Abstract
A static, unilateral, and focal bone depression located lingually within the ascending ramus, identical to the Stafne's bone cavity of the angle of the mandible, is being reported. During development of the mandible, submandibular gland inclusion may lead to the formation of a lingual concavity, which could contain fatty tissue, blood vessels, or soft tissue. However, similar occurrences in the ascending ramus at the level of the parotid gland are extremely rare. Similar cases were previously reported in dry, excavated mandibles, and 3 cases were reported in living patients. A 52-year-old African American male patient was seen for pain in the mandibular teeth. Panoramic radiography showed an unusual concavity within the left ascending ramus. Cone-beam computed tomography confirmed this incidental finding. The patient was cleared for the extraction of non-restorable teeth and scheduled for annual follow-up.
Mandibular bone cavities, depressions, and defects have often been described in connection to the development of the salivary glands. They were first described by Stafne1 in 1942 and are now generally accepted to be developmental in origin.23 In this regard, the submandibular and sublingual glands have been more commonly investigated2 than the parotid gland, which is the largest salivary gland. Some researchers have found an association of fatty tissue and blood vessels with mandibular bone cavities,4 while others3 have reported, using computed tomography (CT) and sialography, that the cavitation resulted from the entrapment of salivary gland tissue during development of the mandible from Meckel's cartilage.56 Archeological findings have demonstrated the possibility of lingual salivary gland depressions in the region corresponding to the parotid gland, although such defects have been reported to be located superiorly in the ascending ramus in only a handful of patients.378 A developmental salivary gland defect on the ascending ramus was first reported using cone-beam CT (CBCT) imaging by Campos et al.;7 they attributed the formation of the ramus defect to focal failure in the ossification of the mandible and not to a developmental relation with the salivary gland. The defect or depression in our report appears to have been more defined, singular, and located higher in the ramus than the lesion described by Campos et al.7 These authors present findings obtained using both panoramic and CBCT imaging.
A 52-year-old African-American male patient was referred to the emergency clinic of the Department of Oral Medicine at the University of Pennsylvania School of Dental Medicine by a private dentist for possible extractions of the maxillary left first molar, mandibular left third molar, and second premolar due to severe periodontal bone loss and pain.
A comprehensive intraoral and extraoral exam was completed. The patient was well developed and well nourished. Tooth vitality tests were performed; the dental complaint of pain was odontogenic in nature, and was limited to the maxillary left first molar, mandibular left third molar, and second premolar. There was no evidence for suppuration or swelling. Bilateral mandibular tori were noted. The temporomandibular joint (TMJ) exhibited a full range of motion, and neither crepitus nor clicking were noted. The patient denied any history of pain associated with the TMJ or myofascial pain related to the muscles of mastication. Cranial nerves II through XII were grossly intact. Submandibular lymph nodes were palpable, non-tender, and mobile. The patient's vital signs were within the normal limits. The patient denied taking any medications other than a course of antibiotics prescribed for the periodontal infection by his general dentist.
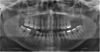
A panoramic radiograph, taken after the initial examination, revealed that the maxillary left first molar exhibited severe vertical bone loss, the mandibular left third molar was symptomatic with an apical rarefying osteitis in relation to the mesiobuccal root, and the mandibular left second premolar was symptomatic with irreversible pulpitis (based on vitality tests) and appeared to be non-restorable. The panoramic examination also revealed an atypical bone cavity that presented as an ovoid radiolucency with well-defined, corticated borders at the superior region of the ascending left ramus (Fig. 1). The area was asymptomatic and appeared to have no relationship with the chief dental complaint. The area appeared to be non-odontogenic in nature. The patient denied any active medical conditions or knowledge of mandibular atypia prior to the dental examination at our clinic.
CBCT was recommended to visualize the lesion 3-dimensionally. A medium-volume CBCT scan was performed at a voxel resolution of 200 µm (CS 9300, Carestream, Atlanta, GA, USA). The depression was a round, well-circumscribed radiolucency, corticated, and its maximal dimensions were 5.4×10×6.3 mm in the coronal, sagittal, and axial multi-planar reconstruction images (Figs. 2, 3, 4). Figure 3 presents a panoramic reconstruction of the CBCT volume showing the depression. In the axial cross sections, the well-defined lytic area was located on the posterior border of the ascending ramus on the lingual aspect (Fig. 5).
Based on the clinical and radiographic features of the lesion, a provisional diagnosis of a developmental salivary gland depression of the left ramus was made. The differential diagnosis included a static bone cavity, or a simple bone cyst, a benign tumor of salivary gland or fatty origin. Although we did not expect the defect to change in size over time, a clinical and radiographic follow-up was recommended to the patient. The patient was cleared for the extractions and was scheduled for annual follow-up.
Salivary gland related depression was first described by Stafne1 in 1942 as "the bone cavities situated near the angle of the mandible." These concavities came to be known as Stafne's idiopathic bone cavities, or Stafne's salivary gland depressions, and a host of various synonyms in the English literature. Over the years, this has become an established diagnosis as the relationship of the submandibular gland and the depression on the lingual surface of the mandible in the submandibular fossa has been studied using diagnostic modalities such as sialography. Based on this knowledge, we routinely diagnose this depression based on the location, anatomy, imaging and lack of consistent symptoms.
In this report, the occurrence of a depression similar to those reported by Stafne1 was discussed. This depression has developmental origins from the parotid salivary gland, fatty tissue, or blood vessels. In archeological studies, the occurrence of parotid-related depressions has been noted on the ascending ramus both on the buccal9 and lingual surfaces.10 The case presented by Mann and Shields10 was an archeological sample from their study of 6700 excavated dry mandibles. Lee et al.11 reported a case in Australia, in which the patient had mild hemifacial macrosomia type I, a hypoplastic right mandible and TMJ. Incidentally, his parotid salivary gland was enlarged (hypertrophic) and observed to be occupying part of the right ascending ramus. This was confirmed by multidetector CT and magnetic resonance imaging (MRI), as well as ultrasound-guided needle biopsy of the parotid tissue.11
