions leading to widened PDL. Up to 100% of patients with progressive systemic sclerosis show this sign.3637 Widening of the PDL is an early sign of progressive systemic sclerosis, which might help dental practitioners establish timely diagnosis through appropriate laboratory tests.35 In patients taking bisphosphonates, PDL widening can be a good indicator for the prediction of osteonecrosis development.48
This review focused on the connection between dental and medical disciplines and the role of dental practitioners as pioneers of the diagnostic process in some instances. Meanwhile, special effort has been made to introduce a narrow differential diagnosis, helping dentists make more logical decisions when confronting such lesions. Clearly, both strategies lead to selecting better treatment protocols for patients.
Figures and Tables
 | Fig. 1Widening of periodontal ligament around the right mandibular second molar is evident with loss of neighboring teeth, subjecting it to heavy occlusal trauma. |
 | Fig. 2Panoramic radiograph demonstrates generalized periodontal ligament widening due to trauma from orthodontic forces. |
 | Fig. 3Periapical radiographs show periodontal ligament widening around maxillary and mandibular incisors due to periodontitis. |
 | Fig. 4Periodontal ligament widening as a result of pulpo-periapical lesion is seen in the left mandibular second molar. |
 | Fig. 5Panoramic reconstructed cone-beam computed radiographic image shows chronic sclerosing osteomyelitis with periodontal ligament widening around right mandibular canine as well as mental fistula. |
 | Fig. 6Widening of periodontal ligament is evident in the roots of the right mandibular first molar in a patient with osteosarcoma. Note the sun-ray appearance in the ascending ramus and the angle of the mandible. |
Acknowledgements
The authors are especially thankful to Dr. Abbas Shokri and Dr. Amin Khodadoustan, and Dr. Yaser Safi for providing figures.
References
1. Baron M, Hudson M, Dagenais M, Macdonald D, Gyger G, El Sayegh T, et al. Relationship between disease characteristics and oral radiologic findings in systemic sclerosis: results from a Canadian oral health study. Arthritis Care Res (Hoboken). 2016; 68:673–680.

2. Xie JX. Radiographic analysis of normal periodontal tissues. Zhonghua Kou Qiang Yi Xue Za Zhi. 1991; 26:339–341.
3. Kaku M, Yamauchi M. Mechano-regulation of collagen biosynthesis in periodontal ligament. J Prosthodont Res. 2014; 58:193–207.

4. White SC, Pharoah MJ. Oral radiology: principles and interpretation. 7th ed. St. Louis: Elsevier;2014.
5. van der Waal I. Non-plaque related periodontal lesions. An overview of some common and uncommon lesions. J Clin Periodontol. 1991; 18:436–440.

6. Razavi SM, Kiani S, Khalesi S. Periapical lesions: a review of clinical, radiographic, and histopathologic features. Avicenna J Dent Res. 2015; 7:e19435.

7. Mortazavi H, Baharvand M, Rahmani S, Jafari S, Parvaei P. Radiolucent rim as a possible diagnostic aid for differentiating jaw lesions. Imaging Sci Dent. 2015; 45:253–261.

8. Arnold M. Bruxism and the occlusion. Dent Clin North Am. 1981; 25:395–407.
9. Borges RN, Arantes BM, Vieira DF, Guedes OA, Estrela C. Occlusal adjustment in the treatment of secondary traumatic injury. Stomatos. 2011; 17:43–50.
10. Meeran NA. Biological response at the cellular level within the periodontal ligament on application of orthodontic force - An update. J Orthod Sci. 2012; 1:2–10.

11. Kundapur PP, Bhat KM, Bhat GS. Association of trauma from occlusion with localized gingival recession in mandibular anterior teeth. Dent Res J (Isfahan). 2009; 6:71–74.
12. Mortazavi H, Lotfi G, Fadavi E, Hajian SH, Baharvand M, Sabour S. Is ABO blood group a possible risk factor for periodontal disease? Dent Hypotheses. 2015; 6:14–18.

13. Kumar V, Arora K, Udupa H. Different radiographic modalities used for detection of common periodontal and periapical lesions encountered in routine dental practice. J Oral Hyg Health. 2014; 2:163.
14. Kuc I, Peters E, Pan J. Comparison of clinical and histologic diagnoses in periapical lesions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000; 89:333–337.

15. Marmary Y, Kutiner G. A radiographic survey of periapical jawbone lesions. Oral Surg Oral Med Oral Pathol. 1986; 61:405–408.

16. Dayal PK, Subhash M, Bhat AK. Pulpo-periapical periodontitis: a radiographic study. Endodontology. 1999; 11:60–64.
17. Chapman MN, Nadgir RN, Akman AS, Saito N, Sekiya K, Kaneda T, et al. Periapical lucency around the tooth: radiologic evaluation and differential diagnosis. Radiographics. 2013; 33:E15–E32.

18. Gupta D. Role of maxillofacial radiology and imaging in the diagnosis and treatment of osteomyelitis of the jaws. J Dent Oral Disord Ther. 2015; 3:1–2.

19. Yoshiura K, Hijiya T, Ariji E, Sa'do B, Nakayama E, Higuchi Y, et al. Radiographic patterns of osteomyelitis in the mandible. Plain film/CT correlation. Oral Surg Oral Med Oral Pathol. 1994; 78:116–124.