Minowa et al.4 described 12 cases from Japan of static bone cysts as defined by Stafne, presenting at the angle of the mandible inferior to the mandibular canal, using CT and MRI. On non-contrast CT, they found fatty tissue occupying the static bone cavity in all 12 cases. Fatty tissue and blood vessels were found in 10 of the 12 cases, and fatty tissue with soft tissue that was not glandular in nature was found in the remaining 2 of the 12 cases. In 2012, Kim2 reported a multilocular developmental salivary gland defect appearing characteristically just above the inferior border of the mandible. Philipsen et al.12 questioned the role of the sole etiological factor (salivary gland inclusion) that has been proposed for the development of lingual mandibular depressions.
Barker3 utilized sialography to confirm that the parotid gland may also cause a bone cavity similar to Stafne's bone defect on the mandible. It was possible that the mandibular ramus concavity was merely the result of entrapment of the salivary glandular tissue and the growth of the mandible took place bypassing this portion of the gland to complete the ossification, hence the depression. In contrast, Wolf8 found that only 1 out of 6 cases described had any relationship with the parotid gland, with the gland in close contact with the bone at the condylar neck below the area of the attachment of the TMJ capsule.
During intrauterine development (around week 8), the anlage of parotid gland is found fairly close to Meckel's cartilage of the first pharyngeal arch, therefore, in close proximity to the developing mandible (Fig. 6).5 The gland arises from epithelial buds in the oral cavity and extends into the mesenchyme and its terminal ends of the solid cords, which eventually become the parotid duct, and ends near the developing facial nerve.5 Considering its close relationship to the mandible during early development, it has been proposed that the parotid gland becomes entrapped in the developing mandible, resulting in a type of bone cavitation and leading to a bone defect. This proposal is supported by some incidental findings in previous reports. Shields9 reported a bone defect on the mandibular ramus drawn from a study collecting and evaluating mandibular skeletal samples from throughout the world.
Another presentation reported by Campos et al.7 in Brazil found a cortical bone defect on the lingual aspect of the ascending ramus of a 14-year-old male. The CT imaging found that the lesion was covered by medial pterygoid muscle, and was not associated with the parotid gland. The authors questioned the possibility of the development of the defect from hyperplastic or hypertrophic submandibular gland, since contact between the gland and the angle was not possible due to the presence of medial pterygoid muscle in between. This further supports the idea that other factors might be responsible for the formation of these defects.
Parotid gland inclusion at the ramus of the mandible is rarely encountered and visualized using diagnostic imaging. From a clinician's standpoint, identifying the traditional Stafne's defect presenting inferior to the mandibular canal in the body of the mandible is critical for differential diagnosis and management. Similarly, the lesions in the ascending ramus might lead to a lot of concern among dental practitioners if the etiology of such a bony concavity is not clearly known. Based on our report, multiple hypotheses can be made. First, fatty tissue, blood vessels, or soft tissue from the parapharyngeal space might be trapped during the intramembranous ossification of Meckel's cartilage due to the proximity of the gland during its development to Meckel's cartilage. This has been proven by many authors who used CT, MRI, and sialography to verify the contents of the bone cavities found. Second, soft tissues including fat and blood vessels from the parapharyngeal space in the stylomandibular tunnel may be able to grow into a hypoplastic mandibular concavity that was developmentally formed prior to the entrapment of soft tissues. Third, parotid gland inclusion in the ascending ramus may cause a depression and might even lead to perforation of the buccal or lingual cortex depending on the direction of the parotid gland entrapment.
We studied the defect using only CBCT imaging results. The differential diagnosis included, but was not limited to, a developmental salivary gland defect, fatty tissue deposition, blood vessels and soft tissue deposition, traumatic bone cyst, aneurysmal bone cyst, and hypertrophy as well as lipomas and other benign tumors of the salivary gland. However, tumors often present with symptoms such as pain, swelling and paresthesia and motor deficiency (cranial nerve VII), especially if they involve the parotid gland.
Based on the location, presentation, age, and gender of the patient, we concluded that this was a rare occurrence of a developmental mandibular depression noted in the ascending ramus that might be related to the parotid gland, blood vessels, fatty tissue, or most likely a combination of both fatty tissue and blood vessels. Three such cases have been previously reported in the literature.3711
Sialography may be considered owing to the proximity of the parotid gland to the lesion, and may be recommended especially in the presence of glandular swelling. Other, more invasive studies include aspiration to exclude a vascular lesion, CT, or MRI-guided biopsy.
Figures and Tables
 | Fig. 2A cone-beam computed tomography panoramic reconstruction and coronal multi-planar reconstructed slice show the well-corticated depression in the ramus. Note the lingual location of the concavity. |
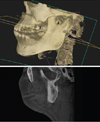 | Fig. 3A cone-beam computed tomography 3-dimensional reconstruction of the mandible and maxilla shows the lingual depression through the thinned or perforated buccal aspect of the left mandibular ramus (top). A sagittal reconstructed slice of the left side shows the details of the concavity (bottom). |
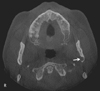 | Fig. 4An axial cone-beam computed tomography reconstruction showing thinning of the buccal cortex and the lingual location of the depression on the left ramus (arrow). |
 | Fig. 5An axial cone-beam computed tomography slice of a 3-dimensional reconstruction with soft tissue overlay and coloration shows the posterior and lingual location of the concavity within the left ramus. The short arrow points to the lingual concavity and the long arrow points to the left styloid process. Note that the stylomandibular tunnel is the space between the styloid process and the ramus of the mandible, which is immediately adjacent to the parotid gland. |
References
1. Stafne EC. Bone cavities situated near the angle of the mandible. J Am Dent Assoc. 1942; 29:1969–1972.

3. Barker GR. A radiolucency of the ascending ramus of the mandible associated with invested parotid salivary gland material and analogous with a Stafne bone cavity. Br J Oral Maxillofac Surg. 1988; 26:81–84.

4. Minowa K, Inoue N, Sawamura T, Matsuda A, Totsuka Y, Nakamura M. Evaluation of static bone cavities with CT and MRI. Dentomaxillofac Radiol. 2003; 32:2–7.

5. Guizetti B, Radlanski RJ. Development of the parotid gland and its closer neighboring structures in human embryos and fetuses of 19-67 mm CRL. Ann Anat. 1996; 178:503–508.

6. Carlson GW. The salivary glands. Embryology, anatomy and surgical applications. Surg Clin North Am. 2000; 80:261–273.
7. Campos PS, Panella J, Crusoe-Rebello IM, Azevedo RA, Pena N, Cunha T. Mandibular ramus-related Stafne's bone cavity. Dentomaxillofac Radiol. 2004; 33:63–66.

8. Wolf J. Bone defects in mandibular ramus resembling developmental bone cavity (Stafne). Proc Finn Dent Soc. 1985; 81:215–221.
9. Shields ED. Technical note: Stafne static mandibular bone defect-further expression on the buccal aspect of the ramus. Am J Phys Anthropol. 2000; 111:425–427.

10. Mann RW, Shields ED. Cavitation defects on the lingual ramus: a further expression of Stafne's defect. J Craniofac Genet Dev Biol. 1992; 12:167–173.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download