20. Schuknecht B, Valavanis A. Osteomyelitis of the mandible. Neuroimaging Clin N Am. 2003; 13:605–618.

21. Chittaranjan B, Tejasvi MA, Babu BB, Geetha P. Intramedullary osteosarcoma of the mandible: a clinicoradiologic perspective. J Clin Imaging Sci. 2014; 4:Suppl 2. 6.

22. Babazade F, Mortazavi H, Jalalian H. Bilateral metachronous osteosarcoma of the mandibular body: a case report. Chang Gung Med J. 2011; 34:6 Suppl. 66–69.
23. Givol N, Buchner A, Taicher S, Kaffe I. Radiological features of osteogenic sarcoma of the jaws. A comparative study of different radiographic modalities. Dentomaxillofac Radiol. 1998; 27:313–320.

24. Garrington GE, Scofield HH, Cornyn J, Hooker SP. Osteosarcoma of the jaws. Analysis of 56 cases. Cancer. 1967; 20:377–391.
25. Wood NK, Goaz PW. Differential diagnosis of oral and maxillofacial lesions. 5th ed. St. Louis: Mosby;1997.
26. Saini R, Abd Razak NH, Ab Rahman S, Samsudin AR. Chondrosarcoma of the mandible: a case report. J Can Dent Assoc. 2007; 73:175–178.
27. Kundu S, Pal M, Paul RR. Clinicopathologic correlation of chondrosarcoma of mandible with a case report. Contemp Clin Dent. 2011; 2:390–393.

28. Mahajan AM, Ganvir S, Hazarey V, Mahajan MC. Chondrosarcoma of the maxilla: a case report and review of literature. J Oral Maxillofac Pathol. 2013; 17:269–273.

29. Mendonça EF, Sousa TO, Estrela C. Non-Hodgkin lymphoma in the periapical region of a mandibular canine. J Endod. 2013; 39:839–842.

30. Steinbacher DM, Dolan RW. Isolated non-Hodgkin's lymphoma of the mandible. Oral Oncol Extra. 2006; 42:187–189.

31. Parrington SJ, Punnia-Moorthy A. Primary non-Hodgkin's lymphoma of the mandible presenting following tooth extraction. Br Dent J. 1999; 187:468–470.

32. Buchanan A, Kalathingal S, Capes J, Kurago Z. Unusual presentation of extranodal diffuse large B-cell lymphoma in the head and neck: description of a case with emphasis on radiographic features and review of the literature. Dentomaxillofac Radiol. 2015; 44:20140288.

33. Yepes JF, Mozaffari E, Ruprecht A. Case report: B-cell lymphoma of the maxillary sinus. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 102:792–795.

34. Imaizumi A, Kuribayashi A, Watanabe H, Ohbayashi N, Nakamura S, Sumi Y, et al. Non-Hodgkin lymphoma involving the mandible: imaging findings. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012; 113:e33–e39.

35. Anbiaee N, Tafakhori Z. Early diagnosis of progressive systemic sclerosis (scleroderma) from a panoramic view: report of three cases. Dentomaxillofac Radiol. 2011; 40:457–462.

36. Stafne EC. Dental roentgenologic manifestations of systemic disease. III. Granulomatous disease, Paget's disease, acrosclerosis and others. Radiology. 1952; 58:820–829.
37. Marmary Y, Glaiss R, Pisanty S. Scleroderma: oral manifestations. Oral Surg Oral Med Oral Pathol. 1981; 52:32–37.

38. Prasad RS, Pai A. Localized periodontal ligament space widening as the only presentation of scleroderma - reliability recheck. Dentomaxillofac Radiol. 2012; 41:440.
39. Auluck A. Widening of periodontal ligament space and mandibular resorption in patients with systemic sclerosis. Dentomaxillofac Radiol. 2007; 36:441–442.

40. Mehra A. Periodontal space widening in patients with systemic sclerosis: a probable explanation. Dentomaxillofac Radiol. 2008; 37:183.

41. Jagadish R, Mehta DS, Jagadish P. Oral and periodontal manifestations associated with systemic sclerosis: a case series and review. J Indian Soc Periodontol. 2012; 16:271–274.

42. Fujita M, Tanimoto K, Wada T. Early radiographic changes in radiation bone injury. Oral Surg Oral Med Oral Pathol. 1986; 61:641–644.

43. Medak H, Oartel JS, Burnett GW. The effect of x-ray irradiation on the incisors of the Syrian hamster. Oral Surg Oral Med Oral Pathol. 1954; 7:1011–1020.

44. Chambers F, Ng E, Ogden H, Coggs G, Crane J. Mandibular osteomyelitis in dogs following irradiation. Oral Surg Oral Med Oral Pathol. 1958; 11:843–859.

45. Kassim N, Sirajuddin S, Biswas S, Rafiuddin S, Apine A. Iatrogenic damage to the periodontium caused by radiation and radiotherapy. Open Dent J. 2015; 9:182–186.

46. Moeini M, Moeini M, Lotfizadeh N, Alavi M. Radiotherapy finding in the jaws in children taking bisphosphonate. Iran J Ped Hematol Oncol. 2013; 3:114–118.
47. Marx RE. Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg. 2003; 61:1115–1117.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